Nodular melanoma is a type of skin cancer. It’s a firm, raised, discolored growth on your skin that may look like a blood blister. Overexposure to ultraviolet light is the primary cause of nodular melanoma. It exists in four stages.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
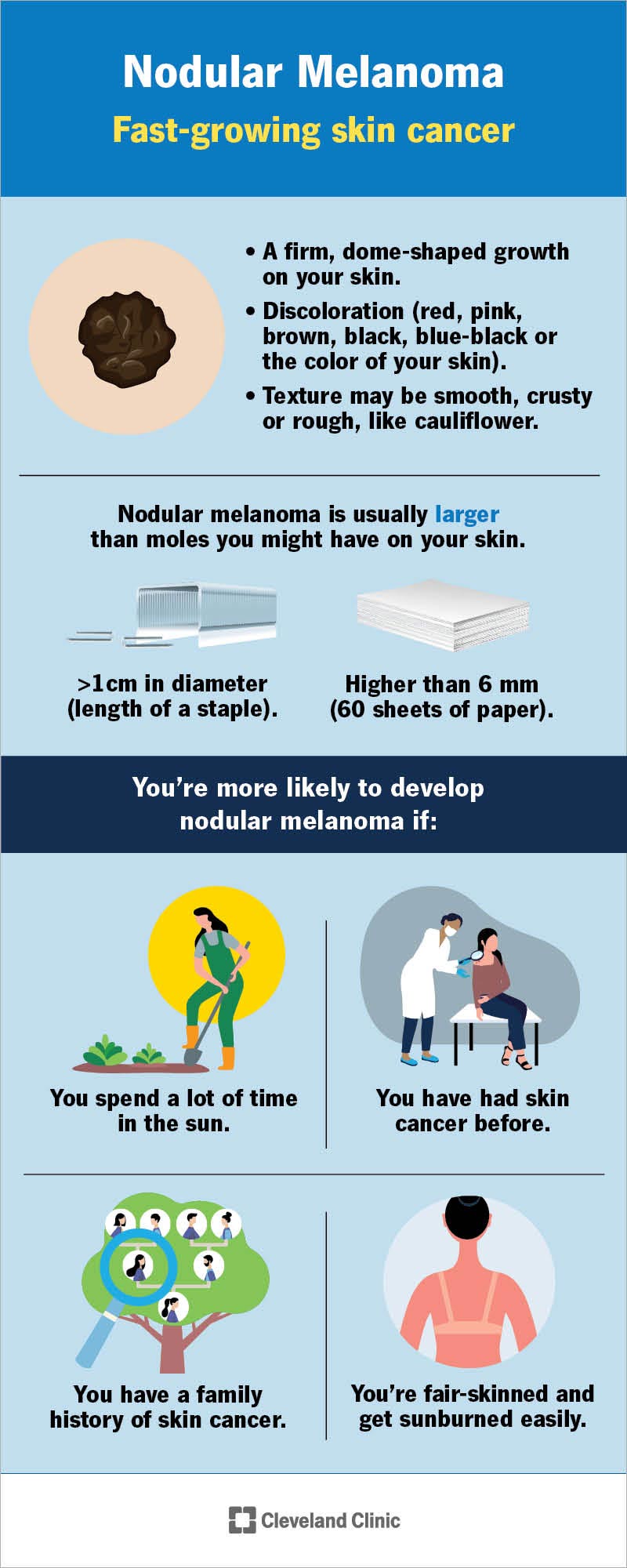
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/23313-nodular-melanoma)
Nodular melanoma is a type of melanoma. It’s a type of skin cancer that develops very quickly, usually growing rapidly over several weeks or months. It grows above and below your skin (vertically), but most of the cancer is below the surface, like an iceberg.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Healthcare providers group nodular melanoma in the following stages:
Anyone can develop nodular melanoma. But you’re more likely to have it if you’re a man and over 50 years old.
You’re also more likely to develop nodular melanoma if:
Nodular melanoma is the second-most common type of melanoma. Approximately 15% to 20% of all melanoma diagnoses are nodular melanoma. It causes about 50% of all melanoma-related deaths.
Advertisement
Nodular melanoma can develop anywhere on your body. However, it usually develops in places that are the most exposed to sunlight, including your:
Nodular melanoma is usually larger than moles you might have on your skin. They’re generally greater than 1 centimeter in diameter, which is about the length of a staple, and higher than 6 millimeters, which is about the height of 60 sheets of paper.
Symptoms of nodular melanoma include:
Yes, nodular melanoma can look like a blood blister.
Blood blisters develop after something pinches your skin. Blood flows to the area from broken blood vessels and damage to the lower layers of your skin. The blood pools and forms a raised blister, which may look brown, red, black or the same color as your skin.
Yes, nodular melanoma may bleed if you poke, scratch or squeeze it. It may also bleed without agitation.
Nodular melanoma is usually hard or firm to the touch.
The biggest risk factor for developing nodular melanoma is overexposure to ultraviolet (UV) light, especially sunburns.
Your skin contains melanocytes (pronounced “mel-ann-o-sites”). Melanocytes produce melanin, which provides the color (pigment) in your skin. UV exposure from the sun (solar) or tanning beds can cause the DNA in your melanocytes to change. The melanocytes grow and divide uncontrollably and invade nearby tissues (malignancy).
No, nodular melanoma isn’t contagious. You can’t give nodular melanoma to another person.
Your healthcare provider will perform a physical examination of the growth, the skin around your growth and your lymph nodes. They’ll touch (palpate) your growth and may ask a few questions, including:
After a physical examination, your healthcare provider may perform a biopsy to confirm their diagnosis. They’ll numb the area so you don’t feel any pain. They may remove a small amount of the growth, or they may remove most or all of it. Then, they’ll send the growth sample to a laboratory so other healthcare providers can test it for cancer cells. You should get the results of your biopsy in two to 10 days.
Advertisement
Nodular melanoma treatment depends on the stage and your general health. The priority is to cure your cancer, but your healthcare providers also want to stop your cancer from coming back and maintain your skin’s appearance.
Often, surgery is the first treatment for early-stage nodular melanoma. Depending on your melanoma type, you may have local numbing and be awake during the procedure, or you may be sedated (put under) with general anesthesia during surgery.
Once you’re either numbed or asleep, a dermatologist or surgeon will use a sharp, thin knife (scalpel) to remove the nodular melanoma and some of the healthy skin and tissue surrounding the growth.
If you have late-stage nodular melanoma, the cancer has spread to other parts of your body. In addition to surgically removing the nodular melanoma, additional treatments may include a combination of:
Advertisement
It depends on your treatment.
After surgery, your skin should heal in one to three weeks.
After chemotherapy and targeted cancer therapy, most side effects go away after stopping treatment.
Early diagnosis is extremely important if you have nodular melanoma. When diagnosed in its early stages, your prognosis is good.
However, nodular melanoma grows quickly, and late-stage nodular melanoma can be fatal. Your chances for a full recovery are better the sooner it’s diagnosed and removed.
The following survival rates reflect the percentage of people who are still alive five years after receiving a nodular melanoma diagnosis and treatment:
The following tips can help reduce your risk of getting nodular melanoma:
Advertisement
See your healthcare provider if you have any of the following:
No, you can’t scratch off nodular melanoma. The cancer will continue to spread, and you may cause an infection.
Receiving a nodular melanoma diagnosis can be scary and frustrating. It’s a good idea to pay attention to your skin, especially if you’re fair-skinned or spend a lot of time in the sun. If you notice any changes, reach out to your healthcare provider immediately. They can help you understand your treatment options and what to expect, which can help ease any anxiety.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.