Acne keloidalis nuchae (AKN) is a skin disorder involving inflammation of the hair follicles on your neck and back of your scalp. It causes red patches on your skin, which can develop into papules, plaques, pustules, infections, scarring and hair loss. AKN is most common among men with curly hair.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
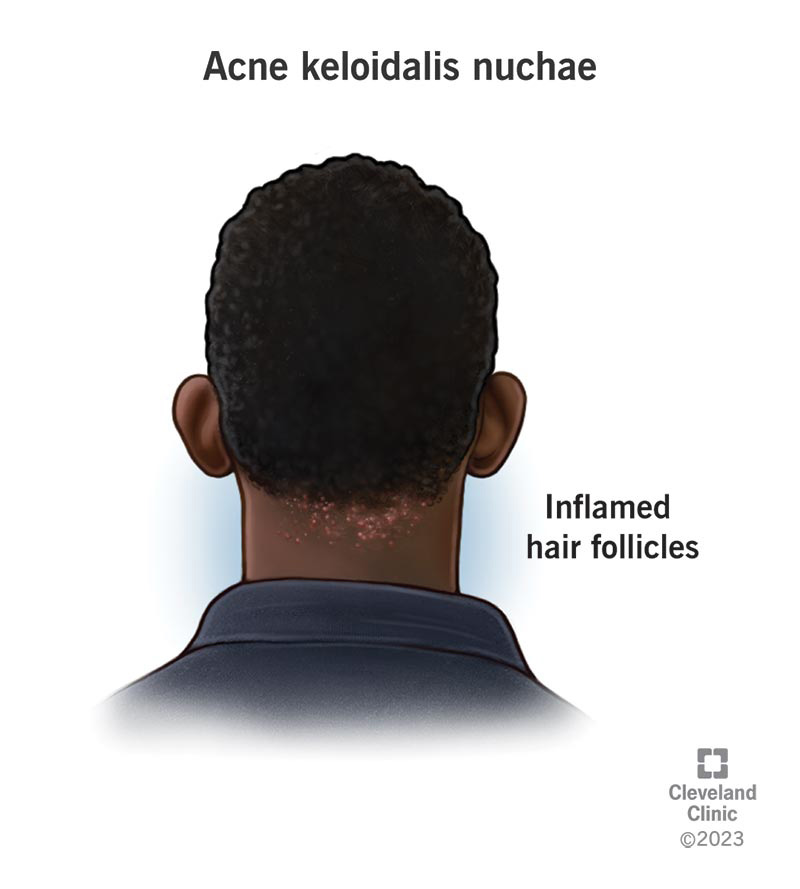
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22891-acne-keloidalis-nuchae)
Acne keloidalis nuchae (AKN) is a type of folliculitis, which is inflammation of your hair follicles. The chronic disorder affects the follicles on the back of your neck and back of your scalp, the skin covering your head where hair grows.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
AKN can cause progressively worsening skin problems in the area, which may lead to scarring and hair loss.
The condition is also called:
Anyone can develop this type of folliculitis. But it’s much more common in men with curly hair. It usually starts after adolescence.
Scientists aren’t sure what causes AKN, but some believe it might be due to:
The condition usually begins with red, itchy bumps (papules) or patches of skin. The papules tend to get infected because of scratching, leading to pustules (pockets of pus, almost like pimples).
Over time, AKN progresses to inflamed, thickened and scarred areas of skin (fibrosis, hypertrophic scars and keloids). Episodes of inflammation can range from mild to severe.
Symptoms may include:
Advertisement
There aren’t perfect tests to diagnose acne keloidalis nuchae. A healthcare provider can diagnose the condition based on a physical exam of the neck and scalp. The healthcare provider will also ask about:
If the diagnosis isn’t clear, your healthcare provider may recommend a biopsy. The test takes a small sample of your skin so an expert can look at the cells under a microscope to help diagnose and treat the condition.
If the skin lesions seem to be infected, then your healthcare provider might order a culture. That’s a test to determine the type of infection. A culture can help decide what treatment can clear the infection.
There isn’t a cure for the condition, so treatment usually involves medications to ease symptoms, such as:
If acne keloidalis nuchae becomes severe, your healthcare provider may suggest surgical excision and skin grafting. This involves cutting away damaged portions of skin and replacing them with healthy patches of skin from somewhere else on your body.
Researchers are testing other ways of treating the condition, including laser therapy, phototherapy, laser hair removal and radiotherapy (only for cases that are resistant to all other treatments).
AKN is a chronic condition without a cure, so it often lasts a lifetime. The goal of treatment is to manage symptoms, prevent infection and slow the progression of AKN.
Because scientists don’t yet understand what causes AKN, there aren’t any proven ways to prevent it. Certain measures, like avoiding irritation and close shaving, may reduce symptoms and help prevent AKN development.
Certain strategies may help ease symptoms and prevent infections:
You should talk to your healthcare provider anytime skin problems are bothering you or interfering with your life.
With AKN, your skin is at risk for infection. Seek medical attention if you have any signs, such as:
Advertisement
Acne keloidalis nuchae (AKN) is a type of folliculitis, or inflammation of your hair follicles. It causes lesions on the skin of your neck and back of your scalp. AKN can worsen over time, leading to scarring and hair loss. Although there isn’t a cure, your healthcare provider can help ease symptoms and prevent infection and progression.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Every day, people see your skin, hair and nails. At Cleveland Clinic, our expert and caring dermatology team will make sure they’re healthy and strong.
