Beckwith-Wiedemann syndrome (BWS) is a genetic overgrowth disorder that can affect many different parts of your child’s body. Most babies are large at birth and have other symptoms across a wide spectrum. BWS also increases your child’s risk for developing certain childhood cancers. BWS can’t be cured, but there are many treatments available.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
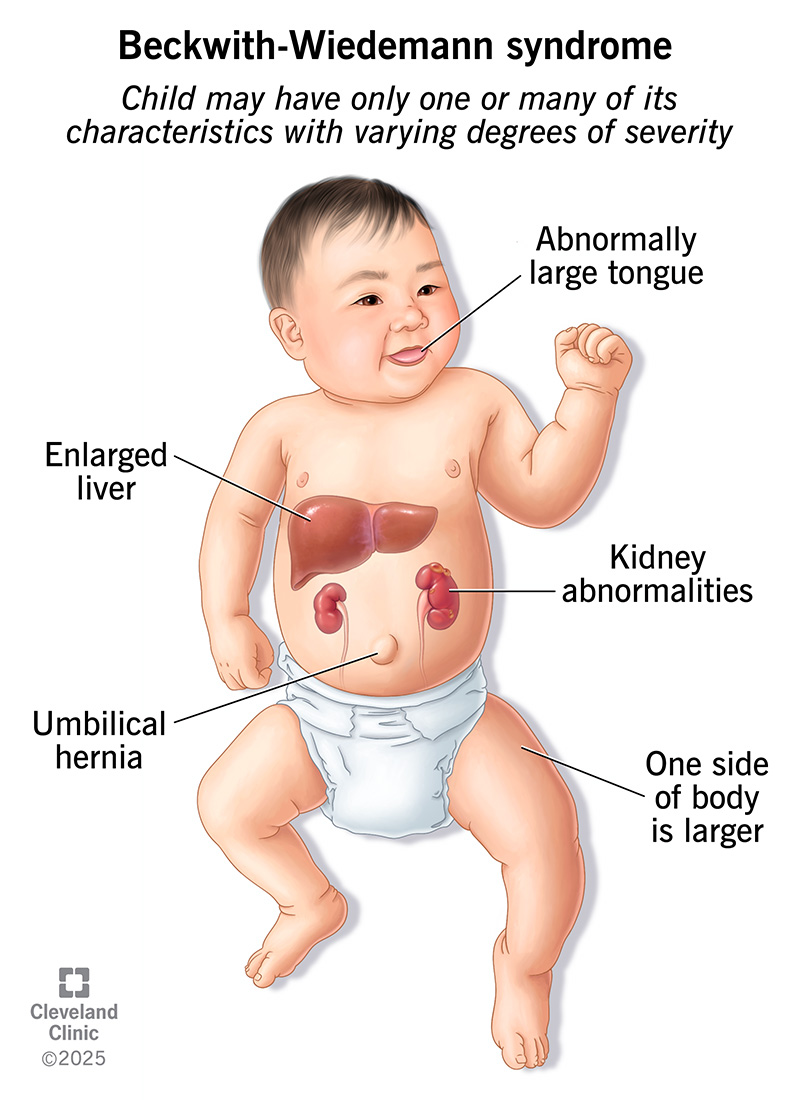
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/beckwith-wiedemann-syndrome.jpg)
Beckwith-Wiedemann syndrome (BWS) is a rare genetic disorder that affects your child’s growth. Most babies with BWS are larger than normal (macrosomia). Some may be taller than other children their age. But your child’s growth should slow down by the age of 8. They should be of average height in adulthood.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
BWS is also known as Beckwith-Wiedemann spectrum. This is because the symptoms and their severity vary widely. The condition can affect many different parts of your child’s body. Your child may have only one or many of its characteristics. Beckwith-Wiedemann syndrome also increases your child’s risk of developing certain childhood cancers.
There’s no cure for Beckwith-Wiedemann syndrome. But there are many treatments available to correct physical differences and relieve your child’s symptoms. BWS usually doesn’t cause any serious medical issues. Life expectancy is typically normal.
Beckwith-Wiedemann syndrome symptoms can vary widely from child to child. Characteristics that your child may have include:
Overall, children with BWS have about a 7.4% chance of developing cancer, with almost all of the risk increased between birth and the age of 8. These cancers include:
Advertisement
The causes of Beckwith-Wiedemann syndrome are complex. Researchers link most cases of BWS to certain epigenetic changes on chromosome 11. These changes affect the normal expression of genes on the portion of chromosome 11 (11p15.5) that controls growth. This is called genomic imprinting.
About 85% of children born with Beckwith-Wiedemann syndrome don’t have a biological family history of the condition. Instead, the epigenetic changes happen randomly.
About 10% to 15% of children have a family history of Beckwith-Wiedemann syndrome. That means one parent passed down a genetic change that causes BWS.
Unknown causes lead to the diagnosis in about 14% to 20% of children born with the condition.
Research into the cause of Beckwith-Wiedemann syndrome shows that people who use assisted reproductive technology (ART) to conceive may have a higher risk of having a baby with a genomic imprinting disorder like BWS. These ART procedures include in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI). Scientists have to do more research to find the connection.
In addition, studies suggest that BWS is more common in twin pregnancies than in pregnancies with just one fetus.
Beckwith-Wiedemann syndrome can lead to preterm labor. After your baby is born, they can develop breathing and feeding difficulties, low blood sugar (hypoglycemia) and cardiomyopathy.
Complications that can occur from childhood through adulthood include:
Your healthcare provider may be able to diagnose Beckwith-Wiedemann syndrome before birth. Using a prenatal ultrasound, they can detect features of the condition, including:
If the ultrasound reveals potential signs of BWS, your provider can use prenatal genetic tests to confirm a diagnosis. These tests include amniocentesis and chorionic villus sampling.
After birth, your provider can diagnose or confirm the condition with a physical examination and genetic testing.
Beckwith-Wiedemann syndrome can affect many different parts of your child’s body. Because of this, you’ll work with many healthcare providers and specialists to address the specific symptoms and conditions affecting your child.
Advertisement
Macroglossia, or an enlarged tongue, is a common feature of BWS. A larger tongue size can cause sleeping, feeding and speaking issues. So, providers may use various treatments, including:
Other Beckwith-Wiedemann syndrome treatment options may include:
Your provider may also recommend genetic counseling for you and your family to help you learn more about your child’s condition.
You and your child will work with a team of healthcare providers to help manage your child’s condition. Your child will need regular check-ups so their providers can monitor their symptoms. Alert your child’s provider about any new or worsening symptoms.
Advertisement
All children with BWS have a higher risk of developing childhood cancers. They’ll need routine cancer screenings so their healthcare provider can find and treat cancer before it spreads.
Beckwith-Wiedemann syndrome is a complex condition that can affect your child in many ways. The prognosis for your child depends on many factors, including:
Early diagnosis and treatment, along with routine cancer screenings, can lead to the best outcome. Most children who develop Beckwith-Wiedemann syndrome have a normal life expectancy.
It may have come as a shock to learn that your child has Beckwith-Wiedemann syndrome (BWS). Their diagnosis may have left you with lots of questions about what this means for your child’s health. BWS can’t be cured. But medical treatments can help resolve most of your child’s symptoms. Ask your child’s healthcare provider what medical challenges your child may face. They’ll have insight into your child’s specific situation. That way, you can understand how BWS may affect your child and what you can do to help them thrive.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Do certain health conditions seem to run in your family? Are you ready to find out if you’re at risk? Cleveland Clinic’s genetics team can help.
