Dry socket is a painful condition that can happen after a dentist pulls a tooth. It occurs when the blood clot doesn’t form or gets knocked loose, exposing the bone and nerves. This can delay healing, but your dentist can help ease symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
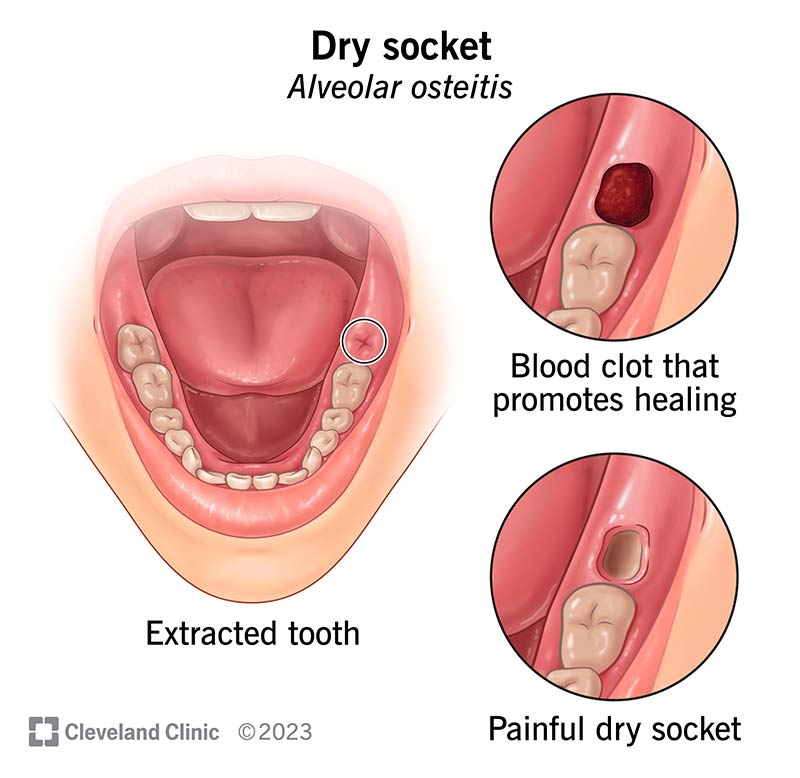
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/17731-dry-socket)
Dry socket (alveolar osteitis) can happen after you get a tooth pulled. Normally, a blood clot forms in the empty space (called a socket) where the tooth used to be. This clot protects the area and helps it heal.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
If the clot doesn’t form — or if it comes out too soon — the bone and nerves underneath can get exposed. That can cause a lot of pain and slow down healing.
Dry socket affects about 2% to 5% of all tooth extractions. It’s more common after wisdom teeth removal.
A dry socket looks like an empty hole where your tooth was, with a whitish layer at the bottom. That white part? It’s exposed bone. That’s why you’re feeling so much pain.
After your dentist pulls the tooth, a blood clot forms in the socket — that’s a good sign. It looks like a dark scab and protects the area while it heals. If you notice the clot, leave it alone and don’t try to touch or remove it. If you don’t see a clot — or if you see bone instead — you might have a dry socket.
Dry socket symptoms may include:
A dry socket happens when a blood clot at the site of a tooth extraction breaks down too soon or doesn’t form properly. This clot is essential — it protects the bone and nerves underneath as the area heals. But in some cases, the clot dissolves or dislodges early, exposing the bone and causing pain.
Advertisement
Researchers still don’t know exactly why this happens in some people and not others. However, they’ve identified several risk factors that can increase your chances of developing a dry socket.
These things can raise your risk for dry socket:
Dry socket treatment may include:
With proper care, a dry socket usually heals within seven to 10 days. In that time, new tissue forms to cover the exposed area. Brushing and flossing regularly helps keep your mouth healthy and lowers your risk of infection.
Let your dentist know if you’re having pain that keeps you up at night or doesn’t improve with medication. If you can’t reach the provider who did the extraction, head to the nearest urgent care or emergency room.
Most dry sockets heal on their own, but the pain can be intense. If you’re dealing with moderate to severe discomfort, it’s a good idea to see your dentist. Prompt treatment can help relieve the pain and speed up healing.
Dry socket usually develops within the first three days after your dentist removes a tooth. If you haven’t had symptoms by day five, you’re likely in the clear.
You can’t always prevent dry socket, but you can lower your risk. Here’s how to protect the healing spot after a tooth extraction:
Advertisement
Taking these steps helps your mouth heal and keeps discomfort to a minimum.
If you recently had a tooth removed and are experiencing severe discomfort, it could be dry socket. Dry socket can be very painful, so don’t wait. See your dentist at the first sign of trouble. The good news: It usually heals within a week. In the meantime, your dentist can help you manage the pain and stay comfortable as you heal.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Dentistry plays an important role in oral health. Cleveland Clinic’s experts can design a personalized plan that will keep you smiling for the long haul.
