Asherman’s syndrome is the formation of scar tissue inside your uterus. It most often develops after uterine procedures, like a dilation and curettage (D&C). Asherman’s syndrome can cause pelvic pain, irregular periods and infertility. The main treatment is removal of the scar tissue.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
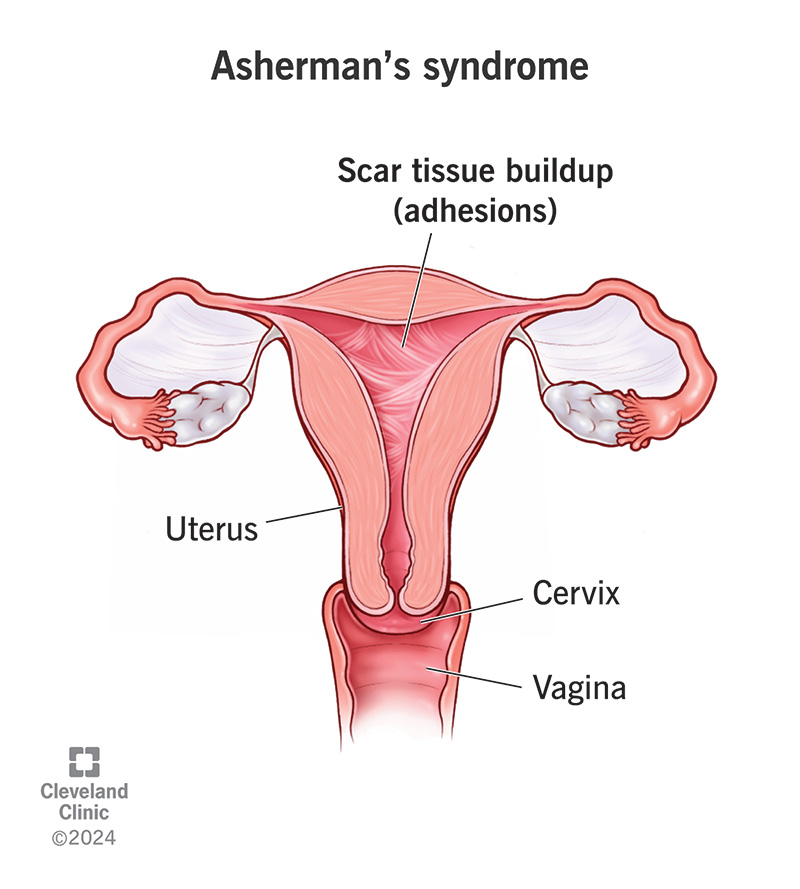
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16561-ashermans-syndrome)
Asherman’s syndrome happens when scar tissue (adhesions) builds up inside your uterus and/or cervix. It most often develops after procedures that remove tissue from your uterus. Your healthcare provider may call Asherman’s syndrome “intrauterine adhesions” or “intrauterine synechiae.”
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The extra scar tissue creates less space inside your uterus. Think of the walls of a room getting thicker and thicker, making the space in the middle of the room smaller. These changes can cause pain, irregular periods and infertility.
Maybe you’ve noticed that your periods have changed after a dilation and curettage (D&C). Or you have more pelvic pain than usual. You know what’s not normal for you. If you think you might have Asherman’s syndrome, reach out to a healthcare provider.
Symptoms of Asherman’s syndrome can include:
You may not have a period but feel pain at the time you’d expect your period. This may mean that menstruation is happening. But the blood can’t leave your uterus because it’s blocked by scar tissue.
In some cases, you may not experience any symptoms of Asherman’s syndrome.
Asherman’s happens when the basal layer of the endometrium (uterine lining) is traumatized or removed in opposing parts within your uterus. Inflammation in those areas causes a scar to form. This most commonly happens after medical removal of tissue inside your uterus.
Advertisement
Researchers tend to group the causes of Asherman’s syndrome into two groups: pregnancy-related and not pregnancy-related.
Researchers estimate that more than 90% of cases of Asherman’s syndrome happen after pregnancy-related dilation and curettage (D&C). You may have gotten a D&C for:
Researchers have found that a recently pregnant uterus seems to be sensitive to damage (trauma) of the endometrium. This is the tissue that lines your uterus. Damage to the endometrium shortly after a pregnancy can cause scar tissue to form.
In very rare cases, a cesarean section (C-section) may cause Asherman’s syndrome.
Less often, Asherman’s syndrome results after a D&C for procedures not related to pregnancy, like:
It can also develop after operative hysteroscopy for:
Other causes include:
Other than having uterine procedures in general, factors that increase your risk for Asherman’s syndrome include having:
Your healthcare provider will consider your symptoms and medical history. If you’ve had surgeries or procedures that can cause Asherman’s syndrome, they’ll likely recommend tests that can help diagnose it.
Diagnostic hysteroscopy is the go-to test for diagnosing Asherman’s syndrome. Your provider inserts a thin, lighted camera in your vagina and through your cervix. This allows your provider to thoroughly examine your cervix and the inside of your uterus. They can evaluate the severity of the scar tissue.
A pelvic ultrasound or transvaginal ultrasound may also help diagnose Asherman’s syndrome. Your provider may do a transvaginal ultrasound with saline infusion. For this procedure, your provider inserts a saline solution (a mixture of salt and water) into your uterus. The fluid expands your uterus. Your provider can then see the details of the shape of your uterine cavity with ultrasound.
Researchers have several classification systems to describe the severity of Asherman’s syndrome. One example is from the American Fertility Society. It classifies the severity of the syndrome as follows:
Advertisement
Your healthcare provider may use different descriptions. Don’t hesitate to ask questions if something is unclear.
You have a few options to treat Asherman’s syndrome. The main goal of treatment is to remove the scar tissue and restore the inside of your uterus. Treatment for Asherman’s syndrome can help:
Make sure to discuss with your healthcare provider how this condition makes you feel and your goals for future fertility. If you don’t have pain and aren’t trying to get pregnant, you may not need any treatment.
Operative hysteroscopy is the go-to treatment for Asherman’s syndrome. During the procedure, your provider inserts a thin, lighted camera in your vagina and through your cervix to look inside your uterus. The tool also has very thin scissors or a laser that carefully and precisely removes scar tissue.
Advertisement
You may need more than one operative hysteroscopy to treat Asherman’s syndrome.
The biggest concern with getting an operative hysteroscopy is scar tissue forming again afterward.
To try to prevent this, your provider may:
If you get a barrier in your uterus, you’ll take antibiotics to prevent an infection. Your provider will likely recommend a follow-up appointment one or two weeks after the hysteroscopy to check on your uterus. This may allow your provider to catch new scar tissue while it’s still small. They can remove it before it gets worse.
If you have symptoms of Asherman’s syndrome and don’t want future pregnancies, your provider may recommend a hysterectomy. They’ll remove your uterus, but you’ll likely keep your ovaries.
Researchers are currently studying if stem cell therapy or platelet-rich plasma can help rebuild the endometrium in cases of Asherman’s syndrome. You might be able to participate in a clinical trial on this treatment technique.
Advertisement
Your prognosis (outlook) varies depending on:
If treatment for Asherman’s syndrome is successful, your symptoms should get better. Most people get their periods back after up to three hysteroscopic procedures. But improvement in fertility is more difficult for researchers to study.
Over time, your healthcare provider will want to monitor your condition to check if you’ve developed additional scar tissue.
It depends. The chances of getting and staying pregnant after treatment are lower for people with moderate to severe Asherman’s syndrome.
One study revealed that:
Infertility can be tricky because the cause isn’t always easy to find — and there can be more than one cause. If your provider has diagnosed Asherman’s syndrome as the main cause of your infertility, treating it can help improve your chances of carrying a pregnancy to birth.
Asherman's syndrome can result in recurrent pregnancy loss despite surgery and treatment.
It can also cause pregnancy complications, including:
Your healthcare provider will carefully monitor your pregnancy if you have Asherman’s syndrome.
The scar tissue that develops in Asherman’s syndrome can be a possible side effect of several medical procedures. Often, these procedures are necessary. So, you can’t always prevent Asherman’s syndrome.
It’s important to talk to your healthcare provider about all possible risks of a medical procedure beforehand. Your provider may schedule follow-up appointments after a procedure to check for any scar tissue. They’ll keep an eye on the possible development of Asherman’s syndrome.
Some questions to ask your healthcare provider about Asherman’s syndrome include:
It’s difficult for researchers to tell how rare Asherman’s syndrome is. It can go undiagnosed if you’re not trying to get pregnant. Researchers also think it’s underdiagnosed, as routine exams and procedures typically don’t spot it.
Getting an Asherman’s syndrome diagnosis may change what you thought your future would look like. For some people, having Asherman’s syndrome may require additional effort to manage painful periods. For others, it may mean rethinking pregnancy plans. Although everyone’s situation is different, you don’t have to manage this condition alone. Your healthcare provider will be by your side to help you reach your treatment goals. It may take time, but treatment is possible. Also, lean on loved ones and support groups to relate to others living with Asherman’s syndrome.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
From routine pelvic exams to high-risk pregnancies, Cleveland Clinic’s Ob/Gyns are here for you at any point in life.
