The oculomotor nerve is a cranial nerve pair that carries eye muscle command signals. These nerves handle most of the signals that tell your eyes how and when to move. When these nerves work properly, they help you see and contribute to many abilities. Conditions affecting your oculomotor nerve can disrupt your vision and cause other issues.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
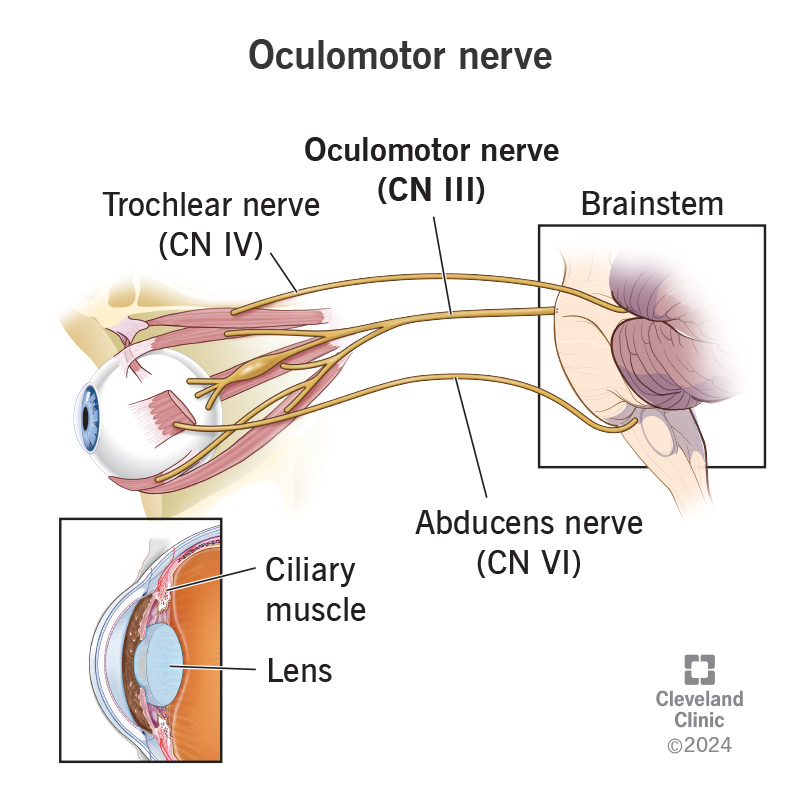
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/oculomotor-nerve)
The oculomotor nerve is one of the main nerves you use to control how your eyes move. Its branches connect to muscles on multiple sides of your eyeballs, delivering movement commands from your brain to those muscles.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Despite its name sounding like it’s for one nerve, it’s a paired set, one for each eyeball. The oculomotor (pronounced “OCK-yoo-lo-mo-tor”) nerve pair is the third of the 12 pairs of cranial nerves, named because they directly connect to your brain. Experts also refer to this nerve using the abbreviation and Roman numeral combination “CN III.”
The oculomotor nerve is one of three cranial nerve pairs that play a role in eye movement, and the oculomotor nerve does the most out of all three. Seven different muscles in and around each eye rely on the oculomotor nerve for the signals that tell them what to do.
The oculomotor nerve lets you do the following:
The only two movements that the oculomotor nerve doesn’t control are:
Advertisement
Because your vision plays a major role in many abilities and processes, your oculomotor nerves have to work seamlessly with several other systems. When they do, you have the following abilities:
Your oculomotor nerve is vulnerable to the same conditions as any other nerve. And because it runs through various brain areas, certain brain conditions can affect this nerve, too.
When the oculomotor nerve doesn’t work correctly, it’s known as oculomotor nerve palsy (sometimes “third nerve” replaces “oculomotor”) or dysfunction. Many things can cause oculomotor nerve dysfunction.
Examples include:
Advertisement
Oculomotor nerve-related symptoms include:
Taking care of your oculomotor nerve health is much like caring for your whole body. Some things you can do include:
The oculomotor nerve is a nerve pair that carries commands from your brain to muscles in and around your eyes. When the oculomotor nerve works correctly, it’s easy not to think about it. But when it doesn’t work properly, it’s understandable to feel confusion or anxiety.
If you think you have a problem with eye movement control or the oculomotor nerve, talk to an eye care specialist. They can look and test for issues that could explain your symptoms and offer treatment options.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Getting an annual eye exam at Cleveland Clinic can help you catch vision problems early and keep your eyes healthy for years to come.
