A peak flow meter is a simple, easy-to-use device that measures how fast you can exhale a lungful of air. It helps manage asthma and can even indicate when your asthma is getting worse before you have symptoms. Use your peak flow meter at least once a day or as directed by a healthcare provider.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
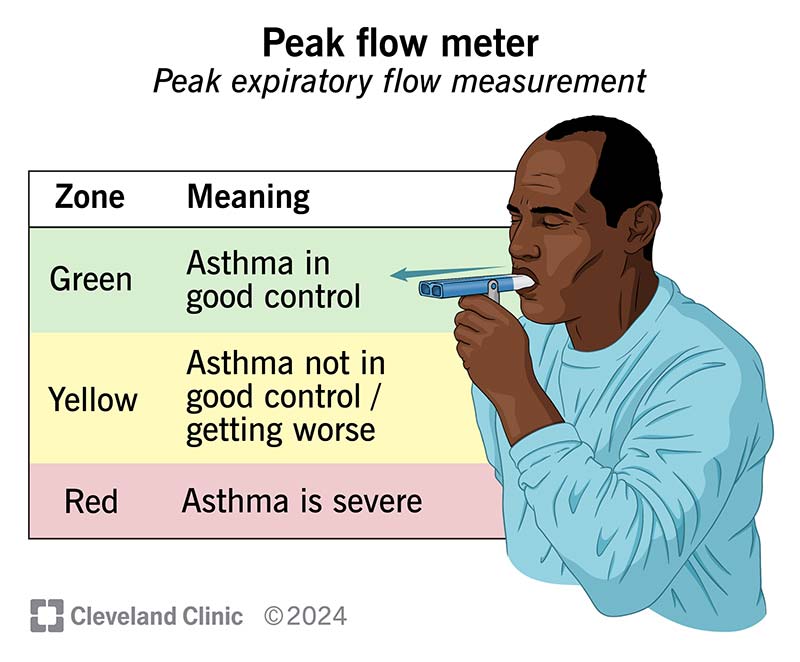
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/peak-flow-meter)
A peak flow meter is a small, handheld device that measures how fast you can push air out of your lungs when you blow out (exhale) as hard and as fast as possible. This is your peak flow. Another name for peak flow is peak expiratory flow measurement.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
There are manual and digital peak flow meters. A manual peak flow meter has markers on the device that you use to track your peak flow. A digital peak flow meter displays your peak flow on a screen.
Peak flow meters come with a chart with average readings. It’s important to remember that you don’t need to aim for these numbers — they’re just an average.
A peak flow meter helps manage moderate to severe asthma. It measures how open the airways (bronchi) are in your lungs. Your peak flow may drop, even before you have an asthma attack. A drop in your peak flow tells you that your asthma might be getting worse.
A peak flow meter is simple to use. To measure your peak flow:
Advertisement
Repeat these steps three times. The highest of these three readings is your daily peak flow. Write down your daily peak flow on a sheet of paper, on your calendar, in your smartphone or in your asthma diary. You should also record:
A peak flow meter measures liters per minute (L/min).
Your personal or usual best peak flow is the highest number you can achieve over a two-week period while your asthma is under good control. “Good control” means you feel good and don’t have any symptoms. You’ll compare your other peak flow readings to your best peak flow number.
To find your personal best peak flow:
Once you determine your personal best peak flow, continue using your peak flow meter daily or as instructed by a healthcare provider. Regularly using your peak flow meter will help you recognize decreases in your airflow early. This can help guide your asthma treatment. A provider may use these numbers to create an asthma action plan to help manage your symptoms.
It depends. Your “normal” peak flow may differ from another person’s “normal” peak flow. A healthcare provider will help determine your normal peak flow according to your:
Healthcare providers generally use a “traffic light” system that consists of three zones to determine your peak flow rate:
To find the number ranges for your zones, multiply your personal best peak flow by:
Record these ranges so you can reference them quickly. For example, if your personal best peak flow is 400 L/m, the zones will be:
If you’re in the yellow or red zones, you must adjust your medicine according to your healthcare provider’s instructions. Use the peak flow values and your symptoms to take action, if necessary. If you have an asthma action plan, make sure you understand and can follow it. Ask a healthcare provider if you have any questions.
Advertisement
Your peak flow will vary according to your age, height and sex. Peak flow numbers are usually higher in people who are younger, taller or male.
A normal peak flow in adults may be between 400 and 700 L/m. In children, a normal peak flow may range from around 150 to 450 L/m. Be sure to keep track of your peak flow readings. A healthcare provider can use this information to observe your numbers over time and determine if your results are changing.
If your peak flow is in the yellow or red zones, immediately use your rescue inhaler or other emergency medications. If your peak flow doesn’t improve, call a healthcare provider immediately or go to the nearest emergency room.
It depends. A reading of 250 L/m may be good for some people but not others. Talk to a healthcare provider if you have questions about your peak flow meter readings.
Measuring your peak flow can help you:
In general, a peak flow meter is safe and easy to use. However, risks may include:
Advertisement
You also run the risk of getting an inaccurate reading if you take asthma medication before you use a peak flow meter.
Using the same peak flow meter is important to get the most accurate measurements. Different peak flow meter brands may use different measurements.
If your peak flow is in the yellow zone, call a healthcare provider immediately and take asthma medications. If it’s in the red zone, take rescue medicine right away and call a provider or get to the nearest emergency room if your symptoms don’t improve.
A spirometer is a machine that measures lung capacity. That means the amount of air you can inhale into, and exhale out of, your lungs. A peak flow meter measures how fast you can push air out of your lungs.
A peak flow meter helps you manage asthma and recognize changes in how well you’re breathing. It may be challenging to know if you’re using it correctly. A healthcare provider will demonstrate how to use it and ensure you use it properly. It’ll give you a good idea of your average peak flow. Your numbers may vary a little bit. But if there are any significant drops in your numbers, use your rescue inhaler or any other medications and call a healthcare provider immediately or get emergency care.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Breathing issues can affect your life in many ways. Cleveland Clinic’s respiratory therapy program treats your symptoms so you can feel better day to day.
