“Dementia” is a term for a group of symptoms that cause a loss of cognitive functioning (thinking, memory, mood and behavior). The decline interferes with your daily life and activities. It usually affects people after age 65. Medications may help slow the progression of symptoms. Dementia can shorten your life expectancy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Dementia involves a decline in the mental abilities you need for daily living. It develops when there’s damage to the parts of your brain involved with learning, memory, decision-making and language.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
It’s not a specific disease. It’s a clinical description of a set of symptoms caused by underlying brain diseases. The most common cause is Alzheimer’s disease.
If you have it, you might forget the name of a close friend or loved one. Or you might get lost in the neighborhood where you’ve lived for many years.
It isn’t part of normal aging. And it can shorten your lifespan, but how much varies.
An estimated 6.7 million U.S. adults age 65 or older have dementia.
There are three types. They differ based on the cause:
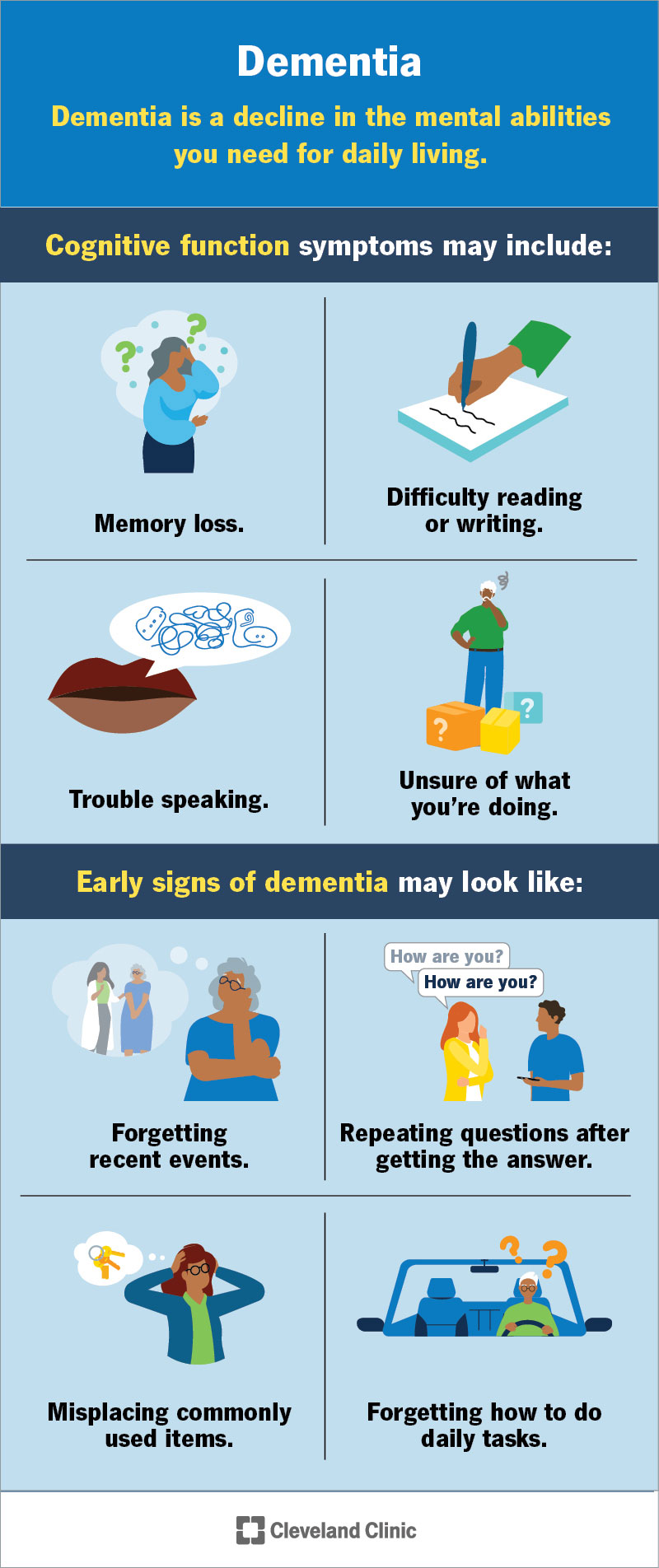
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/dementia)
Symptoms can vary based on the type and the area of your brain that has the most damage.
Cognitive symptoms are changes to your thinking and understanding. These may include:
Advertisement
These are changes in how you feel or relate to others. They can affect your mood, interests and personality. These may include:
Doctors may describe dementia in stages, based on how symptoms get worse over time. The three main stages are:
In the early stage, it affects your daily life, but not severely. You may notice some memory or thinking problems, but you can still do most self-care tasks at home, like dressing, bathing and making simple meals.
In the middle stage, thinking and daily tasks become harder. You may need reminders or prompts to complete them.
In the late stage, you need daily help and may require full-time care. Most thinking skills are lost, and you need support with basic activities, like eating, bathing and getting dressed.
Damaged brain cells cause dementia. In most cases, this damage comes from a neurodegenerative disease (a disease that slowly harms brain cells over time). These changes affect the parts of your brain that control memory, learning, language and decision-making.
Brain cells need to “talk” to each other by sending electrical signals. These signals help your brain work. When something blocks the signals or damages the cells, your brain can’t work properly.
Researchers are still studying why dementia develops in some people and not in others. In rare cases, a gene change can cause it.
Common disorders and conditions that cause secondary dementia include:
With reversible dementia, symptoms may go away once your provider treats what’s causing them. Some common causes include:
Advertisement
Certain factors may raise your chances of developing dementia. These include:
Your brain controls everything your body does. When it stops working properly, it can affect your overall health. Dementia can lead to serious problems, including:
Some of these problems can be life-threatening if not treated quickly. Unmanaged symptoms may lead to early death.
Advertisement
To find out if you have dementia, a provider will:
Diagnosing dementia can take time. That’s because many other disorders can cause similar symptoms. Your care team may need to rule out other problems first. While they work on getting the right diagnosis, they’ll help you manage symptoms.
Your provider may use one or more of the following tests to confirm a diagnosis:
Right now, there’s no cure. Researchers are working to better understand it. But many types of dementia are treatable.
No treatment can completely stop dementia from getting worse. But your provider can help you manage symptoms and reduce how much they affect your daily life.
Treatment can look different for each person because dementia affects everyone in different ways. What works well for one person may not work the same for you. Some treatments may also become less helpful as the disease progresses.
Medicines are usually the first type of treatment for most kinds of dementia. Common options include:
Advertisement
Your provider will explain which medicine is best for you and what side effects to watch for before starting treatment.
Treatment may include additional ways to support and improve your brain function, including:
Make an appointment with a provider if you or your loved ones notice changes in your:
If you or a loved one has dementia, you may want to ask a healthcare provider:
Video playlist content: This video playlist is available to watch online.
View video playlist online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_i18c4vdo/flavorId/1_5f3sgelj/format/applehttp/protocol/https/a.mp4)
Learn more about living with Alzheimer’s disease.
Dementia gets worse over time. Even with treatment, your memory and thinking skills may continue to decline. This can affect your safety and ability to care for yourself or loved ones.
It’s a good idea to make an advance directive. This is a written plan that tells your providers and family what kind of medical care you want in the future.
As symptoms progress, you may have to make tough decisions to stay safe. This could include:
These choices aren’t easy and can affect your emotions. Talking to a mental health professional or joining a support group may help you cope.
Researchers are still studying ways to cure dementia. New treatments and care options may be available in the future.
Dementia is a serious condition that usually shortens your life. But how long you live with dementia can vary.
One study found that people with Alzheimer’s disease lived for about 5.8 years after getting a dementia diagnosis. But people can live longer if they’re in otherwise good medical health.
Providers look at many things to help estimate life expectancy, including:
Each person’s medical history and life situation is different. Both can affect life expectancy.
You can’t prevent all types. But there are ways to lower your risk for some kinds. A healthcare provider can help you stay healthy and keep your brain strong. They may suggest:
Hearing that you have dementia is never easy. It’s normal to feel overwhelmed and worry about what lies ahead. This might distract you from the present and enjoying time with the people you love.
While no one can predict the future, you can take steps to plan for it. There are treatments that may help slow the symptoms of dementia. You may also want to talk with your healthcare provider or a social worker about completing important documents, like legal, financial and medical plans. These help make sure your wishes are clear, so others can speak up for you when you can’t.
Remember, your care team will be there to support you every step of the way. Help is available for both you and your loved ones throughout this journey.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
It can be unsettling when your brain stops working like it used to. Cleveland Clinic’s cognitive decline experts help you manage the symptoms and provide support.
