What is a pacemaker?
A pacemaker is a small device that helps control your heartbeat. It uses electrical impulses to keep your heart beating at a normal rate.
Why do I need a pacemaker?
You may need a pacemaker if you have a heart rate that is too slow (bradycardia) while resting and/or exercising, unexplained fainting spells (syncope) or heart failure.
How does a pacemaker work?
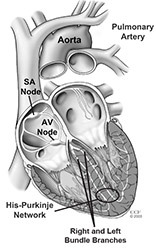
Your heartbeat is controlled by an electrical system in your heart. As electrical impulses travel through your heart, the top chambers (atria) and bottom chambers (ventricles) take turns squeezing and relaxing. When they relax, they fill with blood. When they squeeze (contract), blood is pushed out to the rest of your body.
The sinoatrial (SA) node, atrioventricular (AV) node, bundle branches and His- Purkinje network keep the electric impulse moving through your heart. If this pathway is interrupted, it causes changes to your heart rate and rhythm.
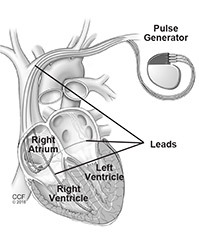
The pacemaker uses wires (leads) to sense your heart’s electrical activity. If needed, electricity travels through the leads to your heart muscle to keep the electric impulse moving. Your doctor will adjust your pacemaker settings as needed. The pacemaker only sends an impulse when your heart tries to drop below the set minimum.
The pacemaker uses a battery and a tiny computer, which are inside the pulse generator.
Types of pacemakers
Your doctor will talk to you about the type of pacemaker that is best for you.
Depending on your medical condition, you will need a:
- Single chamber pacemaker: Uses one lead in either your heart’s upper chamber (atrium) or lower chamber (ventricle).
- Dual chamber pacemaker: Uses two leads — one in your heart’s upper chamber (atrium) and one in the lower chamber (ventricle).
- Biventricular pacemaker: Uses three leads — one in your heart’s upper right chamber (atrium) and one in each lower chamber (right and left ventricles).
How is a pacemaker put in place?
The pacemaker is placed in a pocket that is created under your skin. This is usually done using an endocardial (transvenous) approach. But, your doctor may need to use an epicardial approach instead.
Endocardial approach - most common
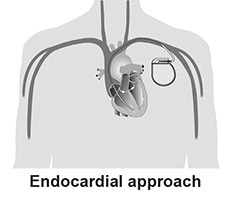
- The pacemaker/pulse generator is placed in your upper chest area, in a pocket created under your skin.
- Uses local anesthesia. You will be awake, but the procedure area will be numb, and you will get medicine to make you drowsy.
- A small incision is made in your upper chest.
- Your doctor guides the lead(s) into the incision, through a vein that leads to your heart.
- The lead tip(s) attach to your heart, and the other end connects to the pulse generator.
Epicardial approach
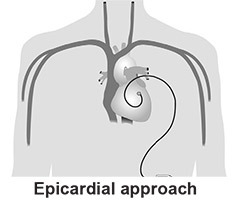
- The pacemaker/pulse generator is placed in your abdomen, in a pocket created under your skin.
- Uses general You will be asleep.
- If you need an epicardial approach, your doctor will talk to you about your surgery. You may have either a traditional or minimally invasive procedure.
Getting Ready for Your Procedure
The Day before Your Procedure: Call 800.223.2273 between 3 p.m. and 5 p.m. Ask for Pager 21215.
Medicine
- Make sure your doctor knows every type of medicine you take. This includes vitamins, supplements and medicine you buy without a prescription.
- Ask your doctor if you need to make changes to your medicine routine before your procedure.
- You may need to stop taking some types of medicine or make other changes.
- DO NOT make any changes to your medicine routine unless your doctor tells you to.
If you take blood thinners (Coumadin, aspirin or other anticoagulant):
- You may need to stop taking the medicine a few days before your procedure.
- If you take Coumadin, the results of your INR test must be in a good range before you can have your procedure.
- If you have diabetes, ask your nurse how to adjust your insulin/medicine.
Eating and drinking
- Eat a normal meal the evening before your procedure.
- DO NOT eat, drink or chew anything after 12 midnight before your procedure. This includes gum, mints and candy.
- If you need to take pills, take them with only small sips of water.
- Do not swallow any water when you brush your teeth.
Clothing, makeup, etc.
- DO NOT wear makeup or nail polish.
- Wear comfortable clothes to the hospital. You will change into a hospital gown for the procedure.
- DO NOT wear any jewelry (including wedding rings and watches).
- DO NOT bring any valuables to the hospital.
What should I bring to the hospital?
- Make sure you arrange to have someone drive you home from the hospital. Many patients go home the same day, but you may need to spend the night in the hospital.
- Bring a one-day supply of the medicine you take. This is in case your procedure is delayed and you need to take them. Do not take anything unless your healthcare provider tells you to.
- If you plan to spend the night in the hospital, pack a small bag with toiletries and other things you need for your comfort. Please leave the bag with the person who comes with you to the hospital.
During the Procedure
Where is the procedure performed?
Unless you are having surgery, your pacemaker implant procedure will be done in a procedure room in the Pacemaker Lab.
What can I expect?
- We will give you an IV in your arm or hand to give you fluids and medicine. This includes an antibiotic to prevent infection and medicine to make you drowsy.
- We will clean and remove any hair from the procedure area, then cover you with sterile paper sheets (drapes) from your neck to your feet.
- You will have a soft strap across your waist and arms to keep your hands from touching the sterile area.
- You will lie on a table with a large X-Ray machine above you, and a screen to the side. Your doctor uses these to guide the lead(s) into place.
- We will apply several sticky patches (electrodes) on your chest, back and heart. These are used to record an electrocardiogram (ECG/EKG) and, if needed, adjust your heart rate/rhythm during the procedure.
- We will keep track of your blood pressure (with a blood pressure cuff) and oxygen level (with a small clip on your finger).
How long does the procedure take?
The procedure takes 2 to 5 hours.
Will I feel pain?
- You should not feel any pain during the procedure. Please tell your doctor right away if you feel pain or have any symptoms.
- You will feel some burning/pinching when you get the anesthesia. The area will quickly become numb.
- You may feel a pulling sensation as your doctor makes the pocket for the pacemaker in the tissue under your skin.
How are the leads tested?
- Your doctor will test the leads after they are in place. This is called pacing.
- Pacing involves sending electricity through the leads to your heart.
- Your heart will contract, and you may feel your heart beat faster.
- Your doctor will connect the leads to the pacemaker/pulse generator after they are tested.
After the Procedure
How will I feel?
- You may feel discomfort at the pacemaker implant site during the first 48 hours after the procedure.
- Your doctor will tell you which medicine you can take for pain relief.
- Tell a member of your healthcare team if you have a lot of pain or if it does not go away.
Tests and monitoring
- You will have a chest X-ray to check your lungs and the position of the pacemaker and lead(s).
- We will keep track of your heart rate and rhythm with a telemetry monitor. This is a small box with wires that connect to electrodes on your chest.
Device Clinic
Before you go home, you will go to the Device Clinic to have your pacemaker programmed to the settings determined by your doctor.
- You will sit in a reclining chair while your pacemaker is programmed.
- Wires will be connected from a computer to electrodes on your chest.
- A nurse will use a programmer device over your pacemaker to change the settings.
- You may feel your heartbeat get faster or slower. This is normal, but please tell your nurse how you feel.
- If you have a biventricular pacemaker, you may have an echocardiogram (echo).
- Your doctor will review the results, and if there are no changes needed, you will be able to go home.
Follow-up and discharge instructions
- Ask your doctor if you need to take the same medicine you did before your procedure.
- We will talk to you about incision care, activity guidelines and follow-up appointments.
- We will give you a temporary ID card that lists the type of pacemaker and leads you have, the date of implant and your doctor’s name. Carry this card with you at all times in case you need medical care. You will get a permanent card from the pacemaker company within three months.
- Please let us know if you have any questions or concerns before you go home.
Questions or symptoms after you go home?
Call 216.444.6483 or 800.223.2273 ext. 46483 8 a.m. - 5:30 p.m. Monday - Friday. At other times, call 888.490.6121 to speak to a registered nurse 24/7 or call 800.223.2273 and ask for the EP Fellow on call. If you have an emergency, call 911 or have someone drive you to the nearest emergency department.