What is hypertrophic cardiomyopathy?
Hypertrophic cardiomyopathy (HCM) causes the heart muscle (myocardium) to become thick. The condition often affects the lower chambers of the heart (ventricles) and can also cause cellular changes and mitral valve problems.
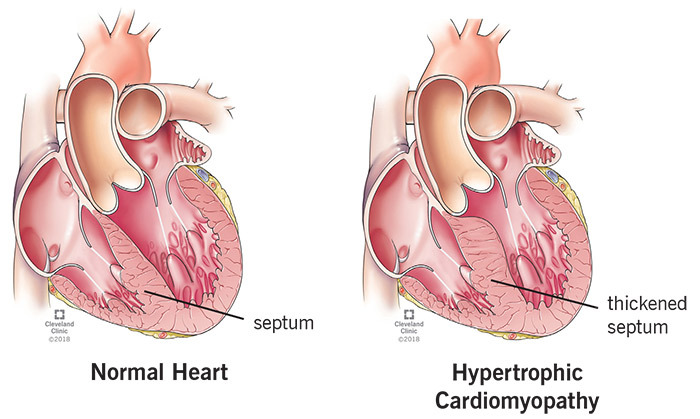
The most common area of the heart to be affected by HCM is the septum — the muscular wall that separates the left and right sides of the heart. If the area of the septum that separates the left and right ventricles is thickened, it can reduce or block blood flow to the aorta (outflow tract obstruction). This causes the ventricles to work harder to pump blood. This type of HCM may be called hypertrophic obstructive cardiomyopathy (HOCM).
Hypertrophic cardiomyopathy can cause thickening in other parts of the heart muscle, such as the bottom of the heart (apex), right ventricle or throughout the entire left ventricle.
As the heart muscle gets thicker, the left ventricle can become stiff. If the ventricle is stiff, it can’t relax and fill with blood as it should. As a result, there is less oxygen-rich blood available to pump to the organs and muscles. The stiffness in the left ventricle causes pressure to increase inside the heart and may cause mitral valve problems, such as leakage (regurgitation).
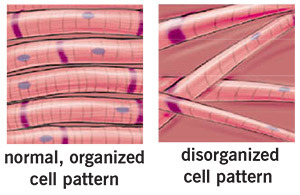
Hypertrophic cardiomyopathy causes cellular changes in the heart muscle. Through a microscope, the cells look disorganized and irregular (disarray) instead of being organized and parallel. This disarray can cause changes in the electrical signals that travel through the ventricles and cause an irregular heart rhythm called ventricular arrhythmia.
Who is affected by HCM?
Hypertrophic cardiomyopathy affects about 600,000 to 1.5 million Americans, or one in 500 people.
What are the symptoms and complications of HCM?
Many people with HCM live a normal life and do not have any related health problems. But, HCM can lead to heart conditions such as:
- Sudden cardiac arrest/sudden cardiac death: Sudden cardiac arrest means your heart suddenly stops working because of a fast heart rhythm called ventricular tachycardia. Unless you get emergency treatment, including CPR and defibrillation, right away, you can die (sudden cardiac death).
- Most people with HCM have a low risk for sudden cardiac death. However, HCM is the most common cause of sudden cardiac death in people under age 30. Hypertrophic cardiomyopathy may be best known as the cause of cardiac arrest and death in young athletes.
- Heart failure: A condition in which the heart’s pumping power is weaker than normal.
Associated symptoms
If you have ventricular tachycardia or heart failure, symptoms can include:
- Chest pain or pressure that usually happens when you exercise or are active, but it can also happen when you are resting or after you eat.
- Shortness of breath and fatigue, especially when you are active. These symptoms are often caused by a back-up of pressure in the top left chamber of your heart (left atrium) and lungs.
- Syncope (fainting/"passing out"). This can be caused by irregular heart rhythms or abnormal changes in your blood vessels when you exercise. The cause is sometimes unknown.
- Palpitations (feel of fluttering in the chest or skipped heartbeats) caused by an irregular heartbeat (arrhythmia). Atrial fibrillation is an arrhythmia that affects about 25 percent of people with HCM. The condition increases your risk of blood clots and heart failure.
What causes HCM?
- Hypertrophic cardiomyopathy can be inherited, caused by an abnormal gene that is linked to the heart muscle. There are many genes that can cause HCM, so it is common for families to have members with different types of HCM. It is also possible to have the HCM gene and not get the disease.
- High blood pressure and aging can cause HCM.
- The cause is sometimes unknown.
How is HCM diagnosed?
Your doctor will take several steps to find out if you have HCM. These include:
- A complete medical history. Your doctor will ask you about your symptoms and your family’s medical history.
- Physical exam. Your doctor will listen to your heart and lungs. Patients with HCM may have a heart murmur.
- Tests. An echocardiogram (echo) is often used to check for thickening of the heart walls. Your doctor may also order blood tests, an electrocardiogram (EKG), chest X-ray, exercise stress echo test, cardiac catheterization or magnetic resonance imaging (MRI).
What treatments are available for patients with HCM?
The type of treatment best for you depends on the problems you have that are caused by HCM. Your healthcare team will create a plan of care for you based on:
- Any narrowing you have in the blood vessels that blood travels through as it leaves your heart (outflow tract).
- How well your heart is working.
- Your symptoms.
- Your age and activity level.
- If you have an arrhythmia.
Treatment includes risk identification and regular follow-up visits. You may also need to make lifestyle changes, take medications or have a procedure.
Risk identification
Most people with HCM have a low risk of sudden cardiac death, but it is important to know your risk so you can take steps to prevent it. Your risk of sudden cardiac death is higher if you:
- Have a family history of sudden cardiac death.
- Are young and have had several episodes of syncope (fainting/"passing out").
- Have abnormal blood pressure when you exercise.
- Have had an irregular, fast heart rate.
- Have severe symptoms and your heart does not work well.
Your doctor will talk to you about your risk of sudden cardiac death. If you have two or more risk factors, you may need to take medication to control your heart rate or get an implantable cardioverter defibrillator (ICD) to reduce your risk.
Medications
Medications such as beta-blockers and calcium channel blockers relax the heart muscle. They help the heart fill with blood and do a better job of pumping blood through the heart and to the rest of your body. You may need to take other medications to control your heart rate.
Your doctor may have you take antibiotics to reduce your risk of bacterial endocarditis. This is a potentially life-threatening condition. Your risk of this infection is higher if you have HCM.
You may need to avoid certain medications, such as nitrates, because they lower your blood pressure, and digoxin, because it makes your heart squeeze harder when it contracts.
Procedures
Your doctor may talk to you about a septal myectomy, ethanol ablation, ICD and/or heart failure management.
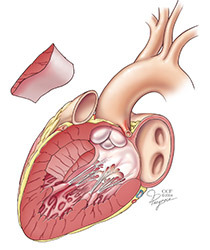
Septal myectomy
This surgery is done to remove a small amount of the thickened septal wall. This opens up the outflow tract from the left ventricle to the aorta. The procedure is used when treatment with medications does not help enough. A myectomy also often corrects mitral valve leakage (regurgitation).
Ethanol ablation (septal ablation)
This procedure is used when a septal myectomy cannot be done. The procedure is done in the cardiac catheterization (cath) lab. A cath is done to locate the coronary artery that sends blood to the upper part of the septum. A tiny balloon is used to open the artery. A contrast agent is used to show the blocked area of the outflow tract. A tiny amount of pure alcohol is injected through the catheter to the septum. This causes the septum to slowly shrink back to a more normal size over a period of a few months. As a result, more blood can flow through the outflow tract.
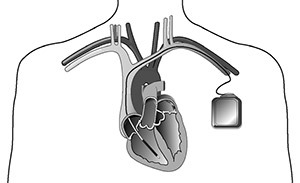
Implantable Cardioverter Defibrillators (ICDs)
An ICD is a small device placed just under the skin. It constantly monitors your heart rhythm. When it detects a very fast, abnormal heart rhythm, it delivers a small but powerful shock to your heart to get it back into a normal rhythm.
If you need a procedure, your doctor will talk to you more about what to expect and go over all the risks and benefits of the treatment.
Lifestyle changes
Depending on your condition and symptoms, you may need to make one or more changes, such as:
- Fluid and sodium restrictions if you have symptoms of heart failure.
- Your doctor will talk to you about which types of exercise are best for you. Most people with HCM can do non-competitive aerobic activities, but you may need to avoid high-intensity sports and heavy weightlifting.
Regular follow-up visits
Ask your doctor how often you need to be seen for regular follow-up visits. Follow-up care is very important to keep track of your condition and make any needed changes in your treatment.
Preventing bacterial endocarditis
Bacterial endocarditis (BE) is an infection of the heart valves or the heart’s inner lining (endocardium). It happens when germs (especially bacteria, but fungi and other microbes can also cause BE) enter the blood stream and attack the lining of the heart or the heart valves. Bacterial endocarditis causes growths or holes on the valves or scarring of the valve tissue, which often causes the valve to leak. Bacterial endocarditis can be deadly without treatment.
To Reduce Your Risk of BE:
- Take good care of your teeth and gums by brushing and flossing every day. See your dentist every 6 months. If you have dentures, make sure they fit properly.
- Call your doctor if you have symptoms of an infection, such as a fever over 100 degrees F; sweats or chills; skin rash; pain, tenderness, redness or swelling; a cut that won’t heal; red, warm or draining cuts or sores; sore throat, scratchy throat or pain when swallowing; sinus drainage, nasal congestion, headaches or tenderness along your upper cheekbones; a nagging cough that lasts more than two days; white patches in your mouth or on your tongue; nausea, vomiting or diarrhea.
- Don't wait to get treatment. Colds and the flu do not cause endocarditis, but infections, which may have the same symptoms, do cause endocarditis. To be safe, call your doctor.
- Ask your doctor about taking antibiotics before you have any dental or medical procedures to reduce your risk of BE.
- Ask your doctor for a BE identification card or request one from the American Heart Association (heart.org). Carry the card with you at all times.
For more information
- Contact the Heart & Vascular Institute Information and Resource Center Nurse toll-free at 866.289.6911 or email us using the Contact Us form at clevelandclinic.org/heart.
- The Hypertrophic Cardiomyopathy Association (HCMA) is dedicated to providing support and education to those with HCM, their families and other health care professionals. Call: 973.983.7429; email: support@hcma-heart.com; website: 4hcm.org.