The coronary arteries are the blood vessels that carry blood to your heart. Your heart pumps about 3,000 gallons of blood through your body every day.
What is coronary artery disease?
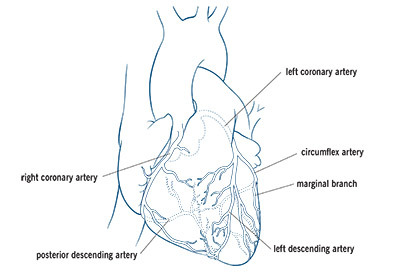
Coronary artery disease is the narrowing or blockage of the coronary arteries. This condition is usually caused by atherosclerosis. Atherosclerosis is the build-up of cholesterol and fatty deposits (called plaques) inside the arteries. These plaques can clog the arteries or damage the arteries, which limits or stops blood flow to the heart muscle.
If the heart does not get enough blood, it cannot get the oxygen and nutrients it needs to work properly. This can cause chest pain (angina) or a heart attack.
How does plaque build up in the arteries?
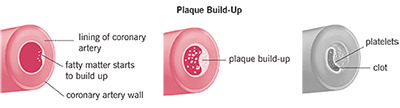
Healthy coronary arteries are smooth and elastic. The inside of these muscular hollow tubes are lined with a layer of cells called the endothelium. The endothelium helps protect the vessel walls and keep the arteries working properly so blood can flow freely.
Coronary artery disease starts when you are very young. Before your teen years, the blood vessel walls start to show streaks of fat. As you get older, the fat builds up, causing minor damage to your blood vessel walls. With time, other substances that move through your blood stream, such as inflammatory cells, cellular waste products, proteins and calcium, stick to the vessel walls. These things combine with the fat and form plaque.
Plaques are different sizes, and many are soft on the inside with a hard, fibrous “cap” that covers the outside. If the hard surface cracks or tears, the soft, fatty inside is exposed. Platelets (disc-shaped particles in the blood that help form clots) move to the area, and blood clots form around the plaque. The endothelium can also become irritated and stop working properly, which causes the artery to squeeze at the wrong times. This causes the artery to narrow even more.
Sometimes, the blood clot breaks apart and blood can flow through the area again. Other times, the blood clot suddenly blocks the blood supply to the heart muscle, causing one of three serious conditions known as an acute coronary syndrome.
What is collateral circulation?
If the blockage in a coronary artery slowly gets bigger, new blood vessels may form to reroute blood around the blockage. This is called collateral circulation. These new blood vessels may not be able to carry enough blood to the heart when you are active or under stress.
What is ischemia?
Ischemia is described as “cramping of the heart muscle.” It is similar to a leg cramp after you exercise a long time. The muscles in the legs cramp up because they need oxygen and nutrients. Your heart, which is also a muscle, needs oxygen and nutrients to keep working. If the heart muscle can’t get enough blood because the coronary artery is too narrow, it causes ischemia. When this happens, you may feel chest pain or other symptoms.
Ischemia happens most often when the heart needs extra oxygen, such as when you are active, eating, excited, stressed or exposed to cold.
If symptoms stop within 10 minutes after you rest or take medication, you may have stable coronary artery disease (stable angina). But, the problem can get worse and you may have symptoms even when you are resting.
You may have ischemia, or even a heart attack, but not have any symptoms. This is called silent ischemia. This condition is more common in people with diabetes.
What are acute coronary syndromes?
An acute coronary syndrome is caused by a sudden blockage in the blood supply to the heart. Some people have symptoms before they have an acute coronary syndrome, but you may not have symptoms until the condition occurs. Some patients never have any symptoms. Changes caused by an acute coronary syndrome can be seen on an electrocardiogram (ECG) and in blood tests.
Unstable angina: This may be a new symptom or can happen if you have stable angina that changes to unstable angina. You may start to have angina more often, when you are resting, or it may be worse or last longer. The condition can lead to a heart attack. If you have unstable angina, you will need medication, such as nitroglycerin or a procedure to correct the problem.
Non-ST segment elevation myocardial infarction (NSTEMI): This is a type of heart attack (MI) that does not cause major changes on an ECG. But, a blood test will show that there is damage to your heart muscle. The damage is usually minor since the blockage that causes an NSTEMI is often small or temporary.
ST segment elevation myocardial infarction (STEMI): This type of heart attack (MI) is caused by a sudden blockage of the blood supply to the heart.
If you have an acute coronary syndrome, call 911!
What are the symptoms of coronary artery disease?
The most common symptom of coronary artery disease is angina. Angina is chest pain and can also be described as chest discomfort, heaviness, tightness, pressure, aching, burning, numbness, fullness, or squeezing. It can be mistaken for indigestion or heartburn. Angina is usually felt in the chest, but you may also feel it in your left shoulder, arms, neck, back or jaw.
Other symptoms of coronary artery disease include:
- Shortness of breath.
- Heart palpitations: Irregular heartbeats, skipped beats or a “flip-flop” feeling in your chest.
- A faster-than-normal heartbeat.
- Dizziness.
- Nausea.
- Extreme weakness.
- Sweating.
What should I do if I have symptoms of coronary artery disease?
If the symptoms last longer than 5 minutes, CALL 911!
If the symptoms go away in 5 minutes and are new, worse or happening more often, call your doctor.
Do not wait to get help; Time is Muscle!
At the first signs of a heart attack, call 911. Do not wait for your symptoms to “go away.” Every minute you spend without treatment increases your risk of long-term heart damage.
Get to the hospital, even if you are not 100% sure you are having a heart attack!
If you have a prescription for nitroglycerin
If you have symptoms of angina and you have a prescription for nitroglycerin, stop what you are doing and rest. Take one dose (dissolve one tablet under your tongue or spray under your tongue). Wait 5 minutes. If you still have symptoms, call 911.
If you have chronic stable angina and you have symptoms, take one dose of nitroglycerin. Wait 5 minutes. If symptoms continue, take another dose. You can take 3 doses within 15 minutes. If symptoms continue after 3 doses, call 911.
Symptoms in women
Women can have different symptoms of coronary artery disease than men do. For example, many women who have a heart attack have:
- Pain or discomfort in the chest, left arm or back.
- A very fast heartbeat.
- Shortness of breath.
- Nausea or fatigue.
If you have any of these symptoms, get medical help right away. Call 911 or have someone take you to the nearest emergency room. Do not wait!
How is angina different from a heart attack?
The symptoms of a heart attack (myocardial infarction/MI) are similar to angina. But, angina is a warning symptom of heart disease, not a heart attack.
Angina
- Caused by a drop in blood supply to the heart due to the gradual build-up of blockage in the arteries.
- Does not cause permanent damage to the heart.
- Symptoms last a few minutes and usually stop if you rest or take medication. You may have chest pain or discomfort, shortness of breath, palpitations, fast heartbeat, dizziness, nausea, extreme weakness and sweating. Symptoms are often triggered by strenuous activity, stress, eating or being in the cold.
- Emergency medical attention is not needed. Call your doctor if you have not had symptoms before or if your symptoms have gotten worse or happen more often.
Heart attack
- Caused by a sudden lack of blood supply to the heart muscle. The blockage is often due to a clot in a coronary artery.
- Can cause permanent damage to the heart muscle.
- Symptoms usually last more than a few minutes and can come and go, and do not completely go away after taking nitroglycerin. Symptoms include chest pain or discomfort; pain or discomfort in other areas of the upper body; trouble breathing or shortness of breath; sweating or “cold” sweat; feeling full, like you are choking or indigestion; nausea or vomiting; lightheadedness; extreme weakness; anxiety; fast or irregular heartbeat.
- Emergency medical attention is needed if symptoms last longer than 5 minutes.
How is coronary artery disease diagnosed?
If you have symptoms that could be caused by coronary artery disease, your doctor will review your medical history and risk factors, do a complete exam, and order some tests. These can include blood work, an ECG, exercise stress tests, cardiac catheterization and coronary computed tomography angiogram (CTA). The test results show how severe the disease is, how it is affecting your heart, and are used to create your plan of care.
What are the risk factors for coronary artery disease?
There are several risk factors for coronary artery disease. There are some you can’t control (nonmodifiable) and many you can (modifiable). The more risk factors you have, the more you are at risk of having heart disease. Your doctor can help you understand your individual risk factors and what you can do to lower your risk.
Risk factors you CAN’T change:
- Male gender. Men have a higher risk of a heart attack than women, and they also have heart attacks earlier in life. The risk evens out after age 70.
- Age. You are more likely to have coronary artery disease as you get older, especially after age 65.
- Family history. Your risk of heart disease is higher if your parents have/had heart disease (especially before age 50). Ask your doctor when you should start regular preventive checks for heart disease.
- Race. The risk of heart disease is higher among African Americans, Mexican Americans, Native Americans, Native Hawaiians and some Asian Americans. The increased risks are caused by higher rates of high blood pressure, obesity and diabetes in these populations.
Risk factors you CAN change:
- Tobacco use and exposure to smoke.
- High cholesterol and triglyceride levels. Ask your doctor what your goals are for these.
- High blood pressure.
- Unhealthy diet.
- Uncontrolled diabetes.
- Being inactive.
- Being overweight (body mass index [BMI] 25-29) or obese (BMI >30). The way you carry your weight is also important. Your risk of heart disease is higher if your waist is more than 35 inches (women) or 40 inches (men). Your waist should be measured around your body, just above your belly button.
- Uncontrolled stress or anger.
What treatments are available for patients with coronary artery disease?
Your doctor will talk to you about the best treatment plan for you. Following your treatment plan will help reduce your risk of problems like heart attack and stroke.
Reduce your risk factors
The first step in treatment for coronary artery disease is reducing your risk factors. This involves making changes in your lifestyle.
- Don’t smoke. If you smoke or use tobacco products, quit. Talk to your doctor about ways to help you stop smoking, including medications.
- Manage health problems like high cholesterol, high blood pressure and diabetes.
- Eat a heart-healthy diet. Talk to your doctor or a registered dietitian about ways to change your diet to reduce your risk of heart disease.
- Limit alcohol use. Daily limits are one drink per day for women and two drinks per day for men.
- Increase your activity level. Exercise helps you lose weight, improve your physical condition and relieve stress. Most people can reduce their risk of heart attack by doing 30 minutes of walking 5 times per week or walking 10,000 steps per day. Talk to your doctor before you start any exercise program.
Medications
You may need to take medication to lower your cholesterol level or blood pressure or as treatment for other health conditions you have. It is important to take all medications as prescribed. Ask your doctor if you have any questions about which medications you should take or how to take them.
Interventional procedures
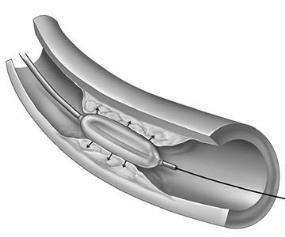
Interventional procedures are nonsurgical treatments to get rid of plaque build-up in the arteries and prevent blockages. Common procedures are balloon angioplasty (PTCA) and stenting. The procedures are done with a long, thin tube called a catheter. It is inserted into an artery through a small incision and guided to the blocked area of the artery to clear the plaque. Your doctor will give you more information if you need an interventional procedure.
Coronary artery bypass graft (CABG) surgery
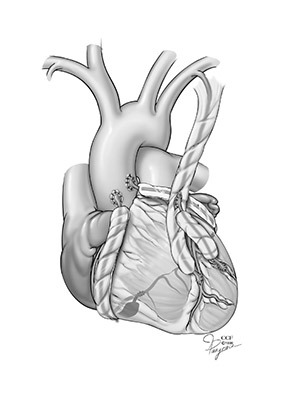
Coronary artery bypass graft (CABG) surgery involves creating a new path for blood to flow when there is a blockage in the coronary arteries. In most cases, the surgeon removes blood vessels from the patient’s chest, arm or leg, and creates the new pathway to deliver oxygen-rich blood to the heart. Your doctor will give you more information if you need CABG surgery.
Other treatment options
If traditional treatment options are not successful, your doctor may recommend other treatment options, such as:
Enhanced external counterpulsation (EECP): Inflatable cuffs (like blood pressure cuffs) are used to squeeze the blood vessels in your lower body. This helps improve blood flow to the heart by helping create natural bypasses (collaterals) around blocked coronary arteries. Enhanced external counterpulsation is a possible treatment for patients with chronic stable angina who cannot have an invasive procedure or bypass surgery and do not get relief from medication.
Important note: These procedures increase blood supply to your heart, but they do not cure coronary heart disease. You still need to follow the other parts of your treatment plan to help prevent your condition from getting worse.
Follow-up care
It is important to keep all follow-up appointments and have all tests your doctor orders. These are needed so your doctor can keep track of your condition and how well your treatment is working.