What are the carotid arteries?
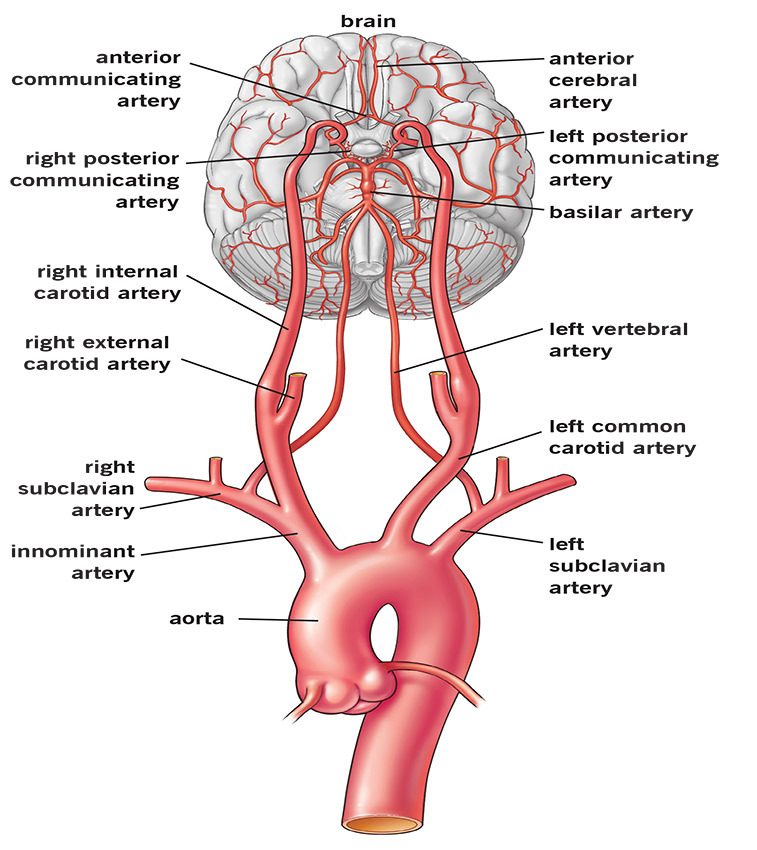
Arteries carry oxygen-rich blood away from the heart to the head and body. There are two carotid (kuh-ROT-id) arteries (one on each side of the neck) that carry blood to the brain. You can feel your carotid arteries on each side of the lower part of your neck, right below the angle of the jaw.
The carotid arteries send blood to the large, front part of the brain. This is the section that controls thinking, speech, personality and sensory and motor functions. Branches of the carotid arteries also send blood to the eyes.
The vertebral (ver TEE brul) arteries run through the spine. They send blood to the back part of the brain (the brainstem and cerebellum [sara-BELL-um]).
What is carotid artery disease?
Carotid artery disease means the carotid arteries have become narrowed. The condition is called carotid artery stenosis (sten-OH-sis). Carotid artery disease is usually caused by atherosclerosis (ath-er-oh-skler-OH-sis). Atherosclerosis is sometimes called “hardening of the arteries.” It is caused by a buildup of cholesterol, fat and other substances that travel through the bloodstream, such as inflammatory cells, cellular waste products, proteins and calcium. Over time, these substances stick to the blood vessel walls and combine to form a material called plaque (PLACK). Plaque buildup can cause the carotid arteries to become narrow or blocked, which reduces blood flow to the brain.
Who is at risk of atherosclerosis and carotid artery disease?
Risk factors for atherosclerosis, which can lead to carotid artery disease, include:
- Family history of atherosclerosis,carotid artery disease or coronary artery disease.
- Age: Men under age 75 have a greater risk than women of developing carotid artery disease, but women are at greater risk after age 75.
- High levels of low density lipoprotein (LDL/”bad” cholesterol) and triglycerides in the blood. However, this link is not as strong as it is for coronary artery disease.
- Smoking.
- High blood pressure (hypertension).
- Diabetes.
- Obesity.
- Sedentary lifestyle (a lack of exercise and activity).
Typically, carotid artery disease happens a few years later than coronary artery disease. Coronary arteries supply blood to the heart. People who have coronary artery disease have a higher risk of developing carotid artery disease.
What are the symptoms of carotid artery disease?
There are no symptoms of carotid artery disease itself. But you may have warning signs of a stroke. A transient ischemic attack (TIA or “mini-stroke”) is one of the most important warning signs. A TIA happens when a blood clot briefly blocks blood flow to the brain. Symptoms of a TIA and a stroke are the same, but they last only a short time (minutes to fewer than 24 hours) during a TIA. Symptoms include one or more of the following:
- Sudden trouble seeing or loss of vision in one or both eyes.
- Weakness and/or numbness on one side of the face, or in one arm or leg.
- Slurred speech or trouble talking.
- Trouble understanding what others are saying.
- Loss of coordination.
- Trouble swallowing.
A TIA is a medical emergency because it is impossible to know if it will turn into a major stroke. If you or someone you know has symptoms of a stroke/TIA, call 911. Getting treatment right away can save your life and increase your chance of a full recovery.
A person who has had a TIA is 10 times more likely to have a major stroke than someone who has not had a TIA.
What is a stroke?
A stroke happens when a blood vessel in the brain becomes blocked or bursts. The brain cannot store oxygen, so it depends on a network of blood vessels to provide it with blood that is rich in oxygen. A stroke results in a lack of blood supply, causing surrounding nerve cells to be cut off from their supply of nutrients and oxygen. When tissue is cut off from its supply of oxygen for more than 3 to 4 minutes, it begins to die.
You can have a stroke if:
- A piece of plaque or blood clot breaks off and travels to the smaller arteries of your brain.
- A blood clot forms and blocks a narrowed artery.
- The artery becomes extremely narrowed by plaque.
A stroke also can also be caused by other conditions, such as sudden bleeding in the brain (intracerebral hemorrhage), sudden bleeding in the spinal fluid space (subarachnoid hemorrhage), atrial fibrillation, cardiomyopathy.
How is carotid artery disease diagnosed?
If you are at risk of carotid artery disease, it is very important to have regular physical exams.
A doctor will listen to the arteries in your neck with a stethoscope. An abnormal rushing sound, called a bruit (BROO-ee), can mean you have carotid artery disease. But, you may have a blocked artery and not have bruits. You may also have a bruit even if the blockage is minor.
Diagnostic tests include:
- Carotid Duplex Ultrasound: An imaging procedure that uses high-frequency sound waves to view the carotid arteries to determine if there is narrowing.
- Carotid Angiography (an-gee-AH-gruff-ee)(carotid angiogram, carotid arteriogram, carotid angio): A catheter (thin, flexible tube) is put into a blood vessel in the arm or leg, and guided to the carotid arteries with the help of a special X-ray machine. Contrast dye is sent through the catheter while X-rays of the carotid arteries are taken. This test can be used to see if, or how badly, the carotid arteries are narrowed or blocked. It can also be done to find out your risk of having a stroke and the type of treatment you may need, such as stenting or surgery.
- Magnetic Resonance Angiography (MRA): MRA is a type of magnetic resonance image (MRI) scan that uses a magnetic field and radio waves to create pictures of the carotid arteries. Many times, an MRA can give your doctor more information than the results of an X-ray, ultrasound, or computed tomography (CT) scan. An MRA gives your doctor important information about the carotid and vertebral arteries and how badly they are blocked or narrowed.
- Computerized Tomography (CT Scan): You may have a CT of the brain if you had or may have had a stroke or TIA. The test shows the damage to the brain. During a CT scan, X-rays pass through the body and are picked up by detectors in the scanner. The test creates 3-D images on a computer screen. Depending on the the type of scan you have, you may have a special dye (contrast material) injected into a vein. The dye lets the radiologist (doctor who reads the scan results) clearly see the body structures on the CT image.
- Computed Tomography Angiography (CTA): A CTA uses advanced CT technology and a special dye (contrast material) injected into your vein to create high-resolution, 3-D pictures of the carotid arteries. CTA images show your doctor how badly the arteries are blocked or narrowed.
What treatments are available for patients with carotid artery disease?
If you have carotid artery disease, your treatment may include:
- Lifestyle changes.
- Medications.
- Procedures.
Lifestyle Changes
To prevent carotid artery disease from getting worse, these lifestyle changes are recommended by your doctor and the National Stroke Association:
- Quit smoking and using tobacco products.
- Control high blood pressure, cholesterol, diabetes and heart disease.
- Have regular checkups with your doctor.
- Have your doctor check your lipid profile and get treatment, if necessary to reach a lipid goal of LDL less than 100 and HDL greater than 45.
- Eat foods low in saturated fats, cholesterol and sodium.
- Reach and stay at a healthy weight.
- Exercise regularly for at least 30 minutes most days of the week.
- Limit the amount of alcohol you drink. Excessive alcohol use is defined as drinking more than three drinks per day. (One drink equals 12 ounces of beer or wine cooler, 5 ounces of wine, or 1.5 ounces of 80-proof liquor.).
Manage other risk factors:
- Find out if you have heart rhythm problems, such as atrial fibrillation (AF), which increases your risk of blood clots that can cause a stroke. If you have AF, you should take anticoagulant (blood-thinner) medications as prescribed.
- Talk to your doctor about circulation problems that can increase your risk of stroke.
Medications
- Antiplatelet medications: All patients with carotid artery disease should take an antiplatelet medication to reduce the risk of stroke and other cardiovascular disease complications. The most commonly used antiplatelet medication is aspirin. There are several other drugs that keep the platelets in your blood from “sticking together.” These include clopidogrel (Plavix) and dipyridamole (Persantine). Your doctor may have you take one of these medications alone or with aspirin to reduce your risk of stroke. You may need to take a blood-thinning medication (anticoagulant), such as warfarin (Coumadin) to reduce your risk of blood clots.
- Tissue plasminogen activator (t-PA): A clot-dissolving medication to treat patients who have a stroke caused by a blood clot (ischemic stroke). Eighty percent of all strokes are ischemic. This medication only works if you are given it within three hours after you first have symptoms of a stroke.
Treatment Procedures
If you have severe narrowing or blockage in the carotid artery, you will need a procedure to open the artery. This increases blood flow to the brain and prevents a future stroke. These procedures include carotid endarterectomy and carotid stenting.
Carotid endarterectomy is the traditional surgical treatment for patients with carotid artery disease. It is an effective treatment for many patients, especially those who have symptoms and at least a 50% blockage of the carotid arteries and those without symptoms who have at least a 60% blockage.
Carotid endarterectomy can be performed using general or local anesthesia. Your surgeon will make an incision in your neck where the artery is blocked. The plaque is removed from the artery, then the incision is closed and normal blood flow returns to the brain.
Carotid angioplasty and stenting is a possible treatment for some patients. You can ask your doctor if the treatment is an option for you.
Carotid angioplasty and stenting is performed while you are awake, but sedated. A balloon catheter is put inside a blood vessel. The doctor uses an X-ray to guide the catheter to the blocked or narrowed area of the carotid artery. A special guidewire with a filter (embolic protection device) is placed past the area of blockage or narrowing.
Once in place, the balloon tip is inflated for a few seconds to open or widen the artery. The filter collects any debris that may break off of the blockage. A stent (a small mesh tube) is placed in the artery and opens to fit the size of the artery. The stent stays in place permanently and acts as a scaffold to support the artery walls and keep the artery open. After several weeks, the artery heals around the stent.
Research shows that carotid stenting plus the filter is as safe and works as well as carotid endarterectomy for patients who are considered high risk for surgery.
Recovery from both the carotid endarterectomy and carotid angioplasty and stenting procedures generally requires a one-night hospital stay. Patients often return to regular activities within one to two weeks after these procedures.
Follow-up care
Your doctor will let you know how often you need to be seen and which tests you will need to keep track of how you are doing and how well your treatment is working.