Retinal detachment is a serious eye condition. The retina, the layer of tissue in the back of the eye, pulls away from tissues supporting it. Sudden changes, including eye floaters and flashes and darkening side vision, are signs this may be happening. A detached retina needs treatment as soon as possible.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
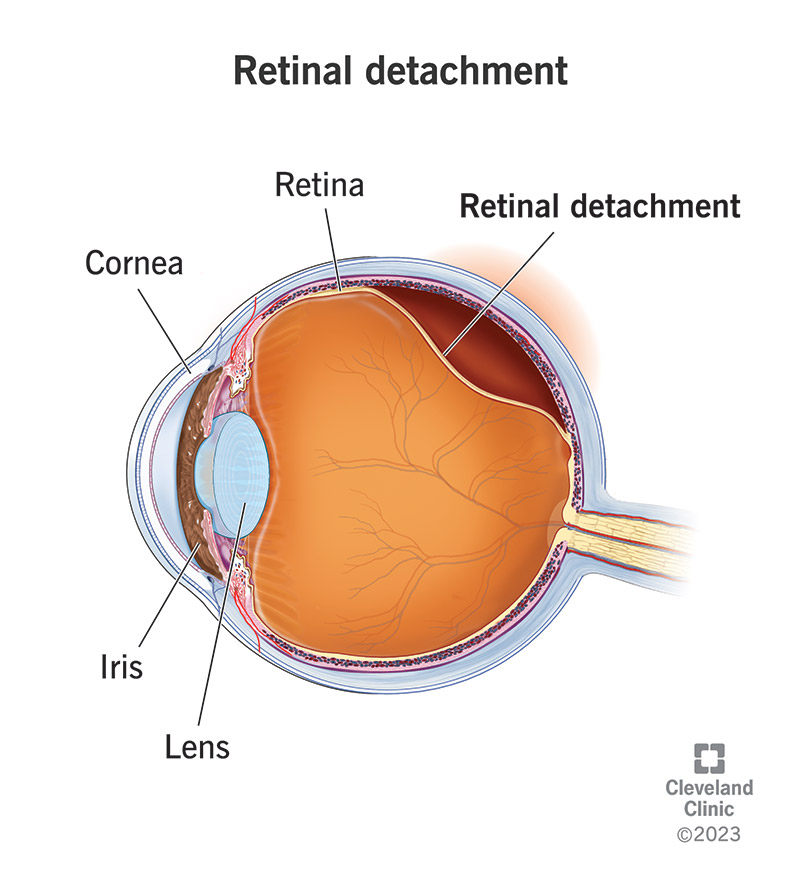
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/10705-retinal-detachment)
Retinal detachment is a painless but serious eye condition. It happens when your retina, the layer of tissue at the back of your eye, detaches from the tissues that support it. A detached retina affects your vision and can lead to blindness.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your retina senses light and sends signals to your brain so you can see. When your retina pulls away from the tissues that support it, it loses its blood supply. The blood vessels in those tissues carry nutrients and oxygen to your retina.
Call your eye care provider or go to the emergency room (ER) right away if you notice:
These can be symptoms of a detached retina. Don’t wait to see if you feel pain. Your provider will want to start treatment as soon as possible.
There are three types of retinal detachment:
Advertisement
Estimates for the incidence of retinal detachment vary. (The incidence is the number of new cases in a set period of time, usually a year.) One figure estimates incidence in the U.S. at 1 in 10,000 people. Another study estimates the annual risk of rhegmatogenous retinal detachment, the most common type, at 6.3 to 17.9 per 100,000 people.
Some people don’t notice any symptoms of retinal detachment, while others do. It depends on severity — if a larger part of the retina detaches, you’re more likely to experience symptoms.
Symptoms of a detached retina can happen suddenly and include:
Risk factors and causes for detached retinas include:
Having certain eye conditions also raises your risk for retinal detachment, such as:
If you’re at high risk for retinal detachment, talk to your healthcare provider. Your provider can help you set an eye exam schedule and suggest other steps to protect your eye health.
Having a detached retina is a serious condition that can cause loss of vision. Permanent blindness can happen as quickly as a few days.
You need an eye exam to diagnose retinal detachment. Your eye care provider will use a dilated eye exam to check your retina. They’ll put eye drops in your eyes. The drops dilate, or widen, the pupil. After a few minutes, your provider can get a close look at the retina.
Your provider may recommend other tests after the dilated eye exam. These tests are noninvasive. They won’t hurt. They help your provider see your retina clearly and in more detail:
Advertisement
Your eye care provider will discuss treatment options with you. You may need a combination of treatments for the best results.
Treatments include:
Laser (thermal) therapy or cryopexy (freezing)
Sometimes, your provider will diagnose a retinal tear before the retina starts pulling away. Your provider uses a medical laser or a freezing tool to seal the tear. These devices create a scar that holds the retina in place.
Pneumatic retinopexy
Your provider may recommend this approach for the right candidates. During pneumatic retinopexy:
After surgery, your provider will recommend that you keep your head still for a few days to promote healing. Your provider may also tell you what position you should lie in or sleep in.
These recommendations may seem uncomfortable or annoying, but they’re particularly important. It’s a short-term sacrifice for long-term benefits.
Advertisement
Scleral buckle
During a scleral buckle surgery:
Vitrectomy
During a vitrectomy, your provider:
If your provider uses an oil bubble, you’ll have it removed a few months later. Your body reabsorbs gas and air bubbles. If you have a gas bubble, you may have to avoid activities at certain altitudes. The altitude change can increase the size of the gas bubble and the pressure in your eye. You’ll have to avoid flying and traveling to high altitudes. Your provider will tell you when you can start these activities again.
Complications/side effects of treating retinal detachment
While surgery to reattach your retina is often very successful, any surgery can have risks or complications. These risks and complications include:
Advertisement
After treatment for a detached retina, you may have some discomfort. It can last for a few weeks. Your provider will discuss pain medicine and other forms of relief. You’ll also need to take it easy for a few weeks. Talk with your provider about when you can exercise, drive and get back to your regular activities.
Other things you can expect after surgery:
Your outlook depends on factors like how clear your vision was before the retinal detachment, how extensive your detachment was and if there are any other complicating factors. Your provider will talk to you about what type of vision improvement you can expect.
In general, surgery for rhegmatogenous retinal detachment is highly successful — the repair works about nine out of 10 times. Sometimes, people need more than one procedure to return the retina to its place.
It’s possible to get a detached retina more than once. You may need a second surgery if this happens. Talk to your provider about preventive steps you can take to protect your vision.
You can’t prevent rhegmatogenous retinal detachment, but you can take steps to lower your risk:
You can help to prevent diabetes-related tractional retinal detachment by improving your blood glucose levels and blood pressure.
People who have an average risk of eye disease should get eye exams once a year. If you’re at higher risk for eye disease, you may need checkups more frequently. Talk to your provider to figure out your best exam schedule.
It’s essential that you follow the instructions you get from your eye care provider about positioning and about your activities.
Ask your provider for suggestions on how to make things easier, like using a firm neck pillow to help keep your head in place. If you must lie face down or stay in that position for most of your time, your provider’s office can help you get face-down equipment for your home.
Your surgeon’s instructions will list situations that are emergencies, but you should contact your provider or get emergency help if you:
If you have retinal detachment (or face a higher risk), ask your provider:
Retinal detachment is a painless but serious condition. If you notice detached retina symptoms — a sudden increase in eye floaters, flashes of light or darkening of your vision — get care right away. Call your eye care provider or go to the emergency room. You’ll need some type of surgery to fix a detached retina. Waiting even days for treatment could mean permanent loss of vision. After surgery, it’s important to continue taking care of your eyesight by following your surgeon’s instructions.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Your eyes are one of your most important senses. If something goes wrong, it can change your world. Cleveland Clinic can help treat all types of retinal disease.
