A meningioma is a tumor that forms in your meninges, which are the layers of tissue that cover your brain and spinal cord. They’re the most common type of brain tumor. The tumors are usually noncancerous (benign). And they’re treatable.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
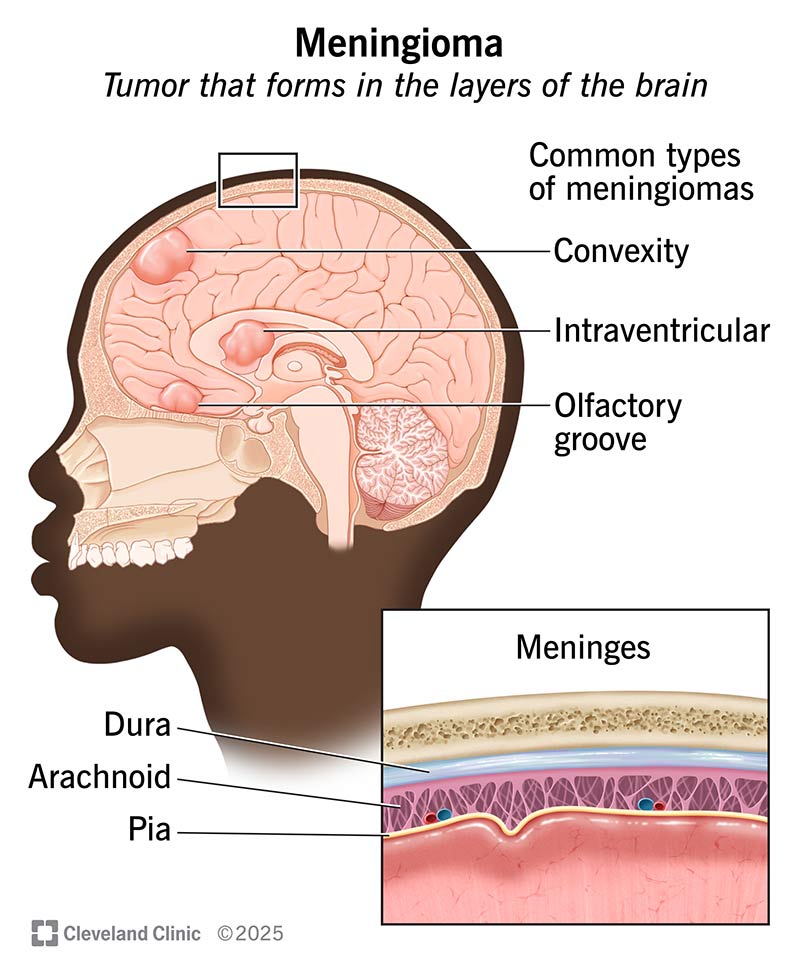
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17858-meningioma)
A meningioma is a tumor that grows in the tissue that surrounds your brain, called the meninges. These are three layers of tissue that cover and protect your brain and spinal cord.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Tumors are most often found near the top and the outer curve of your brain. They may also form at the base of your skull. Tumors that form around your spine are possible but rare.
These tumors tend to grow slowly. You might not notice you have this tumor until it becomes large. Symptoms usually happen because the tumor presses against your brain and affects how those areas function.
Meningiomas are the most common type of brain tumor. Most meningiomas aren’t cancerous (they’re benign). But some can be cancerous (malignant).
There are several different types based on their location, including:
There are three grades. Grades tell how severe the tumor is:
Advertisement
Because meningiomas are typically slow-growing, they may not cause noticeable symptoms until they grow large enough to push on important structures around them. Symptoms can vary depending on which part of your brain it affects.
Common meningioma symptoms may include:
Most tumors happen because of a chromosomal deletion. This is a genetic mutation where part of a chromosome is missing. These mutations happen randomly (sporadically). Or you may inherit them as part of certain genetic conditions, like:
Meningiomas can affect anyone. You may be more at risk for a meningioma if you:
Cancerous tumors are more common in males.
If the tumor is large and untreated, you may have the following complications:
To diagnose a meningioma, a healthcare provider will perform a physical and neurological exam. They’ll confirm with imaging tests like a CT scan or an MRI.
A meningioma can be difficult to diagnose. This is because it grows slowly and doesn’t cause symptoms until it’s bigger. Also, symptoms may resemble normal signs of aging in adults over 65.
Treatment for meningiomas varies from person to person. It’ll likely involve a combination of the following therapies:
Advertisement
Meningiomas may come back after treatment (recur). Tumors are less likely to come back if your surgeon can safely remove all of them during surgery.
If you have meningioma and notice new or different symptoms, report the changes to your provider as soon as possible.
If you’ve completed treatment for meningioma, your care doesn’t stop there. Your provider will keep monitoring your health, checking for tumor recurrence and managing any long-term side effects during follow-up visits.
Your life expectancy depends on several factors, including:
It varies from person to person. You should talk to your provider to learn more about what your life expectancy looks like.
A survival rate is a statistic that estimates the likelihood of surviving for a set period. It’s usually five years after a cancer diagnosis. For grade II and grade III tumors, the five-year survival rate is 63.5%.
It’s important to remember that survival rates are an estimate. Your provider can give you the most accurate information based on your situation.
Receiving a brain tumor diagnosis is unsettling, regardless of whether it’s benign or cancerous. The good news is that meningiomas are treatable. Know that your care team is there to provide you with robust, individualized treatment options and support. If you have any questions or concerns, don’t be afraid to ask. They’re available to help you.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you learn you have may have a noncancerous brain tumor, you’ll want the best care. Cleveland Clinic offers the latest in meningioma treatments.
