Parkinson’s disease is an age-related degenerative brain condition, meaning it causes parts of your brain to deteriorate. It’s best known for causing slowed movements, tremors, balance problems and more. Most cases happen for unknown reasons, but some are inherited. The condition isn’t curable, but there are many different treatment options.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Parkinson’s disease is a condition where a part of your brain deteriorates, causing more severe symptoms over time. While this condition is best known for how it affects muscle control, balance and movement, it can also cause a wide range of other effects on your senses, thinking ability, mental health and more.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The risk of developing Parkinson’s disease naturally increases with age, and the average age at which it starts is 60 years old. It’s slightly more common in males.
While Parkinson’s disease is usually age-related, it can happen in adults as young as 20 (though this is extremely rare, and often people have a parent, full sibling or child with the same condition).
Parkinson’s disease is very common overall, ranking second among age-related degenerative brain diseases. It’s also the most common motor (movement-related) brain disease. Experts estimate that it affects at least 1% of people over age 60 worldwide.
Parkinson’s disease causes a specific area of your brain, the basal ganglia, to deteriorate. As this area deteriorates, you lose the abilities those areas once controlled. Researchers have uncovered that Parkinson’s disease causes a major shift in your brain chemistry.
Under normal circumstances, your brain uses chemicals known as neurotransmitters to control how your brain cells (neurons) communicate with each other. When you have Parkinson’s disease, you don’t have enough dopamine, one of the most important neurotransmitters.
When your brain sends activation signals that tell your muscles to move, it fine-tunes your movements using cells that require dopamine. That’s why lack of dopamine causes the slowed movements and tremors symptoms of Parkinson’s disease.
Advertisement
As Parkinson’s disease progresses, the symptoms expand and intensify. Later stages of the disease often affect how your brain functions, causing dementia-like symptoms and depression.
“Parkinsonism” is an umbrella term that describes Parkinson’s disease and conditions with similar symptoms. It can refer not only to Parkinson’s disease but also to other conditions like multiple system atrophy or corticobasal degeneration.
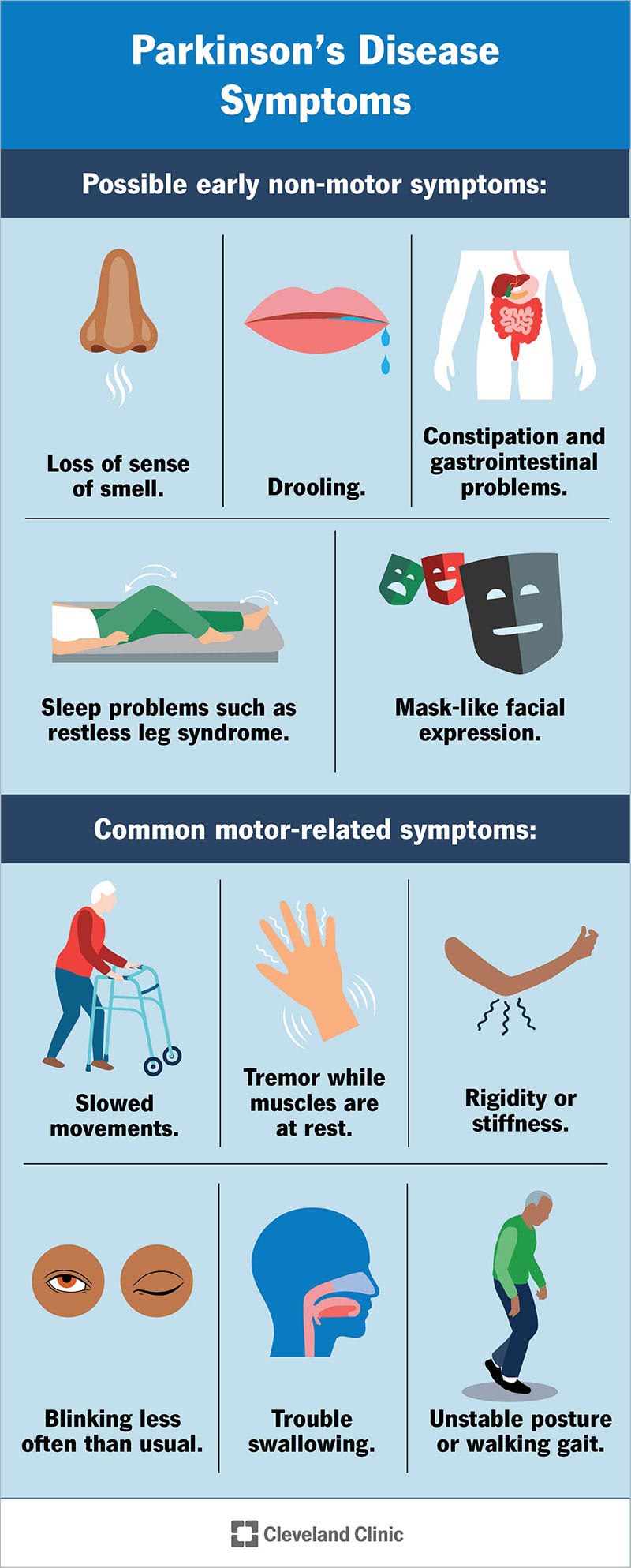
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/8525-parkinsons-disease)
The best-known symptoms of Parkinson’s disease involve loss of muscle control. However, experts now know that muscle control-related issues aren’t the only possible symptoms of Parkinson’s disease.
Motor symptoms — which means movement-related symptoms — of Parkinson’s disease include the following:
Additional motor symptoms can include:
Several symptoms are possible that aren’t connected to movement and muscle control. In years past, experts believed non-motor symptoms were risk factors for this disease when seen before motor symptoms. However, there’s a growing amount of evidence that these symptoms can appear in the earliest stages of the disease. That means these symptoms might be warning signs that start years or even decades before motor symptoms.
Non-motor symptoms (with the potential early warning symptoms in bold) include:
Advertisement
Parkinson’s disease can take years or even decades to cause severe effects. In 1967, two experts, Margaret Hoehn and Melvin Yahr, created the staging system for Parkinson’s disease. That staging system is no longer in widespread use because staging this condition is less helpful than determining how it affects each person’s life individually and then treating them accordingly.
Today, the Movement Disorder Society-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) is healthcare providers’ main tool to classify this disease. The MDS-UPDRS examines four different areas of how Parkinson’s disease affects you:
Advertisement
Although there are several recognized risk factors for Parkinson’s disease, such as exposure to pesticides, for now, the only confirmed causes of Parkinson’s disease are genetic. When Parkinson’s disease isn’t genetic, experts classify it as “idiopathic” (this term comes from Greek and means “a disease of its own”). That means they don’t know exactly why it happens.
Many conditions look like Parkinson’s disease but are instead parkinsonism (which refers to Parkinson’s disease-like conditions) from a specific cause like some psychiatric medications.
Parkinson’s disease can have a familial cause, which means you can inherit it from one or both of your parents. However, this only makes up about 10% of all cases.
Experts have linked at least seven different genes to Parkinson’s disease. They’ve linked three of those to early onset of the condition (meaning at a younger-than-usual age). Some genetic mutations also cause unique, distinguishing features.
Experts believe idiopathic Parkinson’s disease happens because of problems with how your body uses a protein called α-synuclein (alpha sy-nu-clee-in). Proteins are chemical molecules that have a very specific shape. When some proteins don’t have the correct shape — a problem known as protein misfolding — your body can’t use them and can’t break them down.
Advertisement
With nowhere to go, the proteins build up in various places or in certain cells (tangles or clumps of these proteins are called Lewy bodies). The buildup of these Lewy bodies (which doesn’t happen with some of the genetic problems that cause Parkinson’s disease) causes toxic effects and cell damage.
Protein misfolding is common in many other disorders, such as Alzheimer’s disease, Huntington’s disease, multiple forms of amyloidosis and more.
There are conditions or circumstances experts have linked to parkinsonism. While these aren’t true Parkinson’s disease, they have similar features, and healthcare providers may consider these causes while diagnosing Parkinson’s disease.
The possible causes are:
Parkinson’s disease isn’t contagious, and you can’t contract it from another person.
Diagnosing Parkinson’s disease is mostly a clinical process, meaning it relies heavily on a healthcare provider examining your symptoms, asking questions and reviewing your medical history. Some diagnostic and lab tests are possible, but these are usually needed to rule out other conditions or certain causes.
But most lab tests aren’t necessary unless you don’t respond to treatment for Parkinson’s disease, which can indicate you have another condition.
When healthcare providers suspect Parkinson’s disease or need to rule out other conditions, various imaging and diagnostic tests are possible. These include:
Researchers have found possible ways to test for possible indicators of Parkinson’s disease. Both of these new tests involve the alpha-synuclein protein but test for it in new, unusual ways. While these tests can’t tell you what conditions you have because of misfolded alpha-synuclein proteins, that information can still help your provider make a diagnosis.
The two tests use the following methods.
For now, Parkinson’s disease isn’t curable, but there are multiple ways to manage its symptoms. The treatments can also vary from person to person, depending on their specific symptoms and how well certain treatments work. Medications are the primary way to treat this condition.
A secondary treatment option is surgery to implant a device that will deliver a mild electrical current to part of your brain (this is known as deep brain stimulation). There are also some experimental options, such as stem cell-based treatments, but their availability often varies, and many aren’t an option for people with Parkinson’s disease.
Medication treatments for Parkinson’s disease fall into two categories: Direct treatments and symptom treatments. Direct treatments target Parkinson’s itself. Symptom treatments only treat certain effects of the disease.
Medications that treat Parkinson’s disease do so in multiple ways. Because of that, drugs that do one or more of the following are most likely:
Several medications treat specific symptoms of Parkinson’s disease. Symptoms treated often include the following:
In years past, surgery was an option to intentionally damage and scar a part of your brain that was malfunctioning because of Parkinson’s disease. Today, that same effect is possible using deep-brain stimulation, which uses an implanted device to deliver a mild electrical current to those same areas.
The major advantage is that deep-brain stimulation is reversible, while intentional scarring damage is not. This treatment approach is almost always an option in later stages of Parkinson’s disease when levodopa therapy becomes less effective, and in people who have tremor that doesn’t seem to respond to the usual medications.
Researchers are exploring other possible treatments that could help with Parkinson’s disease. While these aren’t widely available, they do offer hope to people with this condition. Some of the experimental treatment approaches include:
The complications and side effects that happen with Parkinson’s disease treatments depend on the treatments themselves, the severity of the condition, any other health issues you have, and more. Your healthcare provider is the best person to tell you more about the likely side effects and complications that you might experience. They can also tell you what you can do to minimize how those side effects or complications affect your life.
More about levodopa
The most common and effective treatment for Parkinson’s disease is levodopa. While this medication has greatly improved the treatment of Parkinson’s disease, providers use it cautiously because of how it works. They also commonly prescribe other medications that make levodopa more effective or help with side effects and certain symptoms.
Levodopa is often combined with other medications to keep your body from processing it before it enters your brain. That helps avoid other side effects of dopamine, especially nausea, vomiting and low blood pressure when you stand up (orthostatic hypotension).
Over time, the way your body uses levodopa changes, and levodopa can also lose its effectiveness. Increasing your dose can help with that, but that increases the chance and severity of side effects, and the dose can only go so high before it reaches toxic levels.
Parkinson’s disease isn’t a condition you can self-diagnose, and you shouldn’t try to manage the symptoms without first talking to a healthcare provider.
The time it takes to recover and see the effects of Parkinson’s disease treatments depends strongly on the type of treatments, the severity of the condition and other factors. Your healthcare provider is the best person to offer more information about what you can expect from treatment. The information they give you can consider any unique factors that might affect what you experience.
Parkinson’s disease is a degenerative condition, meaning the effects on your brain get worse over time. However, this condition usually takes time to get worse. Most people have a normal life span with this condition.
You’ll need little to no help in the earlier stages and can keep living independently. As the effects worsen, you’ll need medication to limit how the symptoms affect you. Most medications, especially levodopa, are moderately or even very effective once your provider finds the minimum dose you need to treat your symptoms.
Most of the effects and symptoms are manageable with treatment, but the treatments become less effective and more complicated over time. Living independently will also become more and more difficult as the disease worsens.
Parkinson’s disease isn’t curable, which means it’s a permanent, lifelong condition.
Parkinson’s disease isn’t fatal, but the symptoms and effects are often contributing factors to death. The average life expectancy for Parkinson’s disease in 1967 was a little under 10 years.
Since then, the average life expectancy has increased by about 55%, rising to more than 14.5 years. That, combined with the fact that Parkinson’s diagnosis is much more likely after age 60, means this condition doesn’t often affect your life expectancy by more than a few years (depending on the life expectancy in your country).
Parkinson’s disease happens for either genetic reasons or unpredictably. Neither is preventable, and you can’t reduce your risk of developing it. There are certain high-risk occupations such as farming and welding, but not everyone in these professions develops parkinsonism.
If you have Parkinson’s disease, the best thing you can do is follow the guidance of your healthcare provider on how to take care of yourself.
You should see your healthcare provider as recommended, or if you notice changes in your symptoms or the effectiveness of your medication. Adjustments to medications and dosages can make a huge difference in how Parkinson’s affects your life.
Your healthcare provider can give you guidance and information on signs or symptoms that mean you should go to the hospital or seek medical care. In general, you should seek care if you fall, especially when you lose consciousness or might have an injury to your head, neck, chest, back or abdomen.
Experts don’t know how most cases of Parkinson’s disease happen. About 10% of cases are genetic, meaning you inherit them from one or both parents. However, the remaining 90% or so are idiopathic, which means they happen for reasons that are still unknown.
Parkinson’s warning signs can be motor (movement-related) symptoms like slow movements, tremors or stiffness. However, they can also be non-motor symptoms. Many of the possible non-motor symptoms can appear years or even decades ahead of motor symptoms. But non-motor symptoms can also be vague, making it difficult to connect them to Parkinson’s disease.
Non-motor symptoms that might be early warning signs include:
No, Parkinson’s disease isn’t fatal on its own. But it can contribute to other conditions or problems that are sometimes fatal.
No, Parkinson’s disease isn’t curable. However, it is treatable, and many treatments are highly effective. It might also be possible to delay the progress and more severe symptoms of the disease.
Parkinson’s disease is a very common condition, and it’s more likely to happen to people as they get older. While Parkinson’s isn't curable, there are many ways to treat this condition. They include several different classes of medications, surgery to implant brain-stimulation devices and more. Thanks to advances in treatment and care, people can live for years or even decades with this condition and can adapt to or receive treatment for the effects and symptoms.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Shaky hands aren’t always because you’re tired or hungry. Cleveland Clinic brain experts can diagnose and treat your tremors and other Parkinson’s disease symptoms.
