Asthma is a condition that causes your airways to swell, narrow and fill with mucus. This can make it hard to breathe or cause other symptoms, like chest tightness, cough and wheezing. Common asthma triggers include allergies (like pets or pollen), smoke, cold weather, exercise, strong smells and stress. Asthma attacks can be fatal if not treated.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
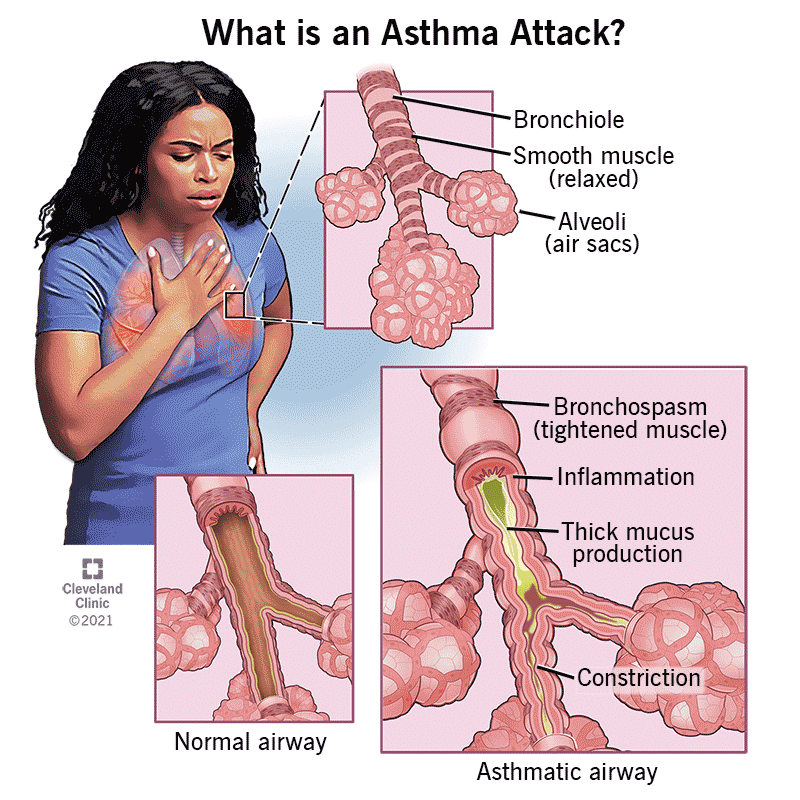
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/6424-asthma)
Asthma is a condition that causes long-term (chronic) inflammation in your airways. The inflammation makes them react to certain triggers, like pollen, exercise or cold air. During these attacks, your airways narrow (bronchospasm), swell up and fill with mucus. This makes it hard to breathe or causes you to cough or wheeze. Without treatment, these flare-ups can be fatal.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Millions of people in the U.S. and around the world have asthma. It can start in childhood or develop when you’re an adult. It’s sometimes called bronchial asthma.
Types of asthma include:
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_m8hom1mo/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Neha Solanki, MD, shares what causes asthma and if patients can outgrow it.
Symptoms of asthma include:
You might have asthma most of the time (persistent asthma). Or you might feel fine in between asthma attacks (intermittent asthma).
Experts aren’t sure what causes asthma. But you might be at a higher risk if you:
Asthma triggers are anything that causes asthma symptoms or makes them worse. You might have one specific trigger or many. Common triggers include:
Advertisement
Asthma triggers can bring on an attack right away. Or it might take hours or days for an attack to start after you’re exposure to a trigger.
Asthma can cause severe flare-ups that don’t get better with treatment (status asthmaticus). This can be fatal if you can’t get enough oxygen to your organs and tissues.
An allergist or pulmonologist diagnoses asthma by asking about your symptoms and performing lung function tests. They’ll ask about your personal and family medical history. It can be helpful to let them know what makes asthma symptoms worse and if anything helps you feel better.
Your provider might determine how well your lungs are working and rule out other conditions with:
The best way to manage asthma is to avoid any known triggers and use medications to keep your airways open. Your provider might prescribe:
Advertisement
Your healthcare provider will work with you to develop an asthma action plan. This plan tells you how and when to use your medicines. It also tells you what to do when you have certain symptoms and when to seek emergency care. Ask your healthcare provider to walk you through it.
Talk to your healthcare provider if you’re having frequent asthma attacks or feel like your symptoms aren’t manageable. Make sure you understand your asthma action plan and when to go to the emergency room.
Use your rescue inhaler, then call 911 (or your local emergency number) if you’re having a severe asthma attack or are experiencing these symptoms:
Most people with asthma can manage their symptoms. Asthma management means you:
Some people are able to avoid triggers and have no symptoms most of the time. Others need to use a maintenance inhaler or other medications in addition to avoiding triggers. Kids may have fewer or no symptoms as they get older and their airways get bigger.
Advertisement
You might be able to reduce or avoid asthma symptoms with a few everyday habits. These include:
Some people have lived with asthma their whole lives. Others are taken by surprise by a diagnosis as an adult. It can take time to figure out your triggers and find ways to manage your breathing that work for you. Working closely with your healthcare team can help. It might be reassuring to know that most people are able to manage their asthma symptoms and continue doing the things they love.
Advertisement
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
You might feel anxious when your child gasps and wheezes. Cleveland Clinic Children’s asthma experts are here to help them (and you) breathe easier.
