
The sweltering 90-degree temperatures and heavy humidity pushed dozens of en plein artists to their limits as they spread out across the streets, parks, and riverbanks of Dexter, Michigan, to capture its historic architecture and small-town charm.
Among them was 57-year-old Laurie Apling, undeterred by the intense summer conditions. She spent hours at a time in the blazing sun, standing nearly motionless at her easel as she carefully applied oil paint to canvas during the annual Paint Dexter Plein Air Festival.
“It was challenging; tough for everyone,” says Laurie, who later sold two of the oil paintings she completed onsite and submitted for judging during the competition. “I just didn’t want to miss it.”
No one would have blamed Laurie for stepping back—especially since, two weeks earlier, she had undergone one of the world’s first robotically assisted aortic valve replacement (AVR) surgeries, performed through a transcervical approach at Cleveland Clinic.
The minimally invasive technique, developed by Laurie’s cardiothoracic surgeon Marijan Koprivanac, MD, allows patients to return to daily life more quickly and typically with less pain than traditional open-heart AVR, as well as other minimally invasive approaches that access the heart through the chest wall.

Laurie with Dr. Koprivanac following an appointment. (Courtesy: Laurie Apling)
“This innovative approach is still open-heart surgery,” says Dr. Koprivanac, “but we’re not disrupting the chest wall by cutting through ribs, muscles, and nerves.” He recently presented findings from his robotically assisted, transcervical aortic valve replacement technique at the annual meeting of the American Association for Thoracic Surgery. “Our new approach is showing a true benefit for patients.”
Dr. Koprivanac makes four small incisions, three in the chest to allow clamps and other instruments to reach the surgical site, and one in the crease of the neck, which offers the added benefit of minimizing visible scarring. The neck incision serves as the main entry point for two robotic arms, which Dr. Koprivanac guides to provide a direct, “down the barrel” view of the aorta and the damaged valve.
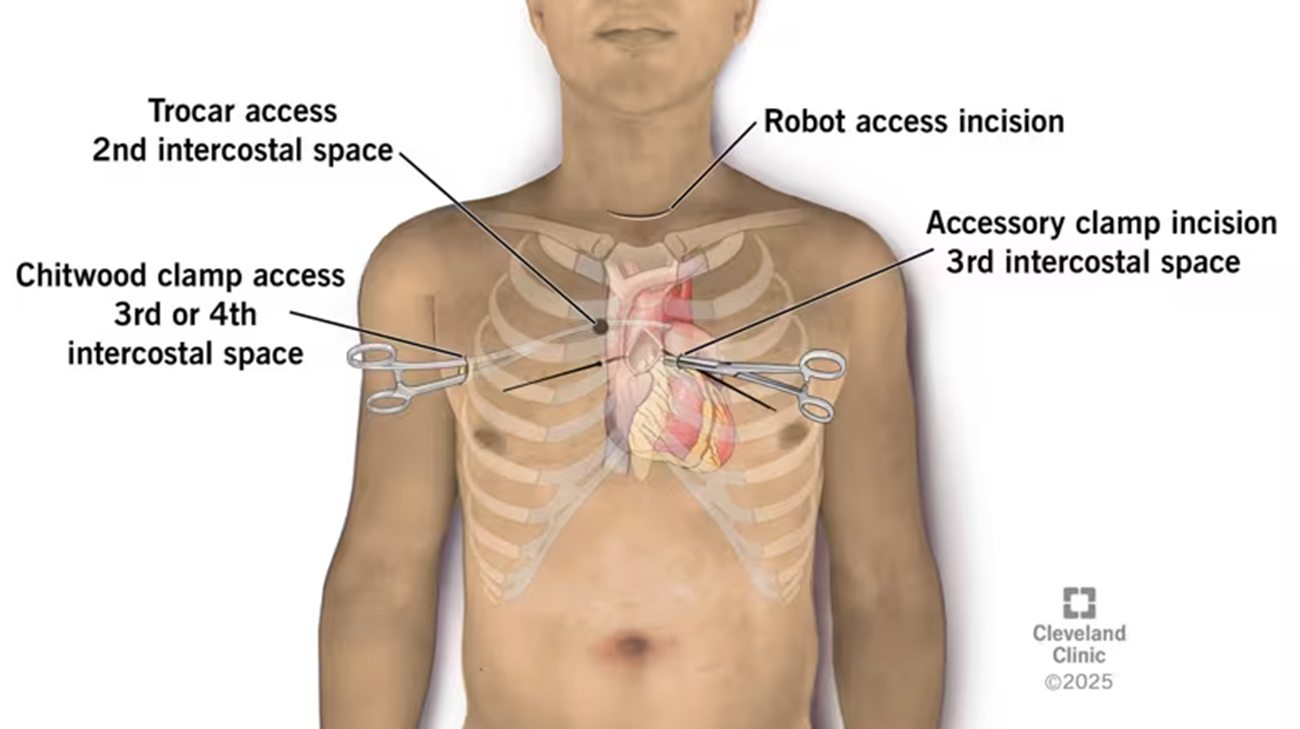
Illustration showing placement of the four incisions in transcervical robotic AVR. (Courtesy: Cleveland Clinic)
As he further explains, “Neck access for various surgeries is an extremely well-developed approach. The neck heals outstandingly well and is extremely resistant to infections. By going through a skin crease in the neck, there is no visible neck scar after about a year.”
As Laurie can attest, the most meaningful benefits of the procedure include small incisions, minimal post-operative pain—without the need for narcotics—and a remarkably quick recovery. She was discharged just two days after surgery and was back to her regular routine, including physically demanding activities within a couple of weeks.
Typically very active, Laurie began experiencing unusual fatigue in early 2025, often needing naps that stretched for hours. Despite normal blood work, her primary care physician detected a heart murmur and referred her to a cardiologist. That’s when Laurie was diagnosed with bicuspid aortic valve disease—a condition that affects the proper flow of blood to and from the heart.

Surgeons performing the transcervical aortic valve replacement surgery at Cleveland Clinic. (Courtesy: Cleveland Clinic)
When Laurie learned her aortic valve would likely need to be replaced, she began researching major medical centers within driving distance of her home in central Michigan. She ultimately decided on Cleveland Clinic and connected with Dr. Koprivanac, known for his expertise in aortic and bicuspid valve surgery and his work advancing minimally invasive techniques for cardiac surgery.
Given Laurie’s overall good health, Dr. Koprivanac explained she was an ideal candidate for his new approach. Understanding this method could offer a faster recovery and less pain, Laurie agreed without hesitation—and has had no regrets.

After undergoing an innovative heart surgery, Laurie has been able to more quickly get back to her active lifestyle. (Courtesy: Laurie Apling)
Encouraged by the successful results of the minimally invasive technique, Dr. Koprivanac and his surgical team are continuing to refine the procedure. Their efforts include designing specialized instruments to enhance precision and improve patient outcomes even further.
“I’m doing really well,” says Laurie, who is preparing for a trip to Milan, Italy, with her online Italian language classmates—a journey she hopes will include time for painting. “I’ve gone back to working out, lifting weights and going to aerobics classes.”
Related Institutes: Heart, Vascular & Thoracic Institute (Miller Family)

