
In July, Kurt Pilker became the 2,000th Cleveland Clinic patient to undergo a lung transplant. He experienced some déjà vu in doing so. The 35-year-old resident of Niagara Falls, New York, was also Cleveland Clinic’s approximately 1,300th lung transplant patient in 2013.
“The surgeon was different, but much of the team was the same,” says Kurt, who is recuperating well from his second double-lung transplant. “Even though I live 3 ½ hours away from Cleveland, I know I’ll get the best result possible at the Clinic.”
According to Kenneth McCurry, MD, a cardiothoracic surgeon and surgical director of the lung and lung-heart transplant program, lungs have a higher rate of transplant rejection than most other organs because they are used to breathe, increasing their exposure to the external environment in comparison to other organs, including the heart.
“Because the lungs have so much exposure to bacteria, viruses and other pathogens, these events can stimulate the immune system or damage the lungs, resulting in chronic rejection. Other factors can also contribute, such as aspiration. As a result, the need for re-transplantation can be common in the first five years after a transplant,” Dr. McCurry explains. “But for someone like Kurt who is young, pretty strong and has good functioning kidneys, his prognosis for doing well with the second transplant is quite good.”
Kurt’s pulmonary problems are a direct result of having been born with cystic fibrosis (CF). A genetic disease, CF causes sticky, thick mucus to build up in organs, including the lungs. Over time, the mucus increasingly clogs the airways, making it difficult to breathe. It also leads to chronic infection of the lungs, which causes lung destruction.

Nurse practitioner Carol Wegus listens to Kurt's lungs after his double-lung transplant. (Courtesy: Cleveland Clinic)
The slow, progressive nature of the disease became especially problematic for Kurt in his mid-twenties, requiring frequent hospitalizations to obtain the levels of oxygen required to survive.
“In the year prior to my first transplant, I spent 270 days in the hospital,” recalls Kurt, one of three siblings in his family to have battled CF. “I’ve always joked that when it comes to being in the hospital for weeks at a time, you either get used to it or go insane. I tell people I went insane and that helped me get used to it.”
Actually, Kurt’s positive, upbeat attitude has sustained him in good times and bad. “I don’t let CF define me,” he states. “Life’s going to suck sometimes. The question is: what do you want to make of it? Are you going to let it drag you down? Or use it to improve yourself?”
After Kurt’s initial double-lung transplant, he was – at last – able to live a much more normal life. He was strong enough to attend Edinboro University in Pennsylvania, earning a bachelor’s degree in computer science network and system administration. He quickly landed a job as an IT help desk technician, and began dating Samantha Kwan. They got married in 2017.
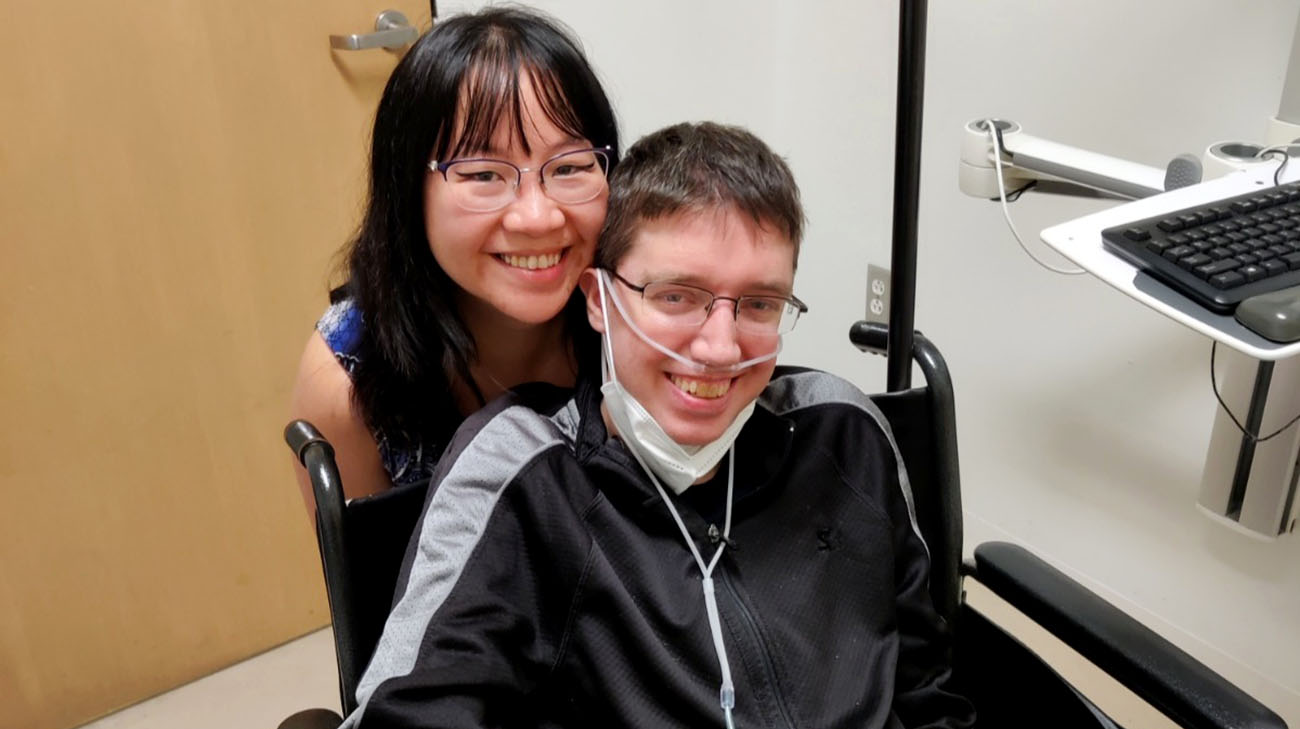
Kurt and his wife, Samantha, before his second double-lung transplant. (Courtesy: Kurt Pilker)
However, Kurt’s body began to slowly but steadily reject his transplanted lungs. “I had to go into the hospital several times because it became much more difficult to breathe. It became worse and worse. Eventually, I even had a hard time just walking short distances.”
As Dr. McCurry explains, while lung transplant patients require immunosuppressive drugs to keep the body’s immune system from ‘attacking’ the new organs, doing so can also increase the risk of infection, which can also cause the new organs to fail. That’s what happened to Kurt.
“While it’s frustrating to go through the process again, many patients do quite well for a long period of time with a second transplant,” Dr. McCurry adds. “Sometimes, even much better than the first transplant.”
However, to even become eligible for a second transplant, Kurt had work to do. His body mass index (BMI) revealed he was drastically underweight. At just 92 pounds at the time, Kurt would need to gain at least 18 pounds to be considered strong enough to tolerate transplant surgery.
For a year, Kurt forced himself to eat more than usual, and for a time he required the use of a surgically-inserted gastrostomy tube, which delivers nourishment directly to the stomach. “Eventually, I was putting on a pound or two a month. For me, that’s amazing. I’d never put that much weight on before, that quickly, in my life.”

Kurt visits Niagara Falls with his family before his double-lung transplant. (Courtesy: Kurt Pilker)
Finally, Kurt’s BMI was sufficient, and he was placed on the national organ transplant waiting list. For his first transplant, Kurt had to endure a nine-month wait. This time, surprisingly to him and his family, his new lungs were available in just over two weeks.
The transplant was completed without major complications. Kurt is regaining his strength while undergoing frequent tests, including those measuring his oxygen levels. He hopes to return home to Niagara Falls shortly, resume working and begin something he’s long dreamed of – leisure travel with Samantha.
“My mom has a condominium near Pensacola, Florida, on the beach, but I’ve never been well enough to travel that far,” Kurt says. “We hope to get there soon.”
On average, about 120 patients undergo lung transplant surgery annually at Cleveland Clinic, a number that has increased significantly over the last 10 years.
“Our program is now in its 30th year and we’re proud to be a leader in lung transplantation,” says Dr. McCurry. “Lungs are a very difficult organ to transplant, but with steady improvements in surgical techniques, post-operative care, and innovative strategies that allow transplantation of more lungs, we have been able to provide this life-saving therapy to many more patients, and the success rate for patients is quite high.”
Kurt jokes he didn’t receive a reward for being recipient number 2,000, but quickly corrects himself. “I got new lungs. That’s a pretty good reward!”
Register with Lifebanc to become an organ donor.
Related Institutes: Heart, Vascular & Thoracic Institute (Miller Family), Respiratory Institute, Digestive Disease & Surgery Institute

