The low-FODMAP diet reduces certain kinds of carbohydrates that are hard for people to digest. It’s often prescribed as an elimination diet to identify food triggers in those who have functional gastrointestinal disorders, such as IBS.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
FODMAP is an acronym for a certain class of carbohydrates, called fermentable short-chain carbohydrates, which are more difficult for people to digest. (The full acronym stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols.) The low-FODMAP diet temporarily restricts these carbohydrates in order to relieve uncomfortable symptoms and give your digestive system a rest. Removing irritants gives your gut lining a chance to repair itself and can help restore a healthy balance of gut flora. If your symptoms improve, you can use the low-FODMAP diet to figure out which foods to limit in the future.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
FODMAPs are:
Fermentable. These are all foods that your gut bacteria feed on, converting them to gasses in a chemical process called fermentation.
Oligosaccharides. These are soluble plant fibers known as prebiotics, which feed the beneficial bacteria in your gut. Oligosaccharides include onions, garlic, beans/lentils and many wheat products. Sensitivity to oligosaccharides may help explain some cases of non-celiac gluten sensitivity. Since gluten-free grains are lower in fermentable sugars than grains that have gluten, some people who think they are sensitive to gluten may actually be sensitive to the oligosaccharides residing in wheat products.
Disaccharides. Lactose is the fermentable sugar in this group, the sugar in dairy and breast milk. Lactose intolerance is one of the most common food intolerances worldwide.
Monosaccharides. Fructose, the sugar in fruit, is the fermentable sugar in this group. But only in certain quantities and proportions, so not all fruits are affected.
Polyols. These are sugar alcohols, commonly used as artificial sweeteners. They are also found naturally in some fruits.
FODMAPs are fermentable short-chain carbohydrates. Translated, that means two things: They are sugar molecules that are linked together in chains, and they are fermentable by the bacteria in your gut. Molecules in chains need to be broken down into single molecules to be absorbed through your small intestine. But FODMAPs can’t be broken down, so they can’t be absorbed there. Your small intestine draws in extra water to help move the FODMAPs through to your large intestine. There, the bacteria living in your colon have a field day fermenting them (eating them). This produces gasses and fatty acids as byproducts inside your gut.
Advertisement
Not at all. In fact, our digestive systems are designed to process some foods that we can’t fully digest ourselves — for example, dietary fiber, which has an important place in digestive health. And feeding the bacteria in our gut is part of our symbiotic arrangement with those bacteria. But some people with sensitive guts experience a level of indigestion from these foods that significantly impacts their quality of life. For these people, the byproducts of fermentation cause chronic symptoms of gas, bloating, abdominal pain and distension. The extra water drawn by the small intestine may cause diarrhea in excess, or constipation if there isn’t enough.
The low-FODMAP diet is often prescribed for limited periods for people diagnosed with irritable bowel syndrome (IBS) and small intestinal bacterial overgrowth (SIBO). Studies show that a majority of people living with these conditions benefit from the diet. It can also be used as a short-term elimination diet for anyone who has digestive problems and wants to try and isolate the foods that are causing them. An elimination diet removes common problem foods and then adds them back in systematically to observe how your system reacts. The low-FODMAP diet is just one of many elimination diets that you can use to discover food sensitivities.
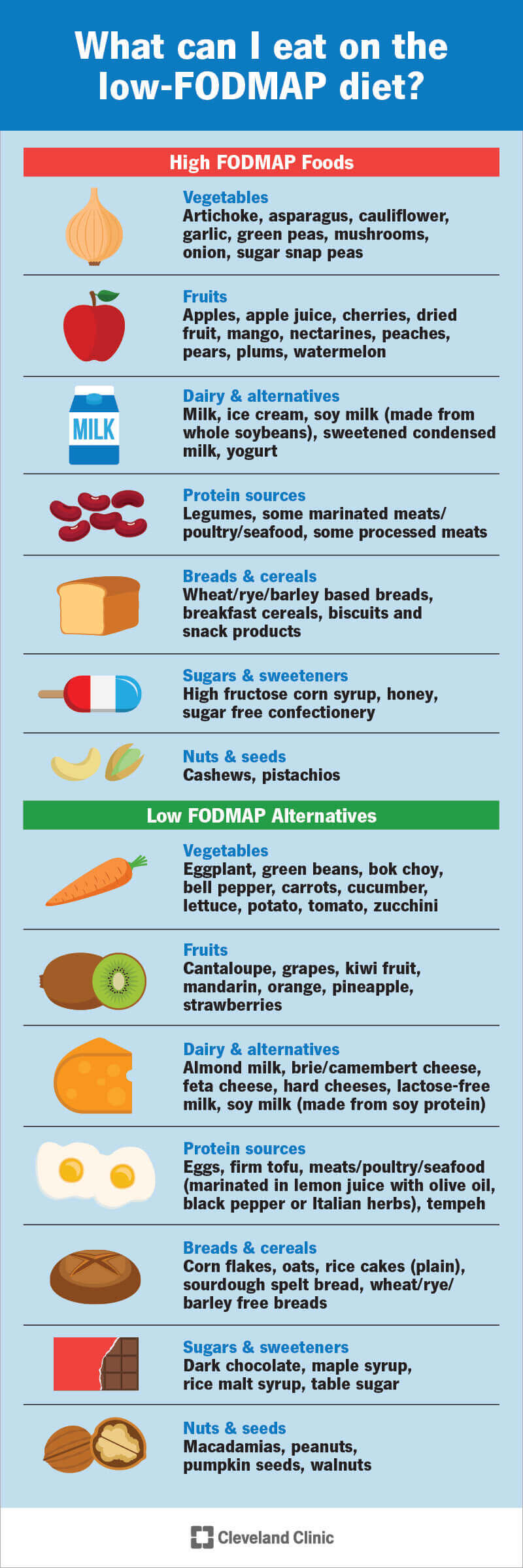
The diet has three phases: an elimination phase, a reintroduction phase and a maintenance phase that’s customized to you. During the elimination phase, you'll avoid all of the high-FODMAP foods — a list of specific fruits, vegetables, dairy products and grains. At first glance, the elimination phase of the diet may seem very limited. But there’s still a good list of foods in each category that you can eat. It takes some mental discipline to follow, but you won’t go hungry on the diet. After two to four weeks, you’ll begin the reintroduction phase, in which you systematically add foods back in. The third phase keeps what works for you and leaves out what doesn’t.
Certain fruits, vegetables, grains and proteins are higher and lower in FODMAPs. Some are OK to eat in limited amounts but will bother you in larger amounts. For example, most legumes and processed meats are high in FODMAPs, but plain-cooked meats, tofu and eggs are low-FODMAP protein sources. Apples, watermelon and stone fruits are high in FODMAPs, but grapes, strawberries and pineapples are OK. A ripe banana is high in fructose, but you can have up to a third cut up in your cereal, or you can have a whole one if it’s not quite ripe. Your dietitian can help provide you with these kinds of specific guidelines for your diet.
Advertisement
This is the question that you’ll need to answer for yourself during the process of the low-FODMAP diet. The answer will be different for everyone. The point of the diet is not to deprive you of “bad” foods but to find out if your symptoms are related to FODMAPs or not — and if they are, which ones. Some people may not improve at all on the elimination phase. If you don't, there’s no reason to follow through to the next phase. But if you do, it will be very important to reintroduce foods in a systematic way to separate the real offenders from foods that you can tolerate. Many people find in the end that it’s only one or two of the FODMAP food groups that bother them. The ultimate goal of the diet is to widen your dietary options as much as possible.
Consult a reliable healthcare provider. Whether you’ve already been diagnosed with a gastrointestinal (GI) disease or you are just beginning to explore possible causes and cures for your symptoms, a registered dietitian or GI specialist can help set you in the right direction. They may have alternative ideas to test before you try the diet. They can also help guide you through the nuances of the diet, provide shopping and menu guides and troubleshoot when questions or problems arise. There’s a lot to keep track of with this diet, including different quantities and portion sizes for different foods. It’s easier to follow successfully if you have a guide who knows the way around.
Advertisement
Plan ahead. This is a temporary diet, but it’s a significant investment of time and trouble in the meantime. Make sure you reserve a chunk of time to complete it when it won’t conflict with other important events or obligations. You can’t cheat on an elimination diet — the whole experiment collapses if you do. Make an intentional commitment to yourself to complete the process before you start. Be deliberate about setting the stage. Clear your fridge and pantry of high-FODMAP foods and prepare some menu plans in advance. Make sure you have ingredients for a few simple standby meals that you know you can prepare and enjoy easily.
Phase 1: Healthcare providers recommend at least two weeks and no more than six weeks for the elimination phase. It can take time for this phase to work and your symptoms to subside. If you have SIBO, the process of starving your overgrown gut bacteria may produce detox symptoms, making you feel worse before you feel better. But even if you feel great on the elimination phase, it’s not meant to be permanent. It’s important to find out which foods you may be able to reintroduce and tolerate. A more moderate diet will be easier to maintain over time, and in nutrition, variety is always the best policy for getting all of your micronutrients.
Advertisement
Phases 2 & 3: The length of the reintroduction phase can vary depending on the individual, but the average time is about eight weeks. During this phase, you’ll stay on the low-FODMAP diet while reintroducing a high FODMAP food from each FODMAP category, one at a time. You’ll spend a few days testing each food in increasing quantities to find your tolerance threshold. Between each test, you’ll spend a few days back on the strict elimination diet to avoid any crossover effects. Once you find out what works for you and what doesn’t, you and your healthcare provider can put together a sustainable, nutritious diet plan that you can keep indefinitely, or until you want to retest.
It’s an experiment, and it may not work. But if you follow the diet under expert guidance, it’s safe to try. Your healthcare provider will keep an eye on your general nutrition and any deficiencies or weight loss that may occur. They’ll tell you when it’s time to stop and try something else. The low-FODMAP diet has a high predicted success rate for people with IBS, but up to 25% may not benefit. For all other conditions, research is more limited, but there’s reason to believe it may help with symptom management in cases of SIBO, IBD and functional dyspepsia. If it doesn’t, your journey isn’t over — there are other kinds of elimination diets, tests and therapies to try.
The low-FODMAP diet is a specific approach to identifying and reducing foods that may be irritating your gut and causing you gastrointestinal distress. If you have chronic symptoms or food sensitivities, you might benefit from following the systematic elimination process. Although it’s strict in the short term, this is not a lifestyle diet. The intent is to isolate your food triggers and then reintroduce as many foods as possible. Many of the foods identified as FODMAPs represent a normally healthy diet. They include nutritious vegetables, fruits and whole grains. These aren’t “bad” foods — but eliminating the ones that trouble you can help you enjoy the ones that don’t.
Last reviewed on 02/24/2022.
Learn more about the Health Library and our editorial process.