Microscopic polyangiitis (MPA) is a rare type of vasculitis that causes blood vessel inflammation. MPA can damage your organs. Areas most commonly affected by MPA include your kidneys, lungs, nerves, skin and joints.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
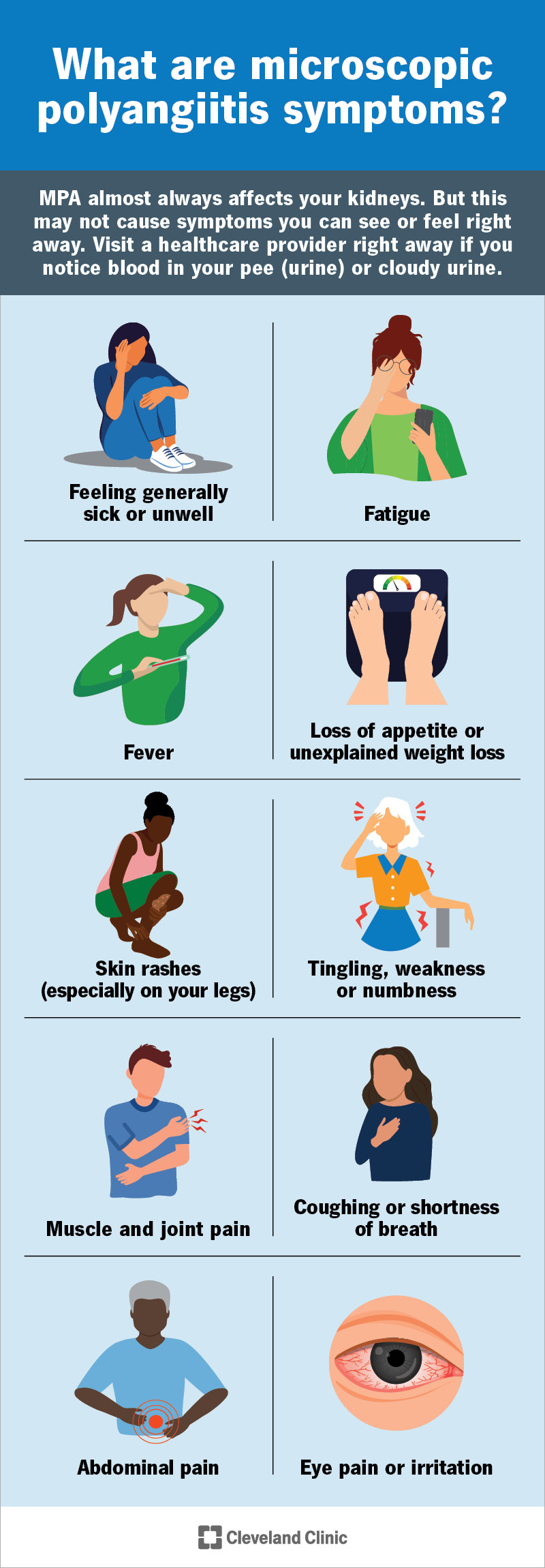
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/microscopic-polyangiitis-mpa-Infographic)
Microscopic polyangiitis (MPA) is a type of vasculitis, a condition that causes inflammation in your blood vessels.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
MPA’s name refers to how it affects you. “Angiitis” is another name for vasculitis. “Poly” means many. And “microscopic” means small. So, MPA is a vasculitis that can affect many small blood vessels in your body. It most commonly affects your:
If you have MPA, the small blood vessels in your body become inflamed. This can damage them in different ways. In some cases, inflammation causes vessel walls to thicken and the openings to narrow, which limits blood flow. In other cases, the vessel walls become thinner and weaker, which can lead to bleeding in nearby tissues. Both types of damage can affect your organs.
Some common MPA symptoms include:
MPA almost always affects your kidneys. But this may not cause symptoms you can see or feel. It can cause blood in your pee (urine) or cloudy pee. Visit a healthcare provider right away if you notice either of these.
MPA is an autoimmune disease. Autoimmune diseases happen when your immune system attacks your body instead of protecting it. Experts aren’t sure what makes this happen.
Advertisement
Some researchers think antineutrophil cytoplasmic antibodies (ANCA) may contribute to this disease. Some healthcare providers call MPA ANCA-associated vasculitis, or ANCA vasculitis.
ANCA are a type of autoantibody. Antibodies are proteins your immune system makes to identify and destroy invaders like germs. Autoantibodies are proteins that mistakenly target healthy tissue in your body. Around 7 in 10 people with MPA have ANCA in their blood when they’re diagnosed.
MPA can affect anyone. But it’s slightly more common in males. It’s also more likely to develop in people around age 50.
MPA can cause serious, potentially life-threatening complications if it damages your kidneys or lungs. Severe MPA can cause:
A healthcare provider will diagnose MPA by learning as much as they can about your health. They’ll ask about the symptoms you’re experiencing and when you first noticed them. Tell your provider if any of the symptoms come and go. Or if any activities seem to make them worse. Let them know if you’ve ever coughed up blood or noticed any changes in your pee. Your provider will give you a physical exam and run some tests.
Diagnosing this disease requires your provider to consider a differential diagnosis — a list of possible conditions that could explain your symptoms. This means your provider will use tests to rule out other, more common conditions before confirming MPA.
To diagnose MPA, your provider will start with blood and urine tests and a chest X-ray. Depending on the symptoms, you may also need:
You’ll need to see a rheumatologist as well. This is a healthcare provider who specializes in treating inflammatory diseases. If MPA affects your kidneys, you’ll also need to work with a kidney specialist.
Treating inflammation and limiting how much it damages your blood vessels is the most important part of managing MPA. Your provider will prescribe a combination of medications, including glucocorticoids (like prednisone) and another immunosuppressant.
You might need higher doses of medication at first. Then, after you start to improve, your provider will reduce your dosage or reduce how often you take medications. The goal is to help you reach remission. This is when there’s no active inflammation that could damage your blood vessels or organs.
Once you’ve reached remission, you’ll continue taking immunosuppressants. You may need these for a long time, maybe for the rest of your life. Your provider will tell you how long you’ll need medications for MPA. This depends on its severity, how much it’s damaged your organs and how well you’re tolerating medications.
Advertisement
Your provider will let you know how often you’ll need regular follow-up appointments, tests and/or screenings.
Talk to your provider if you notice any changes in the symptoms you experience. Especially if it feels like they’re happening more often or are more severe. Or if you’re having new symptoms. And tell your provider if it feels like treatment isn’t working or isn’t as effective as it used to be.
There’s no cure for MPA. But many people enter extended periods of remission after treatment. You may be in remission for months or years before experiencing symptoms again. Healthcare providers call this a relapse. It’s possible that you may never have a relapse.
Your provider will help you understand what you can expect in the future. It’s usually based on how much MPA has damaged your blood vessels and organs and the treatments you need.
MPA (microscopic polyangiitis) is treatable. And most people achieve remission once they start treatment. Talk to your healthcare provider if it ever feels like you’re experiencing new or worsening symptoms.
Never be afraid to ask any questions or share any concerns. Your provider is there to help you understand everything you need to know about your body and health.
Advertisement
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
