Leptospirosis is an illness caused by the bacteria Leptospira. You can get it after getting water or soil contaminated by animal pee (urine) in your nose, mouth, eyes or a break in your skin. Leptospirosis most often causes flu-like symptoms. These can worsen into Weil’s syndrome, a life-threatening illness, in a small number of people.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
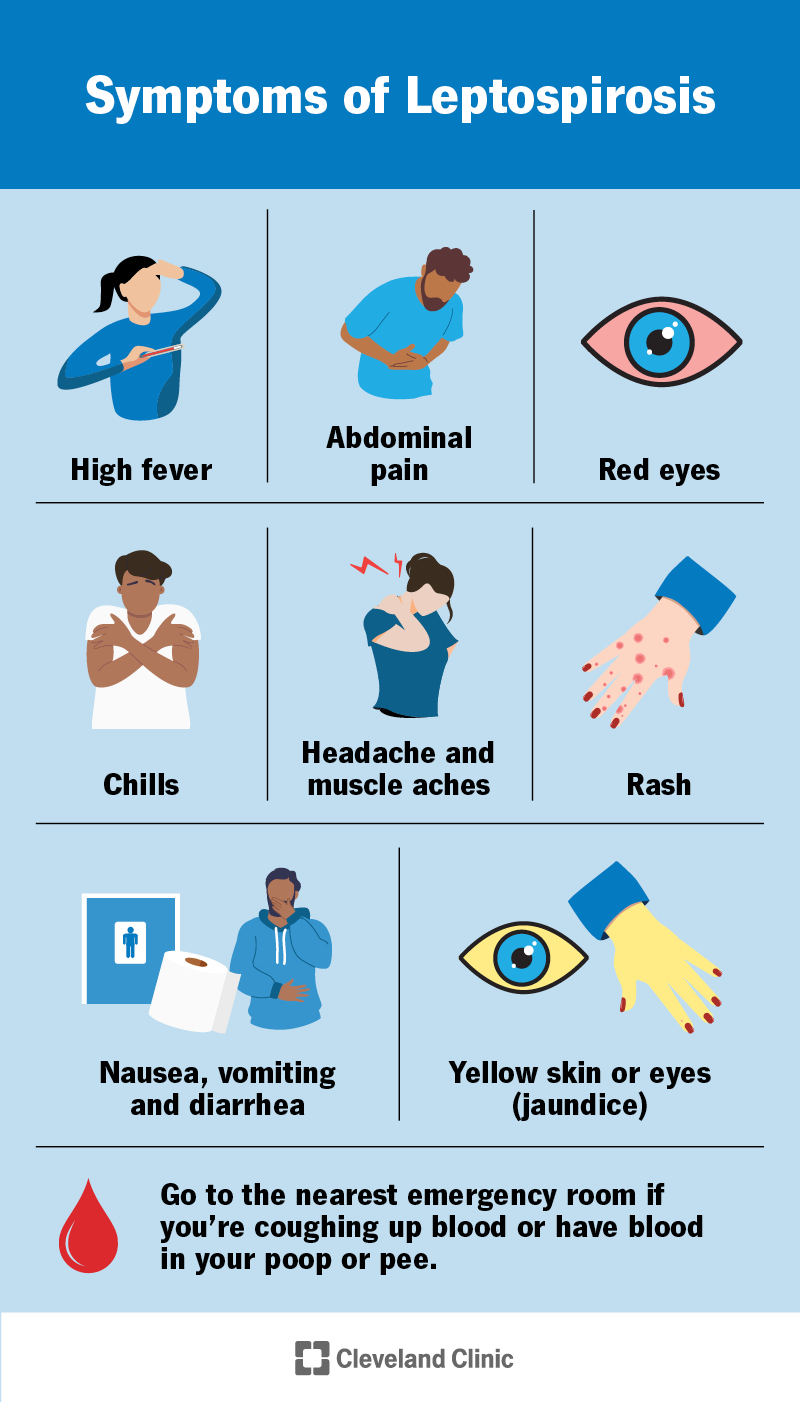
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/leptospirosis)
Leptospirosis is a flu-like illness caused by the bacteria Leptospira. You can get infected through breaks in your skin, or through your eyes, nose or mouth.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Leptospirosis (pronounced “lep-toh-spy-ROH-sis”) is a zoonotic disease. This means it’s transmitted between animals and humans. You can get infected through:
Leptospirosis has two phases: the leptospiremic (acute) phase and the immune (delayed) phase. You may have mild symptoms or no symptoms in the leptospiremic phase. Some people develop severe symptoms in the immune phase.
During the leptospiremic phase (also called the septicemic phase), bacteria are in your bloodstream and moving to your organs. You may get sudden, flu-like symptoms. They usually start within two to 14 days after a Leptospira infection. They last between three and 10 days. Blood tests will show signs of infection.
In the immune phase, Leptospira bacteria have moved from your blood to your organs. The bacteria are most concentrated in your kidneys, which make pee.
A small number of people will get very sick with Weil’s syndrome in this phase. Weil’s syndrome causes internal bleeding, kidney damage and severe yellowing of your skin and eyes (jaundice). Urine tests will show signs of the bacteria, and you’ll have antibodies to Leptospira in your blood.
Advertisement
Some people start out with flu-like symptoms, and some have no symptoms at all. Initial symptoms of leptospirosis can include:
Severe leptospirosis (Weil’s syndrome) symptoms may start three to 10 days later. You may start feeling better before severe symptoms start. They include:
The bacteria Leptospira cause leptospirosis. Bacteria get into your body through your mouth, nose or eyes. They can also enter through breaks in your skin. They travel through your blood to your organs, collecting in your kidneys (the organ that “cleans” your blood). Bacteria from your kidneys leave your body in your pee, which can spread leptospirosis to other people or animals.
Leptospirosis is usually spread to humans from animal pee containing the bacteria Leptospira. Almost any mammal (like rats, dogs, horses, pigs or cows) can get leptospirosis. They may have few or no symptoms of illness.
Animals with leptospirosis can contaminate water or dirt (soil), which spreads the bacteria to other animals or humans. You can get leptospirosis from:
A large number of people can get leptospirosis at once (an outbreak) after heavy rains and flooding. The floodwaters wash into rivers, lakes and canals, bringing bacteria with them.
Leptospirosis is rarely contagious from one person to another. But sometimes, outbreaks have happened in people living closely in a shared living space.
You can get leptospirosis no matter where you live, but it’s most common in tropical areas and warmer climates with lots of rainfall each year. You’re at an increased risk for leptospirosis if you live in or travel to these areas. They include:
There have been outbreaks in the U.S. after flooding in Hawaii, Florida and Puerto Rico.
Recreational freshwater activities put you at an increased risk. This includes activities that put you in contact with animals or contaminated water or soil for a long time. Some activities that might put you at higher risk include:
Advertisement
Left untreated, severe leptospirosis can lead to:
Healthcare providers diagnose leptospirosis with a physical exam, blood tests and urine (pee) tests. Your provider will ask you about your symptoms, your travel history and whether you could’ve been in contact with anything contaminated. If you’re very sick, you may have a chest X-ray or CT scan.
Your healthcare provider might treat leptospirosis with a week of antibiotics. If you have severe leptospirosis, you’ll stay in the hospital to receive supportive care, like IV fluids.
Contact a healthcare provider if you’ve been in water or soil that could have been contaminated and you have any symptoms of leptospirosis.
Go to the nearest ER if you have symptoms of severe leptospirosis, including:
Advertisement
Most cases of leptospirosis are mild and don’t need treatment. Your healthcare provider will keep a close eye on your symptoms. Don’t hesitate to call 911 or go to the emergency room at the first sign of severe symptoms.
For mild symptoms, a healthcare provider can recommend over-the-counter treatments to help you feel better.
Mild cases of leptospirosis last a few days to a few weeks. If you’re very sick, you can be in the hospital for a few weeks. It can take several months to fully recover from severe leptospirosis.
Yes, most people survive leptospirosis. Most people have no symptoms or have very mild symptoms that go away on their own.
Only about 1% of people with leptospirosis get severely ill with Weil’s syndrome. Weil’s syndrome is often deadly if not treated or if you delay treatment. But if treated quickly, it’s very likely you’ll recover.
The best way to prevent leptospirosis is by not swimming or wading in water that might have animal pee in it. This includes floodwaters. Here are other ways you can reduce your risk:
Advertisement
Leptospirosis is an uncommon disease that usually causes mild symptoms. It causes serious illness in a small number of people. It’s important to know if your job or hobbies put you at risk. But you don’t need to hang up your kayak or work boots just yet. Knowing your risks, taking precautions and recognizing symptoms can help keep you healthy and safe wherever life takes you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Have a virus, fungus or bacteria? Some of these “bugs” won’t go away on their own. Cleveland Clinic’s infectious disease experts are here to help.
