A peritonsillar abscess is a pus-filled pocket that forms near one of your tonsils. It’s usually a complication of tonsillitis and is often caused by the same bacteria that cause strep throat. Symptoms include severe throat pain, swollen tonsils and trouble opening your mouth. Treatments include antibiotics and draining the abscess.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
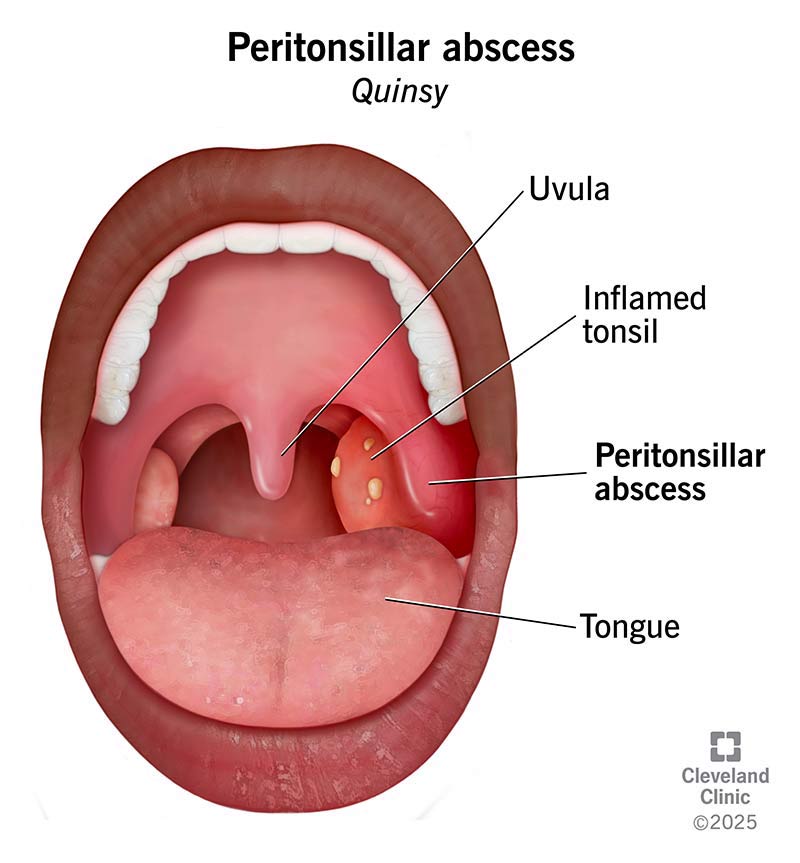
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/peritonsillar-abscess)
A peritonsillar abscess — also called quinsy — is a swollen, pus-filled pocket that forms near one of your tonsils. It’s often a complication of tonsillitis but can also occur on its own. It usually causes an extremely painful sore throat and can make it hard to open your mouth.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A peritonsillar abscess is rare overall, occurring in about 1 in every 10,000 people. But it’s still one of the most common head and neck infections. Abscesses can affect anyone. But they’re most common in older children, adolescents and young adults.
A peritonsillar abscess can be serious, especially if it grows so large that it blocks your throat. This can make it difficult to speak, swallow or breathe. Left untreated, it can become a life-threatening infection.
This is why it’s essential to seek care as soon as possible if you have symptoms.
In most cases, a severe sore throat — usually on one side — is the first sign of a peritonsillar abscess. Additional symptoms often develop over the next few days. Other symptoms include:
The tissue in the back of your throat can become so swollen that it blocks your airway. If you’re having trouble breathing, seek emergency care right away.
In most cases, bacteria cause peritonsillar abscesses. And they’re usually a complication of tonsillitis. This happens when the infection spreads from your tonsil to the tissue around it.
Advertisement
There are also certain factors that can increase your risk for peritonsillar abscesses, like smoking and gum disease. Having a history of peritonsillar abscesses can put you at risk of getting more in the future.
Usually, peritonsillar abscesses are treatable. But the condition can be fatal if swollen tissue blocks your airway. Another concern is that the infection can spread to nearby tissue and even your bloodstream.
It’s essential to see a healthcare provider before things progress to this point.
Your healthcare provider will examine your throat, neck and mouth. Often, they can diagnose a peritonsillar abscess just by looking. They may also do blood tests or take a throat culture. The culture helps them identify the bacteria causing the infection. Most are the same bacteria that cause strep throat.
Your provider may do imaging tests, like an ultrasound or a CT scan. Imaging helps them rule out other conditions that may be causing your symptoms. It also helps pinpoint the location of the pus-filled pocket, so they can get rid of it.
In most cases, a peritonsillar abscess needs surgical drainage and antibiotics. If you still have your tonsils, you might need surgery to remove them. Treatments include:
Other treatments depend on how severe your condition is. For example, if your throat hurts so much that you’re unable to swallow liquids, you may need IV fluids to treat dehydration.
Most people start to feel better within the first 24 hours of treatment. Full recovery usually takes about a week after surgical drainage.
You’ll likely take antibiotics by mouth for about two weeks. You’ll need to take your meds exactly as prescribed until you finish them. It’s important to take them even if you start to feel better.
You’ll likely have a follow-up appointment shortly after treatment or after being discharged from the hospital. Your provider will check to see if your symptoms are improving. In the meantime, let them know about new or worsening symptoms.
Advertisement
If you have a peritonsillar abscess, you may only need treatment during an office visit with your healthcare provider. But if you have severe swelling that blocks your airway, you may have the abscess drained in the hospital. Although it’s uncommon, you may need an emergency tonsillectomy (quinsy tonsillectomy). If so, you’ll probably need to stay in the hospital for a few days.
Your provider may use a combination of treatments to ensure you feel better as soon as possible.
There are lots of ways to support the healing process and feel better during recovery:
The best way to prevent peritonsillar abscess is to treat oral infections promptly. This includes tonsillitis. Early treatment can keep the infection from spreading.
Advertisement
You can also reduce your risk with good oral hygiene and by not smoking, vaping or using tobacco, in general.
Tonsillitis is an infection of your tonsils. A peritonsillar abscess is an area of pus-filled tissue next to your tonsils. A peritonsillar abscess is often a complication of tonsillitis. But this isn’t always the case.
A severe sore throat can be a red flag of a peritonsillar abscess. You may feel dread when your mouth waters because you know swallowing will hurt. Your throat may be so swollen that you can’t open your mouth all the way.
These symptoms may be a sign of peritonsillar abscess or other serious conditions affecting your throat. Regardless, if it takes effort to breathe or feels like you’re not getting enough air, seek emergency care immediately.
Peritonsillar abscesses are treatable. But they’re serious enough that you should never delay care. The sooner the abscess is drained and you’re on antibiotics, the better you’ll feel. Sometimes, the best option is to remove your tonsils altogether. If you have symptoms of a peritonsillar abscess — especially along with a history of tonsillitis — see a healthcare provider right away.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Not just kids need a tonsillectomy. Adults who have frequent sore throats or snore a lot get them, too. Cleveland Clinic is here to help.
