Meniscus tears are a very common knee injury, especially among athletes. Sudden, twisting movements — like pivoting to catch a ball — can tear the cartilage in your knee. People with arthritis in their knees are also more prone to meniscus tears.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
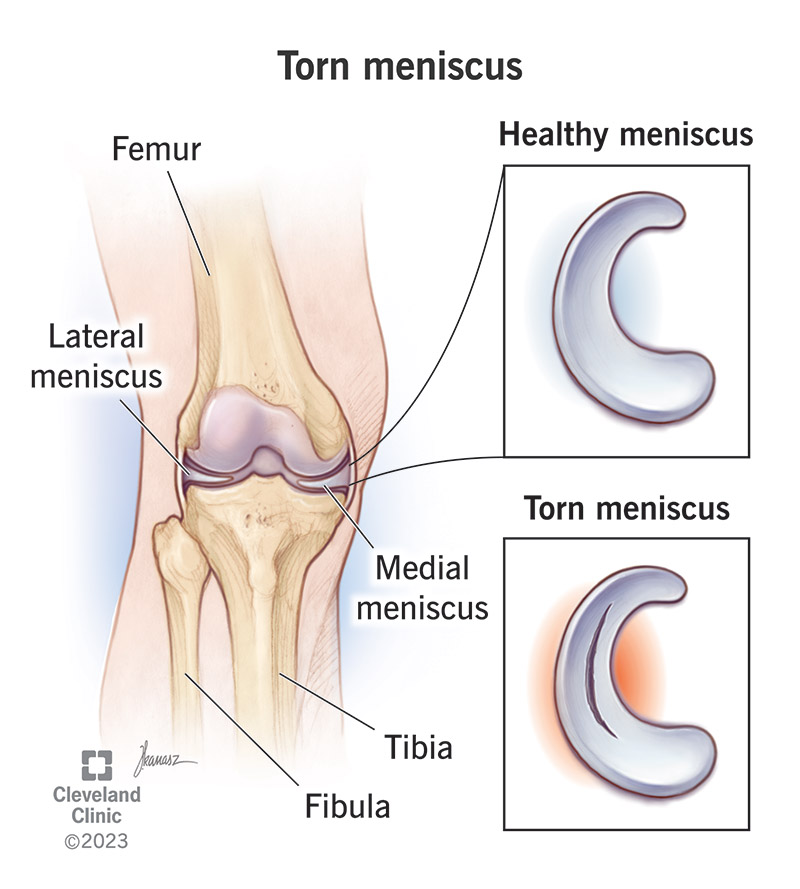
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/torn-meniscus.jpg)
A torn meniscus is a tear in the tough cartilage inside your knee. Two pieces of cartilage sit inside your knee between your thighbone (femur) and shinbone (tibia). This cartilage is the meniscus. The rubbery wedges of cartilage act like shock absorbers for your knee, providing cushioning for your bones and knee joint. It can tear after a hard twist or rotation of your knee.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
As you get older, the cartilage in your knees wears down and gets weaker. This thinner cartilage can tear more easily. Arthritis (a breakdown of cartilage in the joints) can also lead to a meniscus tear. It’s also a common sports injury in people who play sports, even in children and teenagers.
Each of your knee joints has two menisci:
A torn meniscus is a very common sports injury. Often, athletes and people who play sports for fun get meniscus tears. The injury also commonly affects older people and those with arthritis in their knees. Meniscal tears affect 61 out of every 100,000 people in the U.S.
People who tear a meniscus often feel like something has popped in their knees at the time of the injury. Other meniscus tear symptoms include:
At first, you might be able to bear weight on your injured leg. But your knee will start to swell and become more and more painful over the span of a few days.
Advertisement
Acute meniscus tears occur during a sudden motion in which your knee twists while your foot stays planted on the ground. The tear frequently occurs while playing sports. People whose cartilage wears down (due to age or arthritis) can tear a meniscus from a motion as simple as stepping on an uneven surface. Sometimes, degeneration from arthritis causes a tear, even without a knee injury.
People who play sports (like tennis, soccer, basketball or football) that involve sudden, twisting movements are most likely to tear a meniscus. Playing contact sports also increases your risk of a meniscus tear. Getting hit or tackled can make you twist your knee, tearing the cartilage. But degenerative meniscus tears from wear and tear of your cartilage over time are common no matter your activity level.
If your meniscus tear doesn’t heal properly, you may have continued pain and discomfort in your knee. Meniscus injury can also speed up the wear and tear on your knee joint, increasing your risk for osteoarthritis.
Your healthcare provider will physically examine your knee, looking for signs of swelling. They’ll test your range of motion using a McMurray test or Thessaly test. You may also get imaging tests, like X-rays or an MRI (magnetic resonance imaging), to assess the damage.
Your provider may recommend knee arthroscopy to better view and accurately diagnose your injury. During this procedure, the surgeon inserts a tiny camera (called an arthroscope) through a small cut (incision) and into your knee.
Depending on the size and location of your meniscus tear, it may heal without surgery. Your healthcare provider may recommend taking a nonsteroidal anti-inflammatory (NSAID) medicine (like ibuprofen or aspirin) to relieve pain and reduce swelling. In the days after your injury, you should also follow the RICE method. RICE stands for rest, ice, compression and elevation:
Your provider may also recommend working with a physical therapist to strengthen your knee and increase your range of motion.
More serious meniscus tears may not heal on their own. If your injury doesn’t improve with RICE, NSAIDs and physical therapy, your healthcare provider may recommend meniscus surgery. This is a minimally invasive surgery with little downtime. It’s one of the most common orthopedic surgeries in the U.S.
Advertisement
Surgery is a very effective way to repair a torn meniscus. If the tear is too big to repair, your surgeon may remove all or part of the meniscus. After recovery, you’ll be less likely to develop additional knee problems.
Most people who tear a meniscus can return to full activity. If you have surgery to repair a torn meniscus, your knee should be fully recovered after a few months of physical therapy.
If you have surgery to remove all or part of your meniscus, you may be at a higher risk of developing arthritis down the road. That’s because you now have less shock absorption in your joint. Over time, the joint can break down.
It can be hard to prevent an accidental injury. But you can reduce your risk of a torn meniscus if you:
You should call your healthcare provider if you:
Advertisement
You may want to ask your healthcare provider:
A knee injury like a torn meniscus can be painful — and frustrating. It can slow you down and keep you from exercising, playing sports or even just walking around the house. Small tears often heal on their own, while others may require arthroscopic surgery. Work with your healthcare providers to develop a treatment and rehabilitation plan that gets you back to your favorite activities — without pain — safely. Most people fully recover from a torn meniscus.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Whether you have knee pain from a sports injury or another reason, there’s relief in sight. Cleveland Clinics offers personalized meniscus tear treatment.
