Group B strep (GBS) is a bacterial infection that lives in your vagina or rectum. You can pass it to your baby during childbirth. If a newborn gets group B strep, it can cause serious complications. You’ll be screened for the infection in the third trimester. Antibiotics can treat GBS if you test positive. This protects your baby from getting it.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
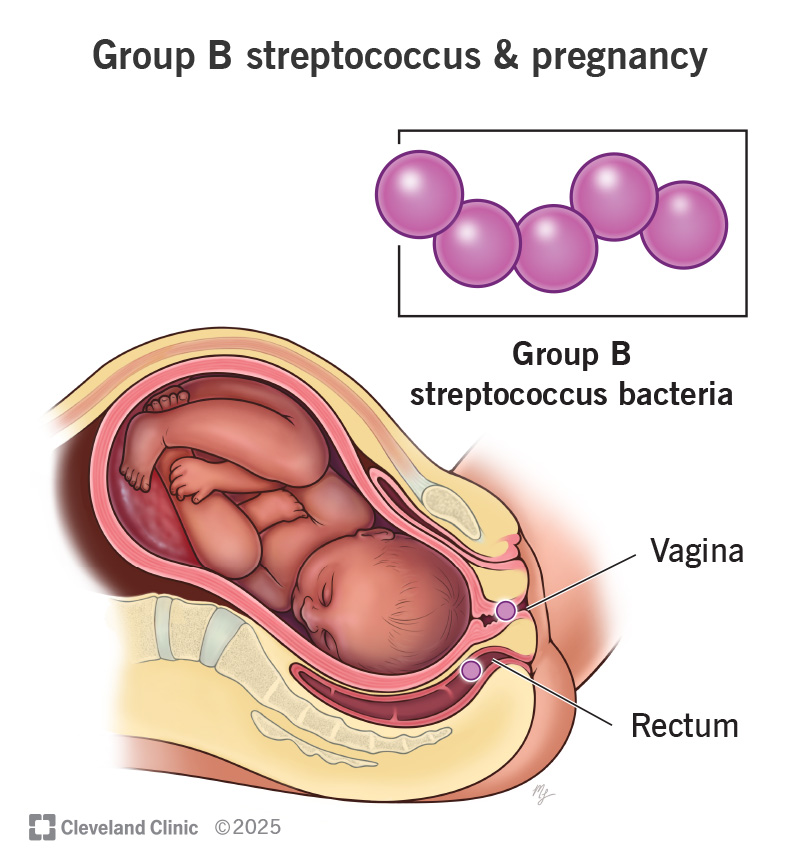
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/group-b-strep)
Group B strep (group B streptococcus or GBS) is a type of bacteria that typically lives in your vagina, intestines and rectum. GBS doesn’t cause problems in most healthy adults. But if you’re pregnant, you can pass it to your baby during a vaginal delivery. Group B strep can be harmful to newborns because they lack immunity against the bacteria.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
For this reason, healthcare providers screen for group B strep between 36 and 37 weeks of pregnancy. Group B strep testing involves your provider taking a swab of your vagina and rectum. If you test positive, you’ll receive antibiotics during labor and delivery. This almost always prevents you from passing the infection to your baby. About 1 in 4 females test positive during pregnancy.
Even though group B strep is mostly known for causing illness in newborns, adults with suppressed immune systems can also get sick from the infection.
Most adults don’t have symptoms of group B strep. It can cause symptoms in people with certain health conditions, but this is rare. These symptoms include:
Symptoms can become serious quickly for newborns. Some symptoms include:
Most babies show symptoms within the first few hours and days after birth. This is called early-onset GBS and is more common and more serious. But some infants don’t show symptoms until one week to three months later. This is called late-onset GBS. It’s less common and usually less severe.
Advertisement
Streptococcus agalactiae causes group B strep. These bacteria naturally occur in certain parts of your body. Experts aren’t entirely sure how the bacteria spread, but they know that they’re potentially harmful in babies and people with weaker immune systems.
It’s not a bacterial infection you get from poor hygiene or from sharing food or drinks with an infected person. Other people who live with you, including other children, aren’t at risk of getting GBS from you. GBS isn’t a sexually transmitted infection (STI).
Anyone can test positive for GBS during pregnancy. If you test positive and don’t receive antibiotic treatment, there’s a chance you could pass it to your baby.
These factors also increase your risk of having a baby with group B strep:
Taking antibiotics during labor is the best way to lower your baby’s risk of infection. Your provider will usually give you antibiotics if your test results aren’t back yet, especially if you have any risk factors.
Group B strep infection can lead to life-threatening illnesses like:
Most infants don’t develop any long-term complications. But, about 1 in 4 infants with meningitis from GBS develop:
Your healthcare provider will test you for GBS around 36 to 37 weeks of pregnancy.
Your obstetrician uses a cotton swab to obtain samples of cells from your vagina and rectum. This test doesn’t hurt and takes less than a minute. Then, the sample is sent to a lab to check for group B strep. If you’re using a midwife, you might be given instructions on how to test yourself at home and submit the swab to a lab.
Most people receive their results within 48 hours. A positive result means you’re GBS positive. But this doesn’t mean you or your baby will get sick. Testing positive means your healthcare provider will want to give you antibiotics during labor and delivery. This greatly reduces the chance that you’ll pass GBS to your baby.
Healthcare providers prevent GBS infection in your baby by treating you with intravenous (IV) antibiotics in the hospital. The antibiotics work best when given at least four hours before delivery. It’s not effective to treat GBS before labor begins. The most common antibiotic to treat group B strep is penicillin or ampicillin. With antibiotic treatment, about 1 in 4,000 babies will get a GBS infection at birth. If you don’t receive antibiotics during labor, your chances of passing the infection to your baby are about 1 in 200.
Advertisement
One exception to the timing is when GBS is found in your pee. When this is the case, oral antibiotic treatment begins right away (regardless of the stage of pregnancy). You’ll still receive antibiotics through an IV during labor.
Anyone who’s previously given birth to a baby who developed a GBS infection or who’s had a urinary tract infection in this pregnancy from GBS will also receive antibiotics during labor.
Some babies still get GBS infections despite testing and antibiotic treatment. Your healthcare provider might take a sample of your baby’s blood or spinal fluid to see if they have GBS infection. If they do, they’ll get treatment with antibiotics through an IV.
Talk to your provider about what you can expect during labor and delivery if you have group B strep. It’s important to remember that you’ll need treatment with IV antibiotics for at least four hours before your child is born. In most cases, your pregnancy care team can make sure this happens.
No, you don’t need antibiotics if you’re having a C-section delivery. But you’ll still be tested for GBS during pregnancy. This is because labor could start before your scheduled C-section. If your water breaks and you’re GBS positive, your baby is at risk of getting the infection.
Advertisement
Once you test positive for GBS, you’re considered positive for the rest of your pregnancy. Nothing in your pregnancy will change until you’re in labor. Your healthcare team will need to make sure you receive antibiotics for at least four hours before your baby can be born. This prevents you from passing GBS to your baby. It’s OK to remind your care team that you’re GBS positive when you get to the hospital.
Even if you receive antibiotic treatment, your baby’s pediatrician will check them for signs of infection.
No. The bacteria naturally live in about 25% of adults. They usually don’t cause health problems.
Try not to panic if your healthcare provider tells you you’re positive for group B strep during pregnancy. Bacteria that live naturally in your body cause it, not anything you did. Your provider will give you antibiotics during labor through an IV in your arm. The chances of passing group B strep to your baby are very low. Talk to your provider about group B strep and share any concerns you have about testing positive.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Trying to choose where to give birth? Learn why Cleveland Clinic is the best choice to help you through each step of the labor and delivery process.
