An overgrowth of the fungus Candida causes a vaginal yeast infection. A vaginal yeast infection causes the skin around your vagina to burn and itch, and it may change the consistency of your vaginal discharge. Treatment includes antifungal medication.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
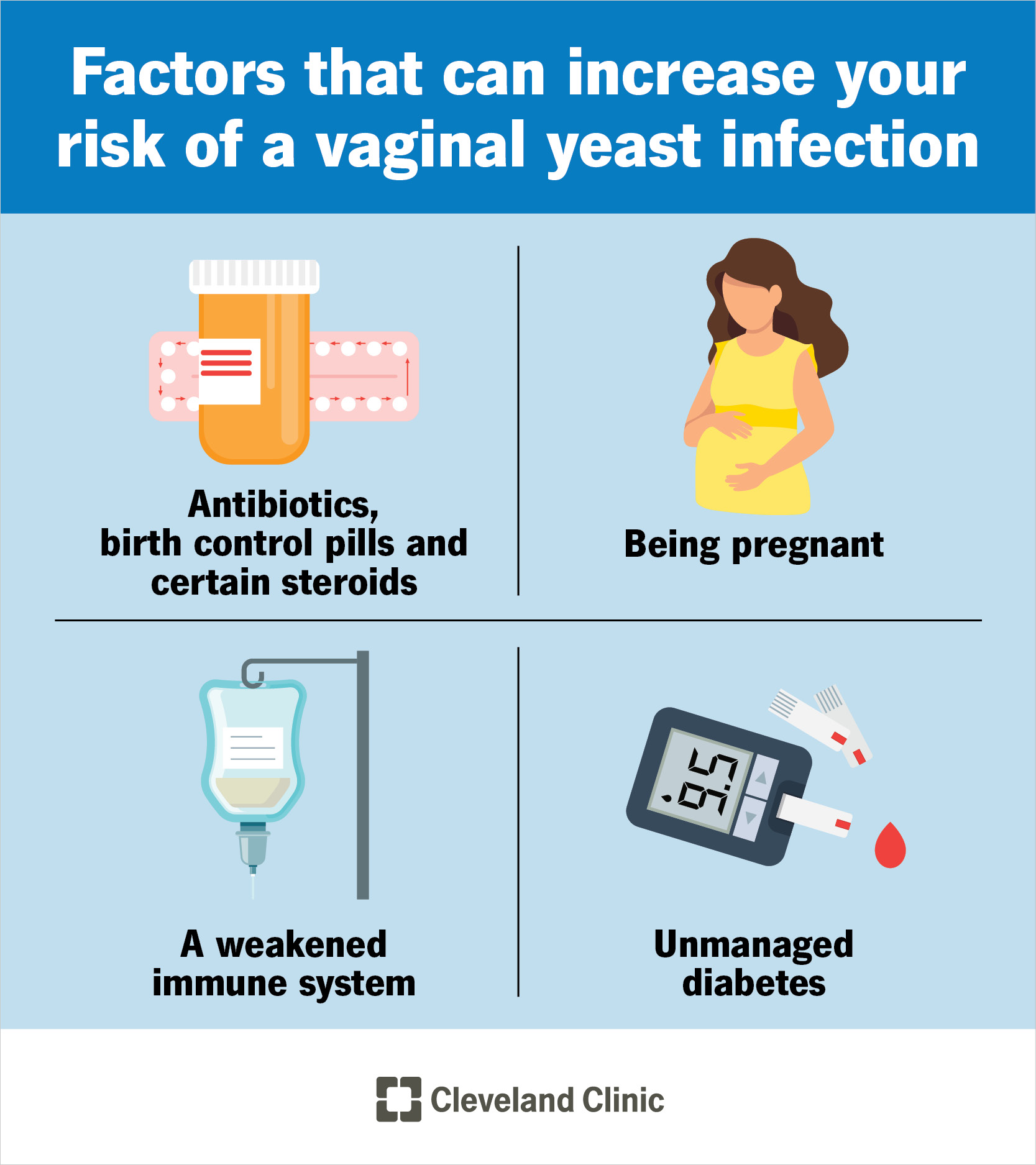
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/5019-vaginal-yeast-infection.jpg)
A vaginal yeast infection happens when a fungus called Candida grows too much. Candida usually lives in your body without causing problems. But when it’s out of balance, it multiplies quickly and leads to a yeast infection.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A yeast infection can cause burning, itching and redness in your vulva and changes to your vaginal discharge. It isn’t a sexually transmitted infection (STI).
Another name for a vaginal yeast infection is vaginal candidiasis. Up to 3 in 4 women will have a yeast infection at least once in their lives. About half of all women will get two or more. They’re most common after puberty and before menopause.
Common signs of a yeast infection include:
Symptoms of a yeast infection can feel like symptoms of other conditions that affect your vagina. Contact a healthcare provider if you have any of these symptoms so they can examine you.
An overgrowth of a fungus called Candida causes a vaginal yeast infection.
Fungus lives in several places within your body. It’s supposed to be there. Other bacteria help keep its growth under control. But certain factors throw off this balance. When this happens, Candida multiplies out of control. This leads to a yeast infection.
Advertisement
Some specific causes are:
Other things that increase your risk:
Yeast infections aren't considered contagious, but in rare cases, you may pass one to a female partner. It’s uncommon to pass it to a male partner.
Your healthcare provider may suspect a yeast infection after hearing your symptoms. They may need to take a sample of discharge from your vagina to confirm a yeast infection, though. The combination of your symptoms and the discharge sample will tell your healthcare provider what type of yeast infection you have and how to treat it.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_6bwvracg/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
How you should treat a vaginal yeast infection.
Antifungal medications treat most vaginal yeast infections. They work by fighting yeast overgrowth in your body. Medications are either oral (usually given in one dose of fluconazole by mouth) or topical (used daily for up to seven days). You may apply topical medications to your vulvar area or place them inside your vagina (suppository) using an applicator. Some common antifungal medications are miconazole (Monistat®) and terconazole.
Your healthcare provider will prescribe the best treatment based on your symptoms and how serious the infection is. Your healthcare provider will give you information about each form of medication and directions on how to use each one properly. You should finish the medication completely to make sure the infection doesn’t come back.
If you’re taking medication for a yeast infection, you shouldn’t have sex until you’re finished with treatment. Sex can cause more irritation, and certain antifungal medications can weaken the materials used in condoms and diaphragms.
Sometimes, you can treat a vaginal yeast infection with over-the-counter medicines. But you may want to avoid this if you aren’t completely sure you have a yeast infection. It’s usually best to talk to a healthcare provider to make sure you’re buying the right medicine.
Advertisement
Most yeast infections clear up with medication after a few days, but it may take a full week. More severe cases may last longer and take longer to treat. Make sure you use the medication as directed and don’t stop taking it too soon, or the infection may come back.
No, a yeast infection can’t go away on its own. Only a medication that destroys fungus will treat a vaginal yeast infection.
Talk to your healthcare provider if you get more than four yeast infections in a year. They may want to order tests to determine what’s causing them. Your provider will use your test results to make sure you receive the right treatment. Managing the reason for the infection can help prevent future vaginal yeast infections.
You can often prevent vaginal yeast infections by making a few lifestyle changes. These changes can include:
Yeast infections are a very common fungal infection that most women will have in their lifetime. It’s highly treatable with medication, some of which are available for purchase at your local drug store without a prescription. Even though you may know the signs of a vaginal yeast infection, it’s important to get examined by your healthcare provider. They can recommend the best treatment based on the type of yeast infection you have and how severe it is.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have vaginitis, getting relief from your discomfort is probably top of mind. Cleveland Clinic’s experts can craft a treatment plan that works for you.
