Allergic asthma is a breathing condition where the airways you breathe through tighten when you inhale an allergen. Common allergens include pollen, dander and mold spores. This type of asthma is very common in both children and adults. Symptoms of allergic asthma can include shortness of breath, coughing, wheezing, stuffy nose, itchy eyes and a rash.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
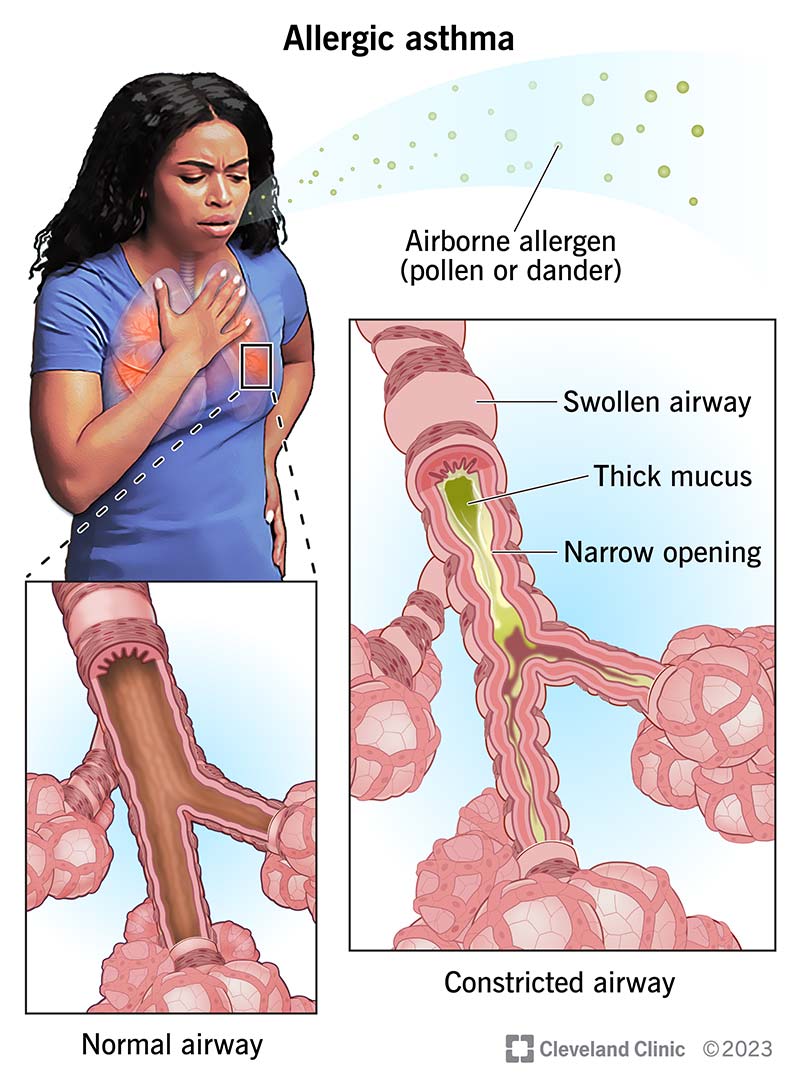
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/allergic-asthma)
Allergic or allergy-induced asthma is a condition where your airways tighten when you breathe in an allergen. Most often, these allergens are in the air — like dust mites, pollen, animal dander or mold spores.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
When you have allergies, your body creates a response to something it thinks is a threat — the allergen. Your immune system fires up all of its defenses to try and fight off this danger. Your immune system releases various chemicals that cause inflammation, or swelling, and squeezing of your airways upon exposure to an allergen.
Allergic asthma is the most common type of asthma. In the United States, about 25 million people have asthma. Out of that group, approximately 60% have allergies.
If you have allergic asthma, you may have many of the same symptoms you’d experience with other types of asthma. These symptoms can include:
Allergen exposure can also trigger other symptoms, including:
Allergy-induced asthma symptoms can range from mild respiratory symptoms to severe asthma attacks. During an asthma attack, your airways will tighten, making it difficult to breathe. You may also feel chest pressure, wheeze and cough. The symptoms of an allergic asthma attack are the same as an asthma attack caused by something else. The difference between the two is the cause of the asthma attack.
Advertisement
Allergens can be all around you — in your indoor and outdoor environments. When you have allergic asthma, inhaling these allergens can set off (trigger) your symptoms. It’s important to know what can trigger your asthma so that you can manage your condition.
Possible allergens that can trigger allergic asthma include:
Food allergies may trigger allergic asthma in some people. Food allergies are rarely the cause of allergic asthma alone.
You’re more at risk of having allergy-induced asthma if you have allergies or a family history of allergies.
Allergy-induced asthma can be serious and cause complications. Some of the most common complications of allergic asthma include:
Your healthcare provider will order tests to determine if you have allergic asthma. The two most common tests are spirometry and bronchoprovocation testing:
Advertisement
If your provider determines you have asthma, they’ll recommend either a blood test or skin test to help determine if environmental allergens are potential triggers for your asthma.
During a skin test, a provider puts small drops of liquid containing various allergens on your skin. Then, they gently scratch your skin to allow allergens to enter the top layer. If you’re allergic to the substance, your skin will react by swelling or you may develop tiny, raised bumps.
In certain cases, a blood test can identify allergic triggers. Allergy blood tests can miss a small percentage of allergies compared to skin testing.
Your healthcare provider will work with you to treat both your allergies and your asthma. Some treatments work for asthma, while others treat just allergies, and some treatments can help manage both conditions. Treatment can involve avoiding the allergen or making lifestyle changes, and medications.
Your provider will help you figure out what’s triggering your asthma and find ways to either avoid or manage these allergens. Often, these triggers are in your environment. Once you know what they are, you can manage your interactions with them. This might mean hiring someone to cut your grass if you know that pollen is a trigger for your asthma, or avoiding places with a lot of animals if dander is a trigger for you.
Advertisement
Depending on what triggers your asthma, other steps you can take include:
Medications for allergy-induced asthma may include:
Advertisement
There isn’t a cure for allergic asthma. However, symptoms can get better or worse depending on your environment and exposures.
While asthma itself can’t be prevented, you can reduce your risk of an allergic asthma attack by understanding and avoiding triggers and ensuring you’re using the best medical treatment to manage your asthma.
Contact your healthcare provider if you have asthma symptoms due to allergens so they can work on a treatment plan with you. Symptoms may include:
If you’re having a severe asthma attack and either don’t have an inhaler or your symptoms aren’t improving after using it, go to the nearest emergency department or call 911 (or your local emergency service number). People experiencing an allergy can also go into anaphylaxis, which is a life-threatening allergic reaction.
Allergic asthma is a very common condition that many people experience throughout their lives. Though there isn’t a cure for this type of asthma, you can take steps to manage it. Learn about your triggers and try to avoid those triggers. Talk to your healthcare provider about ways to manage your environment and avoid asthma attacks. If you feel your asthma isn’t under control, please seek help to find a treatment plan that best works for you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
You might feel anxious when your child gasps and wheezes. Cleveland Clinic Children’s asthma experts are here to help them (and you) breathe easier.
