Celiac disease causes inflammation in your small intestine when you eat gluten. If you eat it a lot, the constant inflammation can damage your intestine. It can make it hard to get enough nutrients from your food. Fortunately, eating gluten-free foods can often reverse the damage.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
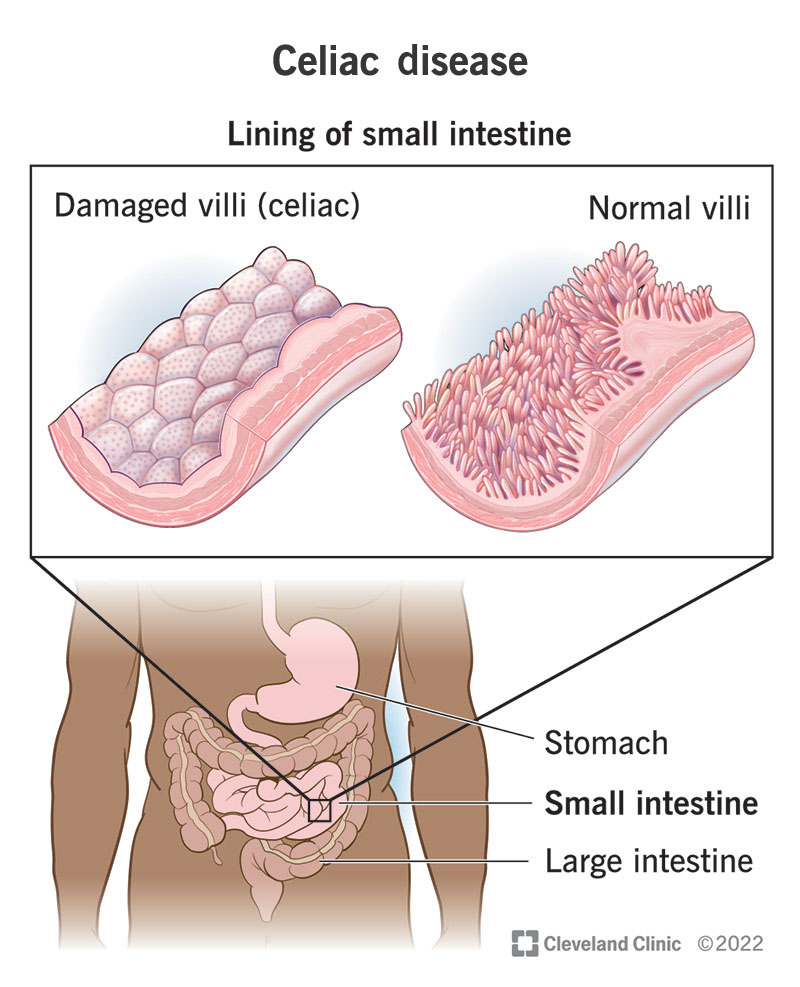
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/14240-celiac-disease.jpg)
Celiac disease is an inherited autoimmune disease. It causes a reaction in your body to a protein called gluten. When you eat gluten, it triggers an abnormal response from your immune system. Your immune system attacks the gluten in your digestive system, causing inflammation. Inflammation damages the inside of your small intestine. This makes it harder for your intestine to absorb nutrients from your food.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Gluten is found in grains like wheat, barley and rye. These grains make up many of the staple foods of the standard Western diet. These include bread, cereals, pasta and beer. Gluten is also added to many food products that you wouldn’t expect. These include sauces, soups and packaged foods. If you have celiac disease, it’s important to eat gluten-free.
Damage to your small intestine can cause serious complications. This is where most of the nutrition in your food gets absorbed. Severe damage can prevent your intestine from doing its job. If celiac disease goes untreated, it can lead to malabsorption and malnutrition. Malnutrition has many serious side effects, especially in children. Children with celiac disease may have growth and development delays.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_sxyjai9r/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Symptoms vary widely and require a gluten-free diet for management.
Signs and symptoms of celiac disease can appear at any age. Healthcare providers most often see it develop during two distinct age windows:
Symptoms of celiac disease vary widely. This can make it hard to recognize. Some people don’t notice any symptoms at all. Some experience indigestion or other GI symptoms after eating gluten. Others only begin to see signs of nutrient deficiencies later on, when real damage has been done. In these cases, symptoms of anemia may be the first to appear.
Advertisement
You might have:
Gastrointestinal symptoms, like:
Symptoms of iron-deficiency anemia, like:
Other symptoms of malnutrition, like:
Dermatological symptoms:
Around 15% of people with celiac disease develop a condition called dermatitis herpetiformis. This is an itchy rash that looks like clusters of bumps or blisters. It affects your elbows, knees, butt and scalp.
Celiac disease is an autoimmune disease. That means it happens because your immune system reacts abnormally. This abnormal reaction to gluten develops in people with certain genetic changes (variants). You inherit these changes from your biological parents. Almost everyone with celiac disease has one of these gene changes (HLA-DQ2 or HLA-DQ8). But not everyone with these genes develops celiac disease.
Most autoimmune diseases, like celiac disease, are partly genetic. But other factors are involved in triggering the disease. Experts aren’t sure what all these factors are. Some suggest that the balance of microorganisms living in your gut might play a part. Others suggest that a major physical event, like an illness or surgery, might trigger it later in life. More research is needed to explore these theories.
You’re more likely to develop celiac disease if you:
If celiac disease goes untreated, it can cause complications. Some of these include:
Advertisement
You might suspect you have celiac disease if you have symptoms after eating gluten. Many people appear to have a sensitivity to gluten or wheat products in what they eat. Food intolerances can cause discomfort that mimics celiac disease. But they don’t damage your small intestine the way celiac disease does. To diagnose celiac disease, a healthcare provider will look for evidence of this damage.
Healthcare providers use two methods of testing for celiac disease. They prefer to use both together to confirm the diagnosis:
Your provider may also want to test your blood for nutrient deficiencies. Severe deficiencies can have wide-ranging effects on your body. You may need nutrition therapy to treat them. Common findings include:
The first and most important step in treating celiac disease is to stop eating gluten. You can’t change the way your body reacts to gluten. But you can prevent gluten from triggering that reaction. When you stop eating gluten, your small intestine will begin to heal. It will soon be able to absorb nutrients again. But you have to be strict about not eating gluten — for life — or you could hurt your small intestine again.
Advertisement
Additional treatments may include:
Most people say their symptoms improve almost immediately after starting to eat gluten-free. It may take several weeks to reverse your nutrient deficiencies. It may take several months for your gut lining to fully heal. It can take longer, in some cases. It depends on how damaged your gut is and how long the damage has been going on. Eating any amount of gluten (however small) can also delay healing.
Most people who stop eating gluten have an excellent prognosis. Most of the damage done by celiac disease can be undone. If you continue to have symptoms, it may be that you’re consuming small amounts of gluten without realizing it. It’s also possible you have another condition. A small percentage of people have a type of celiac disease that doesn’t respond to standard treatments.
Avoiding gluten in all its forms can be daunting at first. You’ll have to learn to read labels carefully. You’ll need to watch out for gluten that sneaks into foods. The good news is that there are many resources available to help you. Your healthcare provider will refer you to a registered dietitian to get you started. There are also many dedicated support groups and references online.
Advertisement
It might help to:
A celiac disease diagnosis will change your life forever. It might seem hard at first. But this change is for the better. Before diagnosis, you didn’t know you needed to avoid gluten. You didn’t know what it was doing to your small intestine. You may have had strange and uncomfortable symptoms for years without understanding why. Now that you know, the power is in your hands to restore your health.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If celiac disease gets in the way of your everyday life, Cleveland Clinic’s experts can help. We can craft a treatment plan that’s specific to you.
