Hemophilia is a rare inherited condition that causes prolonged bleeding. It happens when you don’t have enough proteins (clotting factors ) in your blood, so your blood doesn’t form clots. The condition can be life-threatening if you have severe internal bleeding. Gene therapy and other newer treatments can prevent or reduce bleeding.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
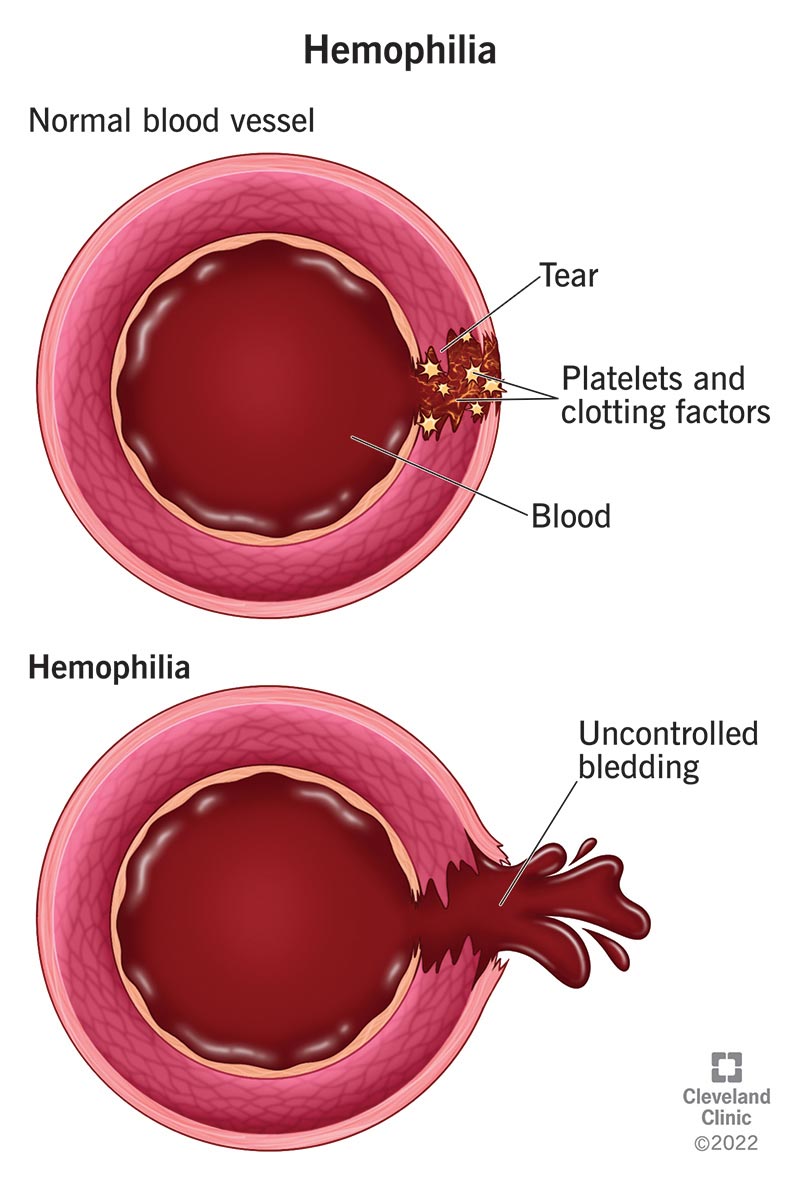
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/14083-hemophilia)
Hemophilia is a rare blood disorder that keeps your blood from clotting. If you have hemophilia, a minor injury may cause you to bleed a lot. You might bruise easily. It can cause life-threatening internal bleeding.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This condition most often happens when you inherit certain genetic changes that keep your body from making clotting factors. These are proteins that help your blood form clots.
Healthcare providers classify hemophilia as being severe, moderate or mild. They base the classification on the number of clotting factors in your blood. There’s no cure for it, but newer treatments prevent or reduce how often you experience bleeding that hemophilia causes.
The types of this condition are:
The most common symptoms are unusual or excessive bleeding or bruising. How much bruising or bleeding you experience depends on whether you have a severe, moderate or mild form of the condition. Common symptoms include:
Advertisement
Very rarely, severe hemophilia causes bleeding into your brain. This is a life-threatening condition. Symptoms are persistent headaches, double vision or feeling very tired. If you have hemophilia and have these symptoms, get medical care right away.
The condition most often happens because you inherit changed genes from your biological parents. Genes carry the clotting factor instruction manual. When genes change, they don’t make enough clotting factor, and your blood doesn’t clot. People inherit the change in an X-linked recessive manner. Here’s how that happens:
A spontaneous gene change may cause hemophilia. This means you don’t inherit the disease. Instead, the gene change happens during fetal development when cells divide and make copies of themselves. Mistakes or changes can happen during the gene-copying process.
The condition doesn’t always involve changed genes. Healthcare providers call this acquired hemophilia. It develops when autoantibodies attack clotting factor 8. Autoantibodies are proteins your immune system makes that attack healthy cells, tissue and proteins.
The most significant risk factor is if your biological father has hemophilia or your biological mother carries the changed gene that causes it.
This condition can affect your quality of life and your health. Complications of hemophilia include:
Another complication of this condition is hemophilia with inhibitor. This is a side effect of replacement therapy, a common hemophilia treatment. Some people develop antibodies (inhibitors) that keep treatment from working like it should.
A healthcare provider will do a physical exam. They’ll ask about your health and if anyone in your immediate family has this condition. They may do the following tests:
Advertisement
Your treatment will depend on your situation. For example, people with severe forms of hemophilia A or hemophilia B may have replacement therapy. You receive human plasma concentrates or lab-made clotting factors. These boost your clotting factor levels. Replacement therapy may prevent bleeding or slow it down.
Newer treatments are:
Advertisement
Your provider may tell you to avoid pain medications — like aspirin, ibuprofen and naproxen — which keep your blood from clotting. You should also avoid anticoagulants such as heparin or warfarin.
Contact your healthcare provider if you notice changes in your body, like increased bleeding or bruising. If you have hemophilia, go to the emergency room right away if you:
Hemophilia is a chronic disease. You’ll need medication and other medical care for the rest of your life. But newer treatments mean you may have nearly the same life expectancy as someone who doesn’t have the condition.
Hemophilia can disrupt every aspect of your daily life, leaving you feeling frustrated and anxious. Here are suggestions that might help:
Advertisement
If you have hemophilia, minor injuries that other people shrug off can cause major health issues for you. Bumping your knee against a table leg can set off internal bleeding that makes your joints ache. A hard sneeze can trigger a bloody nose that nothing can stop. In short, the condition can disrupt your days (and nights).
Fortunately, there are treatments that reduce bleeding and how often you experience it. Hemophilia is a rare disease, and you may feel like most people don’t understand what you go through every day. Remember that you’re not alone. Your healthcare team is here to support you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have a lifelong bleeding disorder like hemophilia, you want the best care. Cleveland Clinic has the support and treatments you need.
