Inhalers are small, handheld devices that allow you to breathe medicine in through your mouth, directly to your lungs. Types include metered-dose, dry powder and soft mist inhalers. They usually treat asthma and COPD but providers may prescribe them for other conditions. Bronchodilators and corticosteroids are common inhaled medications.
An inhaler is a small, handheld device that delivers medication directly to your lungs. Inhalers can be dry powder, metered-dose or soft mist. The most common types use medicine that helps open your airways or reduce inflammation in your lungs.
Inhalers and nebulizers both deliver medicines that treat lung conditions. But an inhaler is a handheld device that doesn’t need electricity. It usually delivers dry powder or a spray of medication, though some use a soft mist of liquid medication.
Nebulizers are larger and use a battery or you plug them in. You use them with a mask or mouthpiece. Nebulizers deliver the medicine over several minutes, rather than in one breath.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
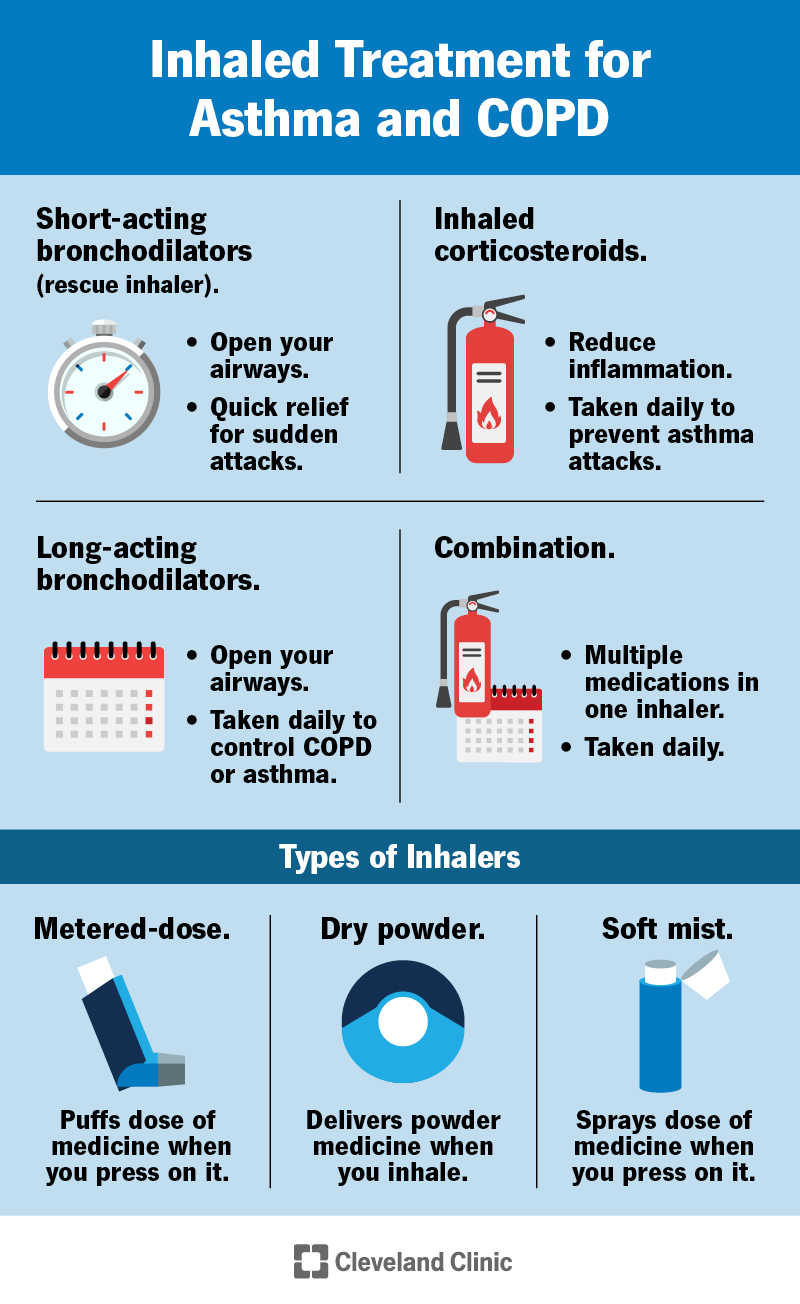
People with chronic lung conditions that affect their breathing, like asthma or chronic obstructive pulmonary disorder (COPD), most commonly use inhalers. You use daily inhalers to prevent or manage your symptoms and fast-acting inhalers (rescue inhalers) during an asthma attack or COPD exacerbation (times when your breathing gets worse).
Yes, providers prescribe rescue inhalers and inhaled corticosteroids for respiratory conditions other than asthma. As with any medication, you should only use an inhaler that’s prescribed for you.
Inhaled medications most commonly treat asthma and COPD. Providers sometimes prescribe them to treat respiratory infections like bronchitis. Providers also use them to treat:
Providers often prescribe inhaled corticosteroids (ICS) to prevent asthma symptoms, along with a rescue inhaler for quick relief of attacks. If ICS medications don’t help manage your asthma, your provider may add a long-acting bronchodilator, like a long-acting beta-agonist (LABA) or a long-acting muscarinic antagonist (LAMA).
Common inhalers to manage COPD include combinations of LABA, LAMA and/or inhaled corticosteroids. Examples include:
Providers also prescribe a rescue inhaler for exacerbations (times when your breathing gets worse).
Types of inhaler devices include pressurized metered dose inhalers (pMDIs), dry powder inhalers (DPIs) and soft mist inhalers.
Metered dose inhalers (MDIs or pMDIs), sometimes called “puffers,” hold the medication in a pressurized canister. The canister sits in a handheld container with a mouthpiece. When you press on the canister, a propellant (something that helps the medicine move out of the canister) helps send a puff of medicine out of the mouthpiece. Following the directions, you breathe the puff in through your mouth to pull the medicine into your lungs. MDIs deliver one dose at a time from a canister that holds multiple doses.
Dry powder inhalers (DPIs) store medicine as a powder inside capsules or other containers that you activate when you’re ready to use the inhaler. Unlike MDIs, a propellant doesn’t push the medicine out of a DPI. Instead, you use a quick, deep breath to pull the powder out and into your lungs.
DPIs are usually tube- or disk-shaped, with a mouthpiece. Some have a place to load in medicine. Different styles and brands have different instructions on how to activate and use them. Some examples of dry powder inhaler devices include:
Soft mist inhalers (Respimat®) turn liquid medicine into a fine mist. You breathe the mist in through your mouth to get the medicine to your lungs.
Types of medications in inhalers for respiratory conditions include those that provide quick relief during an exacerbation or an attack, and those that you take regularly to manage symptoms or prevent attacks. These include short-acting bronchodilators, long-acting bronchodilators and inhaled corticosteroids.
Inhaled corticosteroids (ICS) reduce inflammation in your lungs. You use them daily to prevent asthma attacks. Sometimes, providers also prescribe them for COPD or other lung conditions. They usually come in a dry powder inhaler. Examples of ICS medications include:
Short-acting bronchodilators are inhalers that you use during an asthma attack or an exacerbation of COPD when you’re having severe troubling breathing. They’re often called rescue inhalers. They help you breathe again quickly but the effects only last a few hours, so they’re not for managing your condition long-term.
Bronchodilators in rescue inhalers include short-acting beta-agonists (SABAs) and short-acting muscarinic antagonists (SAMAs or anticholinergics). They both work by relaxing the muscles in your airways. They last for four to six hours and come in a metered-dose inhaler or a nebulizer. Examples of short-acting bronchodilators include:
Most people use long-acting bronchodilators to manage symptoms of COPD. Providers might also prescribe long-acting bronchodilators in combination with inhaled corticosteroids to treat asthma.
Long-acting bronchodilators can last 12 to 24 hours, depending on the medication. They come in a dry powder or soft mist inhaler. You take them every day to reduce your risk of severe symptoms and the need for a rescue inhaler. They include long-acting muscarinic antagonists (LAMAs or anticholinergics) and long-acting beta-agonists (LABAs). Like short-acting bronchodilators, they work by relaxing the muscles in your airways. Examples of LAMAs include:
Examples of LABAs include:
Some inhaled treatments combine two or three medications. For instance, some medicines combine two long-acting bronchodilators and some combine one or two bronchodilators and an ICS. Combivent® combines two short-acting bronchodilators (albuterol and ipratropium). Combination medications can come in metered-dose, dry powder or soft mist inhalers. Examples include:
Long-acting beta-agonists / long-acting muscarinic antagonists
Inhaled corticosteroids / long-acting beta-agonists
Inhaled corticosteroids / long-acting beta-agonists / long-acting muscarinic antagonists
Providers treat a few diseases other than COPD and asthma with inhalers. Other medications available in dry powder inhalers include:
Albuterol is the most commonly prescribed inhaled medication. Providers commonly prescribe short-acting bronchodilators, or rescue inhalers, for COPD and asthma. Providers also sometimes prescribe short-acting bronchodilators for other respiratory illnesses like bronchitis. They give you quick relief if you’re having trouble breathing.
Each inhaler device has its own directions. Make sure you follow the directions for your specific device and ask your provider to show you how to use it. General directions include:
Benefits of using an inhaler device include:
The risks of side effects of inhalers vary by medication and the condition you’re treating. Some risks include:
Risks of inhaler devices themselves usually involve improper use.
It’s easy to misuse MDIs without even realizing it. Not all of the medication will make it to your lungs if you don’t time your inhalation correctly with the inhaler expelling the medication.
It’s important to follow the directions for using your MDI carefully. Ask your provider to demonstrate. You can also ask if a spacer is right for you. It’s a tube that attaches to the mouthpiece and makes it easier to correctly time your inhalation of the medication.
To use a DPI, you have to be able to breathe in deeply and quickly to pull the medication out. This means certain people may not be able to use DPIs. Ask your provider to demonstrate how to use the device they’ve prescribed. Talk to them if you’re concerned about your ability to use it.
Don’t use your inhaler more than prescribed by your provider. Many inhalers have a counter on them so that you can keep track of how many doses you’ve taken. Talk to your provider if you’re concerned about taking too much medication or you feel like you need more medication than prescribed to manage your symptoms.
Talk to your healthcare provider if you have any questions about using your inhaler. You should also contact them if your breathing isn’t well-managed with medications. Signs that your breathing isn’t well-managed might include waking up in the night with asthma symptoms or unexpectedly needing your rescue inhaler more than twice per week.
A note from Cleveland Clinic
Inhalers treat many conditions, but providers most commonly prescribe them for breathing conditions like asthma and COPD. Sometimes it can be hard to know if you’re using an inhaler properly and getting the most benefit from it. Have your provider demonstrate how to use your specific device and ask any questions about proper use. Speak up if you feel like a specific inhaler is too hard to use or isn’t working for you. There may be other options your provider can recommend.
Last reviewed by a Cleveland Clinic medical professional on 03/31/2023.
Learn more about our editorial process.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy