Vasa previa is a serious pregnancy complication that can pose serious risks to your fetus if you deliver vaginally. Early diagnosis, careful monitoring and a scheduled c-section delivery improve your odds of a healthy delivery and healthy baby. The success rate of diagnosed vasa previa pregnancies is 97%.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
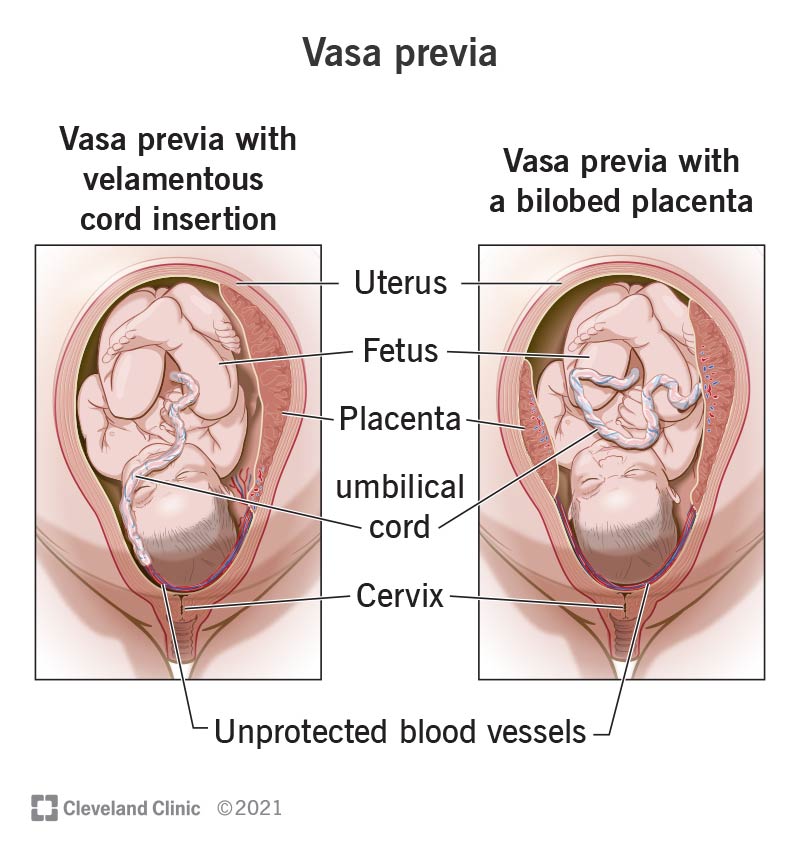
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23465-vasa-previa)
Vasa previa is a rare pregnancy complication that can lead to severe blood loss for your fetus if it’s not carefully managed. With vasa previa, unprotected blood vessels from the umbilical cord travel across the opening of your cervix (or cervical os). When your water breaks during labor, the exposed blood vessels can burst, causing severe blood loss for your fetus or even death. Diagnosing vasa previa early and delivering your baby via c-section can prevent these complications from occurring.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
There are two types of vasa previa:
Placenta previa is a condition where your placenta sits low in your uterus so that it covers your cervix. Typically, your placenta attaches to the top or side of your uterus, away from your cervix. When your placenta is close to your cervix, the blood vessels that connect your placenta to your uterus can break and bleed once labor starts. A resolved placenta previa or low-lying placenta increases the risk of vasa previa.
Advertisement
Vasa previa is serious and can result in stillbirth. However, with a prenatal diagnosis, careful treatment and a scheduled cesarean birth (c-section), the survival rate is 98.6%.
You’re more likely to have vasa previa if:
Vasa previa is rare, occurring in approximately 1 in every 2,500 deliveries. Vasa previa occurs more often in pregnancies involving IVF, about 1 in every 200 deliveries.
You may not notice symptoms with vasa previa. Instead of arriving at a diagnosis based on symptoms, your healthcare provider will likely detect vasa previa during a routine pregnancy ultrasound.
In rare instances, people with vasa previa may notice painless vaginal bleeding around the second or third trimester. The blood may be a darker red than is typical, which can be a sign that it’s fetal blood instead of your own. See your provider immediately if you notice bleeding during pregnancy, with or without pain.
Vasa previa occurs when exposed blood vessels from the umbilical cord that connects you to your fetus travel close to your cervix. Typically, the umbilical cord inserts into your placenta, which keeps the blood vessels safe from twisting or breaking. With vasa previa, not only are these blood vessels exposed, but they’re in the part of the birth canal that’s vulnerable to pressure during childbirth.
Vasa previa is usually diagnosed during ultrasound exams at around weeks 18 to 26. If there are ultrasound risk factors for vasa previa such as bilobed placenta or velamentous cord insertion, your provider can do a transvaginal ultrasound to see if there are blood vessels from the umbilical cord near your cervical os. Your provider may use the color Doppler feature on the ultrasound, which shows blood flow more clearly.
Your provider will note:
If you’re diagnosed with vasa previa, your healthcare provider will schedule a c-section delivery. Your provider will monitor your pregnancy carefully to maximize the amount of time you’re pregnant while taking care to deliver the baby before you run the risk of going into labor.
Advertisement
Your pregnancy plan may include:
Your specific pregnancy plan will depend on a number of factors that you should discuss with your provider. Follow their instructions closely to prepare for a successful delivery.
You can’t fix vasa previa, but you can put a plan in place that improves your chances of successful delivery and a healthy baby. Speak to your healthcare provider about the best time to schedule your c-section so that delivery is safe for both you and the fetus.
Advertisement
With vasa previa, you should expect a c-section instead of a vaginal delivery. And you should expect additional monitoring during your pregnancy. This additional care makes all the difference when it comes to delivering a healthy baby.
The effect that vasa previa will have on your baby depends on early diagnosis. The fetal death rate for undiagnosed vasa previa ranges from 56% to 60%. With prenatal diagnosis, proper management and cesarean delivery, the survival rate is 97%. In some instances, your baby may need additional care in a neonatal ICU unit after they’re born, but the outcomes of c-section deliveries with vasa previa are good.
You can’t reduce your risk of vasa previa, but you can reduce your risk of experiencing the most serious complications by getting regular prenatal check-ups. An early diagnosis significantly improves the outcomes of vasa previa.
Keep regular appointments with your healthcare provider and all recommended ultrasound appointments during pregnancy. If you receive a vasa previa diagnosis, you’ll require additional visits.
If you notice bleeding during your second or third trimester, schedule an appointment with your provider. If the bleeding is severe, you should go to the emergency department immediately.
Advertisement
If you have vasa previa, ask your provider how to reduce serious complications. Questions include:
Pregnancy complications are scary, but they don’t mean that you won’t have a healthy pregnancy, delivery and baby. Learning that you have vasa previa is the first step toward planning for a successful C-Section. Speak with your provider about how your diagnosis will shape plans for delivery.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Worried about your high-risk pregnancy? Want the best maternal and fetal health care? Look no further than Cleveland Clinic. We’re here for all your needs.
