A subgaleal hemorrhage is an accumulation of blood that forms between your newborn’s skull and the skin on their scalp. The condition can occur after a difficult vaginal delivery, especially if your healthcare provider needs to use a vacuum extractor. A subgaleal hemorrhage can be life-threatening, but immediate treatment leads to the best outcome.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
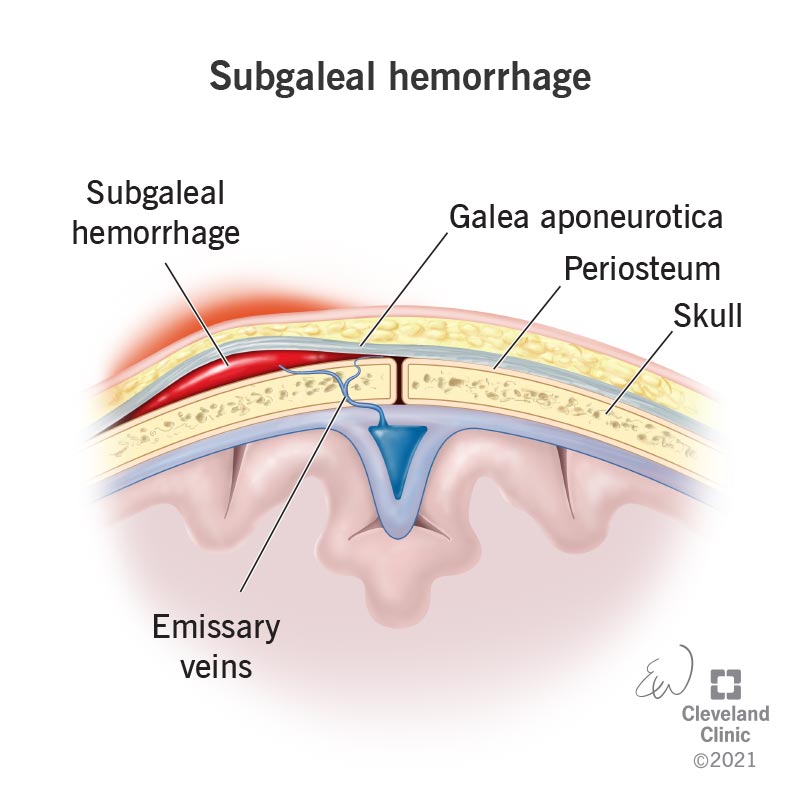
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22219-subgaleal-hemorrhage)
A subgaleal hemorrhage is an accumulation of blood within the layers of soft tissue of the head between the tough, fibrous connective tissue (galea aponeurotica) and the membrane tissue (periosteum) that covers the surface of a newborn’s skull. The condition occurs when the emissary veins that pass through a connective opening (foramen) in their scalp separate from the tissue and rupture during a difficult vaginal delivery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A subgaleal hemorrhage can be life-threatening because your baby can lose 20% to 40% of their blood volume as the hemorrhage forms in their skull. There is a cure if your baby receives treatment in a timely manner. The condition usually resolves within two to three weeks after your baby is born.
Subgaleal hemorrhages can affect any baby born via vaginal delivery. It’s more common to happen if your baby isn’t safely coming down your birth canal and your healthcare provider needs to use tools like a vacuum or forceps to help during delivery.
Subgaleal hemorrhages are rare and occur about 4 times out of every 10,000 vaginal deliveries when tools aren’t used. If tools are necessary to deliver your baby, the rate of occurrence is higher, with about 60 cases out of 10,000 deliveries that use a vacuum extractor.
When the veins that pass through a connective opening of the scalp (emissary veins) break during childbirth, blood gathers between the skin and the scalp bone where the veins ruptured (subgaleal space), causing a subgaleal hemorrhage. This only occurs during a vaginal delivery.
Sometimes, things don’t go as planned during a vaginal delivery. Subgaleal hemorrhages most often occur if your healthcare provider needs to use tools, like a vacuum extractor or forceps, to assist your baby out of your birth canal during a difficult labor process. Your healthcare provider will decide to use tools to assist if:
Advertisement
A subgaleal hemorrhage is most common after a vacuum extractor assists during delivery. The vacuum, which connects to your child’s head, can pull the skin on their scalp away from their skull. This can loosen the connective tissue in the subgaleal space of your baby’s head, allowing blood to accumulate outside of their skull. If too much blood gathers in the area of the skull with loose connective tissue, it could be life-threatening for your baby.
After your baby is born, symptoms of a subgaleal hemorrhage will appear. Symptoms of a subgaleal hemorrhage include:
Life-threatening symptoms occur in less than 25% of all cases of a subgaleal hemorrhage and include:
After your baby is born, your healthcare provider will carefully examine your baby for physical symptoms of the condition, like pale skin, swelling of their scalp and bruising. If they suspect a subgaleal hemorrhage, your healthcare provider will order an imaging test, like an ultrasound of their head, CT scan, MRI or an X-ray to examine the hemorrhage beneath their skin.
If your healthcare provider used a vacuum extractor to help deliver your baby, they’ll be closely monitored in the nursery even if they don’t present any immediate physical signs of a subgaleal hemorrhage because blood accumulation in the subgaleal area of the scalp, along with skin discoloration that indicates tissue damage can happen over time (within an hour to 72 hours after your baby is born).
If your healthcare provider diagnoses your newborn with a subgaleal hemorrhage, they’ll immediately begin treatment to restore blood volume in your baby’s body through blood and plasma transfusions in the newborn intensive care unit (NICU).
Advertisement
Your baby’s healthcare provider will monitor their blood levels to verify that their hemoglobin and hematocrit counts are where they’re supposed to be and not too low. Your healthcare provider will also regularly measure your child’s head circumference to check for swelling.
If the subgaleal hemorrhage is severe and treatment with fluid transfusions isn’t progressing, emergency surgery on the subgaleal area of their scalp will be necessary to stop internal bleeding.
After the internal bleeding caused by the subgaleal hemorrhage stops with treatment, swelling will decrease and symptoms will resolve over a couple of weeks. It’s important to follow up with your healthcare provider through routine visits during your child’s first year to monitor whether or not the condition caused any other symptoms to arise that will affect your child’s development. If treatment is successful, which occurs in an estimated 75% of subgaleal hemorrhage cases, your child will have a good prognosis and will be able to leave the nursery with you.
Although an estimated 10% to 25% of babies born with a subgaleal hemorrhage pass away during early infancy from their condition due to severe internal bleeding, the prognosis is positive for over 75% of newborns diagnosed with a subgaleal hemorrhage. Early intervention to diagnose and treat the hemorrhage leads to the best outcome for your child.
Advertisement
After treatment, your baby’s subgaleal hemorrhage symptoms will resolve within two to three weeks. Your healthcare provider will closely monitor your baby’s health after treatment to make sure there weren’t any negative reactions to the treatment, swelling goes away and your baby’s organs are properly functioning.
It’s difficult to prevent subgaleal hemorrhages from occurring because they’re the result of a difficult vaginal delivery process that often isn’t identifiable until you’re in labor.
During prenatal ultrasounds, your healthcare provider will examine your child’s position and evaluate whether or not a vaginal delivery is the safest option for both you and your baby.
Your newborn, diagnosed with a subgaleal hemorrhage, will likely stay in the NICU until your healthcare provider approves your baby is healthy enough to go home. After your baby receives treatment to alleviate symptoms of the condition, they’ll need follow-up evaluations during their first year to verify that treatment was successful and no lingering symptoms are affecting them.
It’s also important to take care of yourself during this stressful diagnosis immediately after having your baby. Make sure you surround yourself with support from your family and friends and reach out to your healthcare provider if you feel overly stressed, worried, depressed or anxious.
Advertisement
You should visit your healthcare provider if:
You should visit the emergency room if your child diagnosed with a subgaleal hemorrhage has a seizure. Seizures are a serious symptom of a subgaleal hemorrhage. A seizure occurs when your child:
Seizures normally last between 30 seconds and two minutes. Any seizure lasting more than five minutes is a medical emergency, and you should call 911 immediately, especially if your child has trouble breathing.
Subgaleal refers to the location of the condition, which is on the head, between the skin on the scalp and the skull. A hemorrhage designates that there’s active or ongoing bleeding in the subgaleal area of the head. A hematoma identifies bleeding that clots, which changes from a liquid to a partially solid form. Both a hemorrhage and a hematoma occur after an injury, damage or disruption to the blood vessels (veins) in a specific area of the body.
After a difficult delivery, you’ll likely feel anxious and stressed, as your healthcare provider gives immediate care to address your baby’s health. During this time, it’s important to surround yourself with the love and support of your family and friends to get you through this worrisome period. With quick and attentive treatment from your healthcare provider, your baby will have a more positive outcome, and you can welcome your baby home just as soon as they recover in the hospital.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic Children’s offers compassionate, expert neonatal care and surgery for preemies and newborns with complex medical conditions.
