What is Inflammatory Bowel Disease?

Inflammatory bowel disease is a group of disorders that cause chronic inflammation of the digestive tract. Crohn’s disease and ulcerative colitis are the two most common forms of IBD, affecting nearly 2 million Americans. The disease can appear at any age, although it is rare in babies and very young children. The majority of patients are diagnosed with IBD at age 10 or older.
The exact cause of Crohn’s disease and ulcerative colitis is unknown, but it has been known for a long time that a malfunctioning immune system plays a key role in causing the inflammation seen in IBD. Both forms of IBD can run in families, and the risk is increased by certain environmental factors.
Racial differences in IBD incidence exist, with the highest rates occurring among Caucasians, particularly those of Jewish descent. In the Jewish populations, rates are higher among Ashkenazi than Sephardic Jews. These differences occur across different time periods and geographic areas, suggesting a genetic basis for IBD.
Crohn’s Disease & Ulcerative Colitis: What’s the Difference?
Crohn’s disease and ulcerative colitis are similar in many ways. They both cause inflammation and sores in the tissue lining the digestive tract, leading to abdominal pain and frequent diarrhea.
However, Crohn’s disease can develop anywhere in the digestive tract from the mouth to the rectum and penetrates into the deep layers of the lining. Ulcerative colitis usually affects only the surface layer of the tissue lining the colon (the large intestine).
What is Crohn's Disease?
Crohn’s disease is a chronic illness that causes the intestine (bowel) to become inflamed and filled with sores (ulcers). Crohn’s disease most commonly affects the lower part of the small intestine (ileum), but it can occur in any part of the large intestine (colon), small intestine, stomach, esophagus or mouth. It can occur at any age, but it most commonly starts between the ages of 15 and 30. Most children with IBD have Crohn’s disease.
How Does Crohn's Disease Affect the Digestive Tract?
Crohn’s disease can disrupt the normal function of the bowel in a number of ways. The tissue may:
- Swell, thicken or form scar tissue, leading to a blockage in the bowel
- Develop ulcers that can involve the deep layers of the bowel wall
- Lose its ability to absorb nutrients from digested foods (malabsorption)
- Develop abnormal passageways (fistulas) between parts of the bowel or from the bowel to nearby organs, such as the bladder or vagina
Can IBD lead to more serious diseases such as cancer?
Some people who have IBD are not at an increased risk for developing colorectal cancer. However, ulcerative colitis and Crohn’s that affects a large portion of the colon may increase an individual’s risk.
That’s why many patients with IBD are encouraged to have a colonoscopy with extensive biopsies every one to two years, at times established after diagnosis.
Understanding your individual risk is important:
- The risk of colorectal cancer begins after symptoms of ulcerative colitis have occurred for 10 to 12 years.
- Crohn’s disease involving the colon or rectum also increases the risk of developing colorectal cancer.
- Patients with small-bowel Crohn’s disease are at increased risk for smallbowel cancer, but it is rare.
- Ongoing research at Cleveland Clinic is studying how to better identify individuals at increased risk of developing colorectal cancer.
Is IBD inherited?
There is strong evidence to suggest a genetic basis for IBD:
- Ten to 20 percent of people diagnosed with IBD have a family history of IBD, with the highest risk among first-degree relatives (mother, father, sister, brother, or children).
- A positive family history is the single greatest risk factor for IBD.
- Relatives of affected individuals have a minimum 10-fold increased risk for IBD.
- Increased rates of IBD among identical twins (compared with fraternal twins) and among siblings (compared with spouses of affected individuals) suggest that genetics are more important than environmental factors in developing this disease.
- Over the past decade, genetic research in IBD has led to many important discoveries. There are currently more than 160 genes that have been identified to be associated with IBD.
- Ongoing research, including some being done at Cleveland Clinic, is trying to define how changes in these genes lead to the development of IBD.
Symptoms
What are the Symptoms of Crohn's Disease?
Crohn’s disease causes periods of severe symptoms followed by periods of remission that can last for weeks or years. There is no way to determine when a remission will occur or when symptoms will return, although patients in therapy typically do better than those not in therapy.
The symptoms of Crohn’s disease depend on the location of the disease in the bowel and its severity. In general, symptoms may include:
- Chronic diarrhea
- Rectal bleeding
- Abdominal pain and tenderness, often on the right side of the lower abdomen
- Weight loss
- Fever
- Feeling of a mass or fullness in the lower, right abdomen
- Anemia
- Malnutrition
In children, delayed development and stunted growth is common.
Other symptoms can develop. For example, a person with a fistula (abnormal passageway) in the rectal area may experience pain and discharge around the anal area. Less common complications of Crohn’s disease include arthritis, kidney stones, gallstones, inflammation of the eyes and mouth, skin lesions, and liver disease.
What is Ulcerative Colitis?
Unlike Crohn’s disease, ulcerative colitis does not affect the esophagus, stomach or small intestine. Ulcerative colitis is a chronic inflammatory disease that affects the lining of the large intestine (colon) and rectum and leads to symptoms of bloody stools and diarrhea. In children, ulcerative colitis is less prevalent than Crohn’s disease.
How Does Ulcerative Colitis Affect the Digestive Tract?
In ulcerative colitis, the inflammation usually begins in the rectum and then spreads up the colon. How much of the colon is affected varies from person to person. If the inflammation is limited to the rectum, the disease may be called ulcerative proctitis.
Ulcerative colitis is characterized by alternating periods of flare-ups and remission in which the disease appears to have disappeared. The periods of remission can last from weeks to years.
What are the Symptoms of Ulcerative Colitis?
The main symptom of ulcerative colitis is diarrhea that may become bloody.
Symptoms may also include:
- Urgent bowel movements
- Abdominal pain
- Fever
- Anemia
Less common complications of ulcerative colitis include arthritis, kidney stones, inflammation of the eyes and mouth, skin lesions and liver disease.
The Difference Between IBD and IBS
Many people confuse IBD with irritable bowel syndrome (IBS), but they are very different. IBS is a common, uncomfortable disorder of the intestines. Factors known to trigger IBS include certain foods, medicines and emotional stress. IBS is not a life-threatening condition and does not increase the risk of developing IBD or any other more serious colon condition.
Symptoms of IBS include:
- Abdominal pains or cramps, usually in the lower half of the abdomen
- Excess gas
- Constipation, diarrhea or both
- Bowel movements that are firmer or looser than normal
IBS does not cause rectal bleeding.
Inflammatory bowel disease (IBD) refers to Crohn’s disease and ulcerative colitis, and can also be called colitis, enteritis, ileitis or proctitis. Both Crohn’s disease and ulcerative colitis cause inflammation of the bowel.
If you suspect you have IBS or IBD, it is important to see your healthcare provider for a thorough review of your medical history and a physical.
Diagnosis

How is IBD Diagnosed?
Accurate diagnosis is critical because there are conditions that can mimic IBD. Also, Crohn’s disease and ulcerative colitis are so similar that it is sometimes difficult to distinguish between the two. An accurate diagnosis enables a patient to receive the most effective treatment.
Cleveland Clinic and Cleveland Clinic Children’s gastroenterologists have extensive experience diagnosing Crohn’s disease and ulcerative colitis and are skilled in determining the best treatment for each patient based on symptoms, treatment response and test results.
They Use a Variety of Tests to Diagnose IBD:
When symptoms suggest IBD, blood and stool tests may be the first tests ordered to check for anemia, evidence of malnutrition or infection.
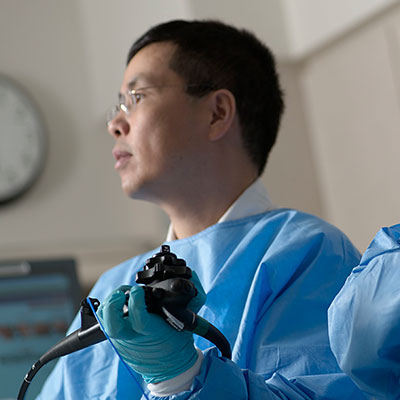
A colonoscopy is an important test for diagnosing IBD. The doctor inserts a thin, flexible, lighted tube that is long enough to view the inside of the entire colon and also the lower part of the small intestine (ileum). Tiny samples of tissue may be taken from inside the colon and examined under the microscope for signs of inflammation.
A flexible sigmoidoscopy provides a look at the last one to two feet of the colon. The doctor inserts a slender, flexible, lighted tube through the rectum and looks for inflammation, ulcers or other signs of IBD in the tissue lining this section of the colon. While sigmoidoscopy is useful for diagnosing IBD in the lowest portion of the colon, it does not reveal disease that might exist higher in the colon or in the small intestine.
An upper endoscopy provides a look at the esophagus, stomach, and first part of the small intestine (duodenum), which are areas that can be uncommonly affected in Crohn’s disease.
Small bowel X-ray tests provide a non-invasive way to get a clear picture of the entire small intestine. There are three commonly used tests: small bowel series/follow-through (using barium), computed tomography (CT) enterography and magnetic resonance enterography (MRE). These tests are particularly useful in Crohn’s disease to assess if and how much of the small intestine is inflamed and also to look for complications such as narrowing of the intestines.
A Pillcam®, a capsule containing a miniaturized camera, may be swallowed by the patient or placed in the stomach under anesthesia. As it passes through the digestive system, it relays unparalleled pictures of the intestinal walls to a small recording device. For children, this procedure, called capsule endoscopy, is performed in the Cleveland Clinic Children’s sophisticated yet family-friendly Pediatric Endoscopy Suite. This test can take up to 10 hours and the PillCam is passed with a bowel movement. You will then return the data recorder and sensors to the healthcare facility.
Treatments
How is Crohn’s Disease Treated?
Treatment options for Crohn’s disease include medications, lifestyle modification and surgery. The appropriate treatment is determined by the severity and location of the disease. Because the disease can sometimes go into remission on its own, it is not always possible to determine whether a specific treatment has been effective. When Crohn’s disease is active, the goal of treatment is to control inflammation, prevent and correct nutritional deficiencies and relieve pain, diarrhea and fever, as well as to prevent subsequent complications.
What Medications Are Used in Crohn's?
Medications are generally the first step in treating Crohn’s disease. The same medications are used in adults and children and include 5-aminosalicylic agents, steroids, antibiotics, immune suppressants and biologic agents. As with all medications, there can be side effects with these treatments and careful monitoring by experience physicians is often required.
Sometimes, Cleveland Clinic and Cleveland Clinic Children’s gastroenterologists initially use a stronger medication to bring symptoms under control quickly, then “downgrade” to a less-potent product. This is known as “topdown” therapy.
Will I Need Surgery for Crohn's Disease?
While surgery to remove active areas of IBD may one day become necessary, our goal at Cleveland Clinic and Cleveland Clinic Children’s is to prevent or delay the need for surgery as long as possible. Approximately 70 to 80 percent of patients with Crohn’s disease will require at least one abdominal surgery for treatment of their disease. Surgery to remove areas of active Crohn’s disease affected by perforations, blockages or intestinal bleeding (bowel resection) is sometimes recommended when symptoms do not respond to medications. When a significant amount of small bowel has already been removed, a technique called strictureplasty may be used to preserve intestinal length.
Although surgery cannot cure Crohn’s disease, it can relieve symptoms and can allow a patient to discontinue medications such as prednisone. Unfortunately, Crohn’s disease generally returns in previously healthy bowel after surgery. Sometimes surgery in Crohn’s disease requires either a temporary or permanent external pouch to collect stool (ileostomy or colostomy). Following surgery for Crohn’s disease, the majority of pediatric patients are started on medications (called postoperative prophylaxis) to delay or prevent disease recurrence.
If you have been told you or your child need surgery to treat Crohn’s disease, you may want to seek a second opinion to ensure that surgery is appropriate. Make sure your diagnosis is confirmed by experts at an institution experienced in identifying and treating digestive disorders.
How is Ulcerative Colitis Treated?
Treatment for ulcerative colitis can include drug therapy, dietary modifications and/or surgery. Though medications cannot cure ulcerative colitis, they can help most people lead normal lives.
It is important to seek treatment as soon as symptoms appear. In the case of severe diarrhea and bleeding, hospitalization may be necessary. In addition, for those with longstanding ulcerative colitis that involves more than just the lowest portion of the colon (rectum and sigmoid), colonoscopy with multiple biopsies should be performed every one to two years to be sure that no precancerous changes (dysplasia) are developing in the colon.
What Medications Are Used in Ulcerative Colitis?
Several medications are used to reduce inflammation of the bowel tissue, allowing it to heal and relieving symptoms. The most common medications include 5-aminosalicylic agents, steroids, immune suppressants and biologic agents.
Will I Need Surgery for Ulcerative Colitis?
An estimated 25 to 40 percent of patients with ulcerative colitis eventually require surgery, because medications are not effective, or because of the development of precancerous changes or cancer of the colon.
Typically, either the entire colon and rectum are removed (proctocolectomy), effectively curing ulcerative colitis. Once the colon has been removed, an external pouch or internal pelvic pouch is needed to collect stool.
Medical management is the treatment of choice in children. However, surgery may be used when medications are not effective or to remove (resect) precancerous changes or cancer developing in the colon. Removing the entire colon and rectum (proctocolectomy) effectively cures ulcerative colitis. An exteriorized stoma, known as an ileostomy, or internal pelvic pouch is then used to collect stool.
If you have been told you need surgery to treat ulcerative colitis, you may want to seek a second opinion to ensure the treatment is appropriate. Make sure your diagnosis is confirmed by experts at an institution experienced in identifying and treating digestive disorders.
Common medications for Crohn’s disease and ulcerative colitis
- 5-aminosalicylic acid (5-ASA). Sulfasalazine and mesalamine are drugs used to treat ulcerative colitis and less commonly Crohn’s disease.
- Corticosteroids. When 5-ASA is not effective or disease is more severe, a stronger anti-inflammatory medication such as a corticosteroid may be used to bring bowel inflammation under control (remission). Corticosteroids are very helpful in controlling symptoms, but cannot be used over the long term due to side effects and the potential for complications. After disease is brought under control with corticosteroids, remission is usually maintained with other medications that can be used long term.
- Immunosuppressants. If corticosteroids or 5-ASA are not effective, an immunosuppressant such as 6-mercaptopurine (6-MP), azathioprine or methotrexate may be prescribed. These medications suppress the immune system just enough to fight off chronic inflammation and allow the bowel to heal. They can be used for long-term maintenance, because they have fewer side effects than steroids.
- Biologic agents. These are the newest class of medications developed to treat IBD. There are currently four biologics agents that are FDAapproved for the treatment of IBD. Infliximab (Remicade®) , adalimumab (Humira®) and vedoligumab (Entyvio®) are approved for the treatment of both ulcerative colitis and Crohn’s disease while adalimumab (Humira®), certolizumab pegol (Cimzia®) and natalizumab (Tysabri®) are only approved for the treatment of Crohn’s disease. Some of these treatments are not currently available for pediatric patients.
Pelvic Pouch
What is a Pelvic Pouch and What are the Different Types?
When the colon and rectum are removed, accommodations must be made for solid waste to exit the body. Cleveland Clinic colorectal surgeons and Cleveland Clinic Children’s pediatric surgeons offer several options.
When the entire colon is removed, an opening (stoma) may be created in the abdominal wall (permanent ileostomy). The tip of the lower small intestine is brought through the stoma. Stool passes through this opening and collects in an external bag, which is attached to the stoma and worn at all times.
The ileal pouch anal anastomosis (IPAA) procedure is an option that does not require a permanent stoma. In this procedure, the colon and rectum are removed, and the small intestine is reshaped to form an internal pouch (reservoir) that serves as a rectum and is connected to the anus. The reservoir is called a J-pouch. This procedure is frequently done in two operations and requires a temporary ileostomy after the first operation.
Other ileal pouch types include the S-pouch and the K-pouch (also known as a Kock pouch or continent ileostomy). Most patients at Cleveland Clinic receive a J-pouch, which is the current gold standard surgical procedure for IBD.
Our physicians have among the world’s largest experience with pouch procedures.
About Pouchitis
Pouchitis, an inflammation caused by a bacterial infection, is the most common long-term complication of the J-pouch procedure in patients with ulcerative colitis. Symptoms are not always specific, but may include more frequent and urgent bowel movements and abdominal cramping.
Pouchitis often responds to a course of antibiotics but can sometimes be difficult to treat. Cleveland Clinic established the nation’s first and largest Pouchitis Clinic to diagnose and treat pouch-associated disorders and specializes in customizing treatments for antibiotic-resistant cases with anti-inflammatory agents and immunomodulators.
Living with IBD

Nutrition & IBD
For adults with IBD who experience nutritional deficiencies, supplements are often prescribed. Cleveland Clinic’s Center for Human Nutrition provides a single resource for the comprehensive evaluation, education and treatment of patients with nutritional needs related to IBD.
Children with IBD can have problems with appropriate growth and development because their inflamed bowel may not absorb nutrients well. In addition, they may not like to eat since they hurt after a meal. Pediatric dietitians at Cleveland Clinic Children’s help children with IBD choose the most nutritious and tasty foods and supplements to get them back on track. A pediatric registered dietitian is a licensed health professional who specializes in the nutritional care of children and understands their specific needs.
Cleveland Clinic Children’s has a team of registered dietitians, board-certified in pediatrics, who collaborate with physician teams to provide expert, evidence-based nutritional care for infants, children and adolescents. The Pediatric Nutrition Support Team provides individual counseling to assess each child’s nutritional needs, develop the most appropriate plan of nutritional support and monitor nutritional status to ensure an optimal outcome.
The Role of Lifestyle in IBD
It is very important for patients with Crohn’s disease or ulcerative colitis to maintain a healthy lifestyle, even when the disease is in remission. Exercising regularly, eating a healthy, well-balanced diet and managing stress can help management of both diseases.
Abstaining from smoking is particularly important. Studies have shown that smokers with Crohn’s disease tend to have a more severe course than nonsmokers with Crohn’s.
Having a child with IBD affects the entire family. That’s why Cleveland Clinic Children’s pediatric IBD specialists take a family-centered approach to care that aims to help families achieve a healthy lifestyle that benefits everyone.
Because teenagers like to feel independent, we help them “buy in” to their therapy and a healthy lifestyle through understanding their disease and the advantages of making healthy choices.
Helping Patients Cope with IBD
It is our goal to guide patients and families in making the best treatment decisions. Helping them cope with their disease is part of the process. Because living with a chronic disease is not always easy, we provide IBD patients and their families with resources for coping with the emotional, physical and cognitive aspects of their disease. We offer educational materials, support groups and links to useful outside resources that can assist with adjusting to life with IBD. At every clinic visit, we provide detailed explanations and welcome questions.
Pediatric IBD

Why is Specialized Pediatric IBD Care Important?
At Cleveland Clinic Children’s, we understand children and their families require the best medical care in the world, delivered with a large dose of compassion. That’s why we put kids with IBD and their families first.
Many things set us apart from other pediatric facilities. We have one of the largest pediatric GI centers in the country, treating more than 15,000 patient visits annually. Our team includes 15 pediatric gastroenterologists as well as pediatric IBD nurse practitioners and care coordinators, GI dieticians, and a GI psychologist, who focus on helping to relieve symptoms, manage chronic abdominal pain and understand the benefits of complying with treatment. Our physicians have been nationally recognized and serve as leaders in the field of IBD.
Our pediatric gastroenterologists treat more children and adolescents with IBD every year than many other programs. They understand the needs of young patients and their families. Families are considered key members of their child’s treatment team and are involved in all treatment decisions. You also can take comfort in knowing that your child will not need to leave Cleveland Clinic for his or her continued IBD care, as we work with experts from our Digestive Disease & Surgery Institute to provide a seamless transition of care from childhood to adolescence and into adulthood.
Although there is no one solution for treating IBD, there are many options. We help patients find the most effective treatments that produce remission and prevent flare-ups, allowing them to enjoy the best quality of life possible. Sometimes this means being able to offer patients a treatment option after they and their physicians elsewhere had given up hope. Moreover, our pediatric gastroenterologists are an integral part of the world-renowned Cleveland Clinic. That means that our pediatric specialists are able to communicate quickly and easily with their adult counterparts at our Digestive Disease & Surgery Institute, and help in transitioning care for young adults. This gives young patients and their families access to the expertise of internationally known pediatric and adult specialists, and to the leading-edge technology that only a large institution can provide.
Center for Pediatric Inflammatory Bowel Disease
Our pediatric gastroenterologists offer diagnosis, treatment and follow-up for children with Crohn’s disease and ulcerative colitis. We were one of the first pediatric inflammatory bowel disease centers in the country to offer infusions of biologic agents such as infliximab (Remicade®). We administer biologics on an outpatient bases to more than 150 patients annually and monitor patients’ progress in office visits. Visit our website.
Our Center for Inflammatory Bowel Disease is a significant contributor to the National Pediatric IBD Registry, which involves 25 of the top children’s hospitals in the United States and Canada. The registry’s goal is to study the natural history of early-onset ulcerative colitis and Crohn’s disease to improve children’s treatment outcomes.
Our Center also serves as an ImproveCareNow site. ImproveCareNow is a collaborative community where patients, parents, clinicians, and researchers work together to improve the health and care of children and youth with Crohn's disease and ulcerative colitis (also known as Inflammatory Bowel Disease or IBD).
Cleveland Clinic Children’s Pediatric Gastroenterology, Hepatology, and Nutrition Department regularly works with Cleveland Clinic Children’s Healthcare Partners to promote and enhance safer patient care and improve the patient experience.
Endoscopy Suite and Infusion Center
Our Pediatric Endoscopy Suite has the latest generation of endoscopy equipment, offering enhanced safety and a higher diagnostic yield to patients aged 2 up to early 20s. Outpatient endoscopy is conducted for the diagnosis of conditions such as IBD and gastroesophageal reflux disease (GERD). Endoscopy services in our pediatric operating room are offered for children from infancy through adolescence.
Multidisciplinary Approach to Pediatric Care
Our gastroenterological patients have access to multiple specialties, including pediatric surgery, pediatric radiology and pediatric anesthesia, as well as the full resources of Cleveland Clinic. Our team actively collaborates with other pediatric subspecialty providers in the treatment of pediatric patients.
This means that you can take comfort in the fact that our dedicated teams specialize in caring solely for children — from the tiniest premature infants to teenagers. Our pediatric anesthesiologists manage nearly 8,000 cases each year and our pediatric radiologists are committed to minimizing radiation exposure for children.
Combined Pediatric/adult IBD and Pouchitis Clinics
Patients can now benefit from new monthly clinics in which colorectal surgeons from the Digestive Disease & Surgery Institute combine forces with gastroenterologists and surgeons from Cleveland Clinic Children’s. These new clinics for IBD and pouchitis provide the highly specialized, multidisciplinary care needed to improve quality of life for patients with IBD and pouchitis. They also help set the stage for a smooth transition from pediatric to adult care.
Innovations and Experience

Cleveland Clinic programs have an international reputation for excellence in IBD, including:
- More operations for Crohn’s disease than any other institution, including the bowel-conserving strictureplasty procedure
- The world’s highest volume of J-pouch procedures
- The nation’s largest referral center for repairing pelvic pouches
- Management of 12 disease- and treatment-specific databases
- Establishment of the world’s first and largest Pouchitis Clinic to diagnose and treat pouchassociated disorders, such as pouchitis and Crohn’s disease of the pouch
- Establishment of an IBD DNA bank to help understand the disease’s genetic basis
- Collaborations with Cleveland Clinic Lerner Research Institute lab scientists to better understand how IBD develops and progresses
- Performed the world’s first total proctocolectomy and ileoanal pouch procedure with a single incision
- More than 2,900 infusions performed each year This is vitally important in a chronic disease such as IBD, where patients require care for life. Most of our IBD patients stay with their Cleveland Clinic Children’s gastroenterologist through their college years, but they are welcome to transition to an adult gastroenterologist at any time. When the time is right, we help make the transition as smooth as possible.
Patient Services
MyChart
Cleveland Clinic MyChart® is a secure, online personal healthcare management tool that connects patients to their medical record. Patients can register for MyChart through their physician’s office or by going online.
Parents and caregivers of children under age 18 can view test results, renew prescriptions, review past appointments and request new ones using Cleveland Clinic MyChart.Caregiver. This secure online healthcare management tool connects parents and legal guardians to portions of a child’s medical record at any time, day or night. Parents visit MyChart to register.
Medical Concierge
For complimentary assistance for out-of-state patients and families, please call 800.223.2273, ext. 55580, or email medicalconcierge@ccf.org.
Additional Resources for IBD Patients:
Crohn’s and Colitis Foundation of America: a nonprofit, volunteer-driven organization dedicated to finding the cure for Crohn’s disease and ulcerative colitis.
National Institute of Diabetes and Digestive and Kidney Diseases: part of the National Institutes of Health that conducts and supports basic and clinical research.
North American Society for Pediatric Gastroenterology, Hepatology and Nutrition GI Kids: a resource for pediatric digestive disorders.
Appointments
Make an Appointment
Adult patients: Please call 216.444.7000 or contact Cleveland Clinic Digestive Disease & Surgery Institute.
Pediatric patients: Please call 216.444.5437 or visit Cleveland Clinic Children's Gastroenterology Department.
To make an appointment at our Akron location, please call 330.665.8270.
Virtual Visits
Cleveland Clinic and Cleveland Clinic Children's offer virtual visit appointments, allowing you to meet with a specialist from the comfort of your home, using a mobile device or computer.
Virtual Second Opinion
If you cannot travel to Cleveland Clinic, help is available. You can connect with Cleveland Clinic specialists from any location in the world via a phone, tablet, or computer, eliminating the burden of travel time and other obstacles. If you’re facing a significant medical condition or treatment such as surgery, this program provides virtual access to a Cleveland Clinic physician who will review the diagnosis and treatment plan. Following a comprehensive evaluation of medical records and labs, you’ll receive an educational second opinion from an expert in their medical condition covering diagnosis, treatment options or alternatives as well as recommendations regarding future therapeutic considerations. You’ll also have the unique opportunity to speak with the physician expert directly to address questions or concerns.
Why Choose Us?
Experts at the Cleveland Clinic’s Digestive Disease & Surgery Institute and Cleveland Clinic Children’s tailor treatment plans to each patient’s needs, taking into account the patient’s age, type of inflammatory bowel disease (IBD) and how severe the disease is at the time of evaluation. This guide provides an overview of treatment options offered at Cleveland Clinic for IBD — which includes both Crohn’s disease and ulcerative colitis — in patients from infancy through adulthood.
Choosing IBD Care
From the time IBD is diagnosed, patients require lifelong care. That’s why treatment at Cleveland Clinic is advantageous. It’s one of the few medical centers in the country uniquely able to provide seamless care for IBD patients of all ages throughout their life.
At Cleveland Clinic and Cleveland Clinic Children’s, we are dedicated to providing expert diagnosis and the most advanced medical and surgical treatment options available for IBD today. With an IBD Center that has earned an international reputation for excellence, Cleveland Clinic provides adult and pediatric gastroenterologists, colorectal surgeons, general surgeons, liver and transplant surgeons and nutritionists under one roof. This enables patients to be seen by many specialists in one day, when needed.
With surgical innovations, advanced treatment options and some of the best long-term outcomes in the world, Cleveland Clinic receives increasing worldwide referrals, particularly for complex IBD cases, access to clinical trials or for surgical expertise that consistently reports excellent outcomes.
Although there is no one solution for treating IBD, there are many options. We help patients find the most effective treatments that produce remission and prevent flareups, allowing them to enjoy best quality of life possible. Sometimes this means being able to offer patients a treatment option after they and their physicians elsewhere had given up hope.
Resources
Stay Connected
- Explore our services, locations and more
- Find a wealth of family health & wellness tips
- For more information on IBD, listen to these Butts & Guts podcast episodes:
- Inflammatory Bowel Disease (IBD) Patient-Centered Medical Home Delivers Integrated Multidisciplinary Care to Patients
- Managing Inflammatory Bowel Disease During the Coronavirus Pandemic
- Understanding Ulcerative Colitis with Dr. Jeremy Lipman
- Patient Perspectives: Managing Ulcerative Colitis
- Subscribe to Health Essentials e-News for expert insights on nutrition, health and wellness