About Heart Valve Disease
Heart valve disease refers to any of several conditions that prevent one or more of the valves in the heart from functioning adequately to assure proper circulation. Left untreated, heart valve disease can reduce quality of life and become life-threatening. In many cases, heart valves can be surgically repaired or replaced, restoring normal function and allowing a return to normal activities.
Cleveland Clinic’s Sydell and Arnold Miller Family Heart, Vascular & Thoracic Institute is one of the largest centers in the country for the diagnosis and treatment of heart valve disease. The decision to prescribe medical treatment or proceed with surgical repair or replacement is based on the type of heart valve disease you have, the severity of damage, your age and your medical history.
Heart valve disease means one of the heart valves isn’t working properly because of valvular stenosis (narrowing of the valves) or valvular insufficiency (“leaky” valve). These conditions cause the heart to work harder to pump the right amount of blood through the body. It is possible to have valvular stenosis and valvular insufficiency in one or more valves.
If you have valve disease, you will need treatment. Many patients with valve disease can have surgery to repair or replace the diseased valve(s). The treatment causes the valve to work normally again and then you can return to your normal activities. Without treatment, valve disease can reduce your quality of life and become life-threatening.
The heart valves
The heart has four valves — one for each chamber of the heart. The valves keep blood moving through the heart in the right direction.
The mitral and tricuspid valves are located between the atria (upper chambers of the heart).
The aortic and pulmonic valves are located between the ventricles (lower chambers of the heart) and the major blood vessels leaving the heart.
Leaflets
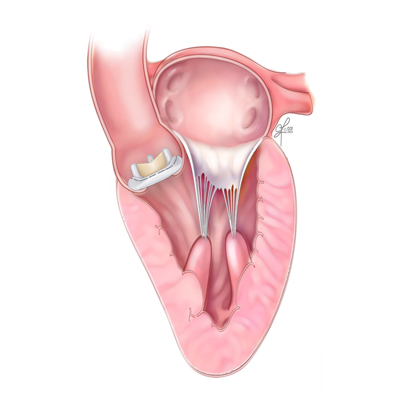
The valves are made of strong, thin flaps of tissue, called leaflets. The leaflets open to let blood move forward through the heart during half of the heartbeat. They close to keep blood from flowing backward during the other half of the heartbeat.
The leaflets in the mitral and tricuspid valves are supported by:
- Annulus: tough, fibrous ring attached to the leaflets that helps support and maintain the proper shape of the valve.
- Chordae tendineae: tough, fibrous strings
- Papillary muscles: part of the inside walls of the ventricles
The chordae tendineae and papillary muscles keep the leaflets stable to prevent blood from flowing backward.
Normal aortic valve – three leaflets.
Bicuspid aortic valve – two leaflets. The valve may not open fully (stenosis) or may not close tightly (regurgitation).
How the Valves Work
Blood flow through the heart
The four valves open and close to let blood flow through the heart. The illustration below shows how the blood flows through the heart and describes how each valve works to keep blood moving.
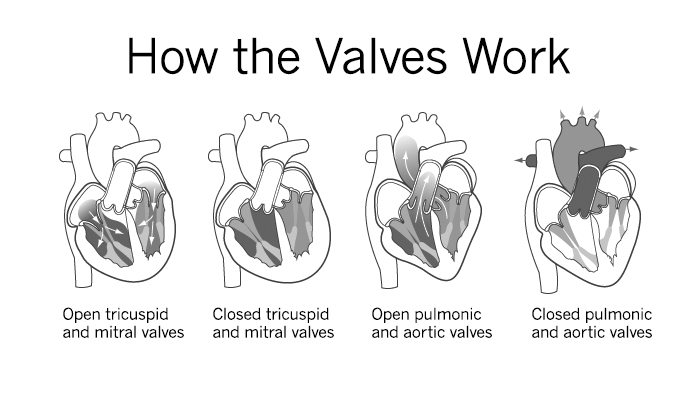
Open tricuspid and mitral valves
Blood flows from the right atrium into the right ventricle through the open tricuspid valve, and from the left atrium into the left ventricle through the open mitral valve.
Closed tricuspid and mitral valves
When the right ventricle is full, the tricuspid valve closes and keeps blood from flowing backward into the right atrium when the ventricle contracts (squeezes).
When the left ventricle is full, the mitral valve closes and keeps blood from flowing backward into the left atrium when the ventricle contracts.
Open pulmonic and aortic valves
As the right ventricle begins to contract, the pulmonic valve is forced open. Blood is pumped out of the right ventricle through the pulmonic valve into the pulmonary artery to the lungs.
As the left ventricle begins to contract, the aortic valve is forced open. Blood is pumped out of the left ventricle through the aortic valve into the aorta. The aorta divides into many arteries and provides blood to the body.
Closed pulmonic and aortic valves
When the right ventricle finishes contracting and starts to relax, the pulmonic valve snaps shut. This keeps blood from flowing back into the right ventricle.
When the left ventricle finishes contracting and begins to relax, the aortic valve snaps shut. This keeps blood from flowing back into the left ventricle.
This pattern is repeated over and over, causing blood to flow continuously to the heart, lungs and body. The four normally working heart valves make sure that blood always flows freely in one direction and that there is no backward leakage.
Causes
What causes valve disease?
A person can be born with valve disease (congenital) or develop a problem later in life (acquired). Common causes of acquired valve disease include infection (such as rheumatic fever and infective endocarditis) and changes to the valve that develop over time.
Congenital valve disease
Congenital valve disease develops before birth. Common problems that cause this type of valve disease are abnormal valve size, leaflets that are not properly formed, and abnormal leaflet attachment. Congenital valve diseases include bicuspid aortic valve disease and mitral valve prolapse.
Bicuspid aortic valve disease is a type of congenital valve disease that affects the aortic valve. The valve has two leaflets instead of three. At least 25 percent of patients with this disease have a larger than normal aorta above the valve. The valve may not open fully (stenosis) or may not close tightly (regurgitation). The condition affects about 2 percent of the population.
Mitral valve prolapse (MVP) is a type of valve disease caused by weaker than normal connective tissue in the mitral valve. The condition causes the leaflets of the mitral valve to flop back into the left atrium when the heart contracts. The tissues of the valve also become abnormal and stretchy. This causes the valve to leak.
Mitral valve prolapse affects about 1 to 2 percent of the population. Men and women have the same risk of MVP. The condition usually isn’t a reason for concern. Only a small percentage of patients with MVP eventually need surgery. If the prolapse becomes severe or is associated with torn chordae or flail leaflets (floppy and lacking support), it could lead to a bad leak, and surgery may be needed.
All patients with MVP should ask their doctor if they need to take precautions to prevent endocarditis.
Acquired valve diseases
Acquired valve diseases include problems that develop with valves that were once normal. Acquired disease can be the result of infection, such as infective endocarditis and rheumatic fever. It can also be caused by changes in the valve structure, such as stretching or tearing of the chordae tendineae or papillary muscles, fibrocalcific degeneration or dilatation of the valve annulus. Sometimes the cause of acquired valve disease is unknown.
Infection
Both infective endocarditis and rheumatic fever can lead to valve disease. Infective endocarditis is a major infection and can be life-threatening. Germs attack the heart valve and may cause the valve to leak. Rheumatic fever may cause the valve leaflets to become inflamed. The leaflets may stick together and become scarred, rigid, thickened and shortened. One or more of the valves (most commonly the mitral valve) may become stenotic (narrowed) or leaky.
How does infective endocarditis develop?
Infective endocarditis (also called bacterial endocarditis) is an infection of the heart valves or the heart’s inner lining (endocardium). It occurs when germs (especially bacteria, but occasionally fungi and other microbes) enter the blood stream and attack the lining of the heart or the heart valves.
Bacterial endocarditis causes growths or holes on the valves or scarring of the valve tissue. This often causes a leaky heart valve. Bacterial endocarditis can be deadly if it is not treated.
How does rheumatic fever develop?
Rheumatic fever is usually the result of an untreated streptococcal infection, such as strep throat. The use of penicillin to treat strep throat can prevent this disease. It occurs most often in children between the ages of five and 15, and it can take years for symptoms of valve disease to develop.
The valve itself is not infected when you have rheumatic fever. Instead, the body produces antibodies to fight the infection, and they react with the heart valves, causing inflammation and eventual scarring.
Structural valve disease
Structural valve diseases include stretching or tearing of the chordae tendineae or papillary muscles, fibro-calcific degeneration or dilatation of the valve annulus.
Symptoms
What are the symptoms of heart valve disease?
When the heart valves begin to fail, the heart beats harder to make up for the reduced blood flow. As the heart beats harder, symptoms of valve disease may occur, including:
- Increased shortness of breath
- Heart palpitations (feeling of skipped heartbeats)
- Chest pain or discomfort
- Swelling of the ankles, feet or abdomen (edema)
- Rapid weight gain (3 pounds in one day is possible)
- Increasing fatigue
- Weakness or dizziness
Symptoms can occur quickly if the onset of valve disease is severe and sudden. Some people slowly develop symptoms, possibly without noticing them.
Call your doctor if you have any of these symptoms so you can be checked for valve disease. If you have already been diagnosed with valve disease, keep your regular follow-up appointments and call your doctor if you have any new symptoms or if they get worse or happen more often. Don’t wait for your next appointment to tell your doctor about changes in your symptoms.
Valve disease and other heart conditions
Patients with valve disease often also have heart failure or atrial fibrillation.
Heart failure means your heart is working less efficiently and cannot pump a normal amount of blood. Symptoms of heart failure and valve disease are similar. If you have heart failure, it is important to follow your treatment plan, which may include:
- Not smoking
- Weighing yourself daily and reporting sudden changes
- Medications to control body fluid and help your heart pump better
- Limiting the amount of salt/sodium in your diet
- Maintaining a healthy weight
- Regular exercise
- Regular doctor visits
Atrial fibrillation is an abnormal heart rhythm that starts in the atria (upper chambers of the heart). It can cause a rapid and disorganized heartbeat.
Many treatment options are available for patients with atrial fibrillation. These include medications, lifestyle changes, ablation procedures and surgery. The best treatment for you is based on your heart rhythm and symptoms.
Diagnosis
How is valve disease diagnosed?
Your doctor will perform an exam and diagnostic tests. Those results, along with your symptoms, will help the doctor make a diagnosis.
The physical exam may show that you have fluid in your lungs, an enlarged heart or a heart murmur. A heart murmur is the sound made by blood moving through a narrowed or leaky valve.
Diagnostic tests help determine the location, type and extent of your valve disease. They help your doctor see how severe the leak or stenosis is and how it is affecting your heart’s function and ability to pump blood. These tests may include:
Echocardiogram (echo): A graphic outline of the heart’s movement. High-frequency sound waves are sent through a transducer that is placed on your chest. This produces pictures of the heart’s valves, chambers and pumping action. An echo can show a narrowed or insufficient valve.
Specialized echos include:
- Exercise stress echocardiogram: An echo performed while you exercise to see how your heart works when you are active.
- Transesophageal echo (TEE): This type of echo uses a special tube (called an endoscope) that is passed into the mouth and down the esophagus (“food pipe”). This lets your doctor get a closer view of your heart.
- Myocardial strain imaging: Used to check for changes in heart function.
- 3D echo: This echo can display parts of your heart in three dimensions so your doctor can more completely measure the size and check the function of your heart and valves.
Electrocardiogram (ECG or EKG): A picture on graph paper of the electrical impulses traveling through the heart muscle. Electrodes (small, sticky patches) are placed on the body, and they send the information that creates the picture. An EKG can detect abnormal electrical activity in the heart.
Cardiac catheterization (cardiac cath or coronary angiogram): An invasive imaging procedure used to check heart function. During a cardiac catheterization, a long, narrow tube (catheter) is guided through a blood vessel in the arm or leg to the heart with the help of a special X-ray machine. Contrast dye is injected through the catheter, and X-ray movies are created as the dye moves through the heart. A cardiac cath can detect a narrowed or insufficient valve.
Magnetic resonance imaging (MRI): A large magnet and radio waves are used to produce a picture of the heart’s valves and chambers. It can create moving images of the heart as it is pumping and can detect abnormal blood flow through the heart.
Other tests to get more detailed information about your condition and heart function.
If you are seen at Cleveland Clinic, you may need to have tests done elsewhere repeated. Our physicians have the ability to perform more sophisticated and advanced testing than is available at some hospitals.
You will receive detailed information about testing you need, including how to prepare and what to expect. If you have questions at any time about testing, please ask your doctor or other member of your healthcare team.
By repeating these tests over time, your doctor can keep track of how your valve disease progresses and help you make treatment decisions.
Treatments
What treatments are available?
Treatments for valve disease include:
- Protecting your valve from further damage by reducing the risk of infective endocarditis
- Medications to ease symptoms and reduce the risk of further valve damage
- Valve repair or replacement surgery, if needed
- Catheter-based procedures, if needed
- Following up with your doctor for regular visits. Valve disease can get worse without any symptoms, so it is important to see your doctor as scheduled to check your condition.
The best treatment options for you depends on several factors, including the type of valve disease you have, the severity of the damage, your age and medical history. Your healthcare team will talk to you about each option.
Treatment with medication
You may need to take medication to help your heart pump better. This helps make up for the loss of pumping power because of the diseased valve.
Is surgery better for me than medication alone?
Medications often help during the first stages of valve disease, but they don’t work as well as the disease gets worse. You do not need to delay surgery until your symptoms are unbearable. It is sometimes best to have surgery before you start to have symptoms. The decision to have surgery is a major one that is based on your individual needs. It involves input from you, your cardiologist and your heart surgeon.
What if I choose not to have surgery?
Valve disease is a mechanical problem that does not go away. As this happens, you will have more symptoms that will get worse. Your overall health will also get worse. Many times, symptoms come on slowly, but they can happen quickly. If you decide against surgery, you should stay in close contact with your doctor. Surgery usually remains a treatment option, even for patients with advanced valve disease, and it may be the only effective treatment.
Valve surgery
There are two types of valve surgery — valve repair surgery and valve replacement surgery. If you need valve surgery, your doctor will determine the best type of surgery for you based on your condition and other factors.
Valve surgery may be combined with other heart surgeries, such as other valve procedures, bypass surgery, aortic aneurysm surgery or surgery to treat atrial fibrillation.
Types of Valve Surgery
Valve Repair Surgery
During valve repair surgery, the surgeon fixes the damaged or faulty valve. This surgery is often done without using artificial parts. The mitral valve is the most commonly repaired valve, but repair surgery can also be used to treat problems with the aortic and tricuspid valves.
The potential advantages of valve repair versus valve replacement are:
- Lower risk of infection
- Less need for lifelong anticoagulant (blood thinning) medication
- Preserved heart muscle strength
Types of valve repair techniques include commissurotomy, decalcification, resection of a portion of the valve leaflet, creation of new chords, annulus support, patched leaflets and bicuspid aortic valve repair.
Types of Valve Repair Surgery
1 of 5Valve Replacement Surgery
Valve replacement surgery is performed when valve repair surgery is not a treatment option. Valve replacement surgery is most often used to treat patients with aortic valve disease, especially those with aortic stenosis. Valve replacement surgery involves removing the faulty valve (native valve) and replacing it with a mechanical or biological valve. The new valve is sewn to the rim (annulus) around your native valve. All valve replacements are “biocompatible,” which means the new valve will not be rejected by your immune system.
Types of valve replacement surgery
Biological valves
Biological valves (also called tissue or bioprosthetic valves) are made from cow tissue (bovine), pig tissue (porcine) or human tissue (allograft or homograft). Biological valves may have some artificial parts to give the valve support and to make it easier to put them into place.
Most patients who receive a biological valve replacement do not need lifelong anticoagulant therapy after surgery.
In the past, biological valves were thought to be less durable than mechanical valves. But, recent studies show these valves often last at least 10 to 15 years without a decline in function.
A homograft valve is a human heart valve that comes from a donor after death. It is frozen and use to replace the native valve. A homograft can be used to replace a diseased aortic valve, especially if there is an infection. It can also be used to replace the pulmonic valve during the Ross procedure.
The Ross procedure is most often used to treat children and young adults with aortic valve disease. The surgery involves removing the pulmonic valve and using it to replace the diseased aortic valve. The pulmonic valve is then replaced with a homograft valve.
Mechanical valves
Mechanical valves are made of metal or carbon. They are well-tolerated by the body, very durable and are made to last a lifetime.
The bileaflet valve is the most common type of mechanical valve. It is made up of two carbon leaflets mounted in a ring that is covered with polyester knit fabric.
If you have your valve replaced with a mechanical valve, you will need to take a blood-thinning medication (anticoagulant), such as warfarin (Coumadin®), for the rest of your life. Anticoagulant medication causes blood to clot slower than normal. It helps prevent blood clots from forming on the replaced valve. This helps reduce your risk of a heart attack or stroke.
If you take Coumadin®, you need to have regular blood tests (Prothrombin time/ PT). This test calculates your international normalized ratio (INR), which is a measurement of how quickly your blood clots. Measuring your INR helps your doctor see how well you are responding to the medication and if you need a change in your dose.
Some patients who have a mechanical valve replacement hear the valve make a clicking noise. This is the sound of the valve leaflets opening and closing.
Valve surgery techniques
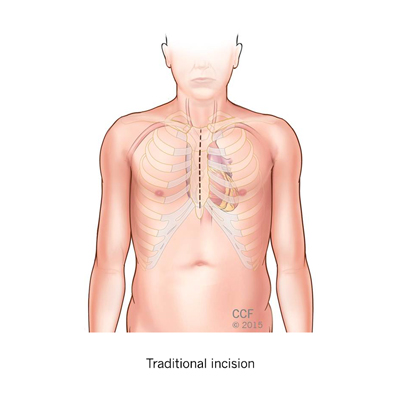
Traditional surgical approach (median sternotomy)
Traditional heart surgery involves a 6-to-8-inch incision through the breastbone to open the chest wall and reach the heart and arteries. This type of incision is needed for many types of heart surgery. The surgeon will use the smallest incision possible to perform the surgery.
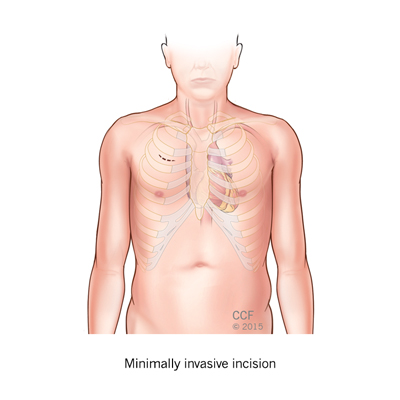
Minimally invasive valve surgery
Minimally invasive heart valve surgery is performed using smaller incisions than those in traditional heart valve surgery. Techniques include endoscopic or keyhole approaches (also called port access, thoracoscopic or video-assisted surgery) and robotically assisted surgery. Your surgeon will be able to tell you if you are a candidate for this type of surgery.
The benefits of minimally invasive surgery include a smaller incision (3-4 inches or smaller than traditional incisions) and smaller scars. Other possible benefits include a reduced risk of infection, less bleeding and trauma, a shorter hospital stay (3-5 days) and shorter recovery.
Valve surgery (replacement and repair) is the most common type of minimally invasive procedure. There are many types of incisions used by surgeons who perform valve surgery. Plese talk to your surgeon about the types of incision(s) and scar(s) you might expect to have.
Transcatheter approaches
Transcatheter aortic valve replacement (TAVR)
Transcatheter aortic valve replacement (TAVR) is a treatment option for some patients with severe aortic stenosis who are either too high-risk to have traditional open-heart surgery or cannot have an operation because they have too many other health problems. The TAVR procedure is used to replace the aortic valve.
The doctor uses a catheter to replace the diseased valve with a biological valve. The catheter is inserted into an artery through your groin or an incision in your chest. Not all patients are eligible for TAVR. If you are interested in this treatment, please talk to your doctor.
Transcatheter MitraClip® mitral valve repair
The MitraClip is a treatment option for some patients with severe symptomatic mitral regurgitation (leaky valve) who are too sick to have traditional open-heart surgery to repair the valve. The doctor uses a catheter to place the MitraClip on the valve leaflets. This helps them close more tightly. The catheter is inserted into an artery through your groin or an incision in your chest. Not all patients are eligible for the MitraClip procedure. If you are interested in this treatment, please talk to your doctor.
Before and After Surgery
What can I expect before and after surgery?
How long will my valve last?
The amount of time your valve repair or replacement lasts depends on several things— your health at the time of surgery, the type of surgical treatment you have and how well you take care of yourself after the surgery. In some cases, valve repair surgery does not keep the valve fom getting worse, and you may need another surgery.
Mechanical valves rarely wear out, but they may need to be replaced if a blood clot, infection or tissue growth keeps them from working properly. Biological and homograft valves will eventually need to be replaced. This is especially true for younger patients who have a biological valve replacement.
What are the risks of major complication from surgery?
All surgery involves risks. These risks are related to your age, other medical conditions you have and the number of procedures you have done during a single operation. Your cardiologist and surgeon will talk to you about these risks before surgery. Please ask questions to make sure you understand all of the possible risks and why the procedure is recommended.
Will I Need to Take Blood-Thinning Medication (Anticoagulants) After Surgery?
Your doctor will let you know if you need to take an anticoagulant and for how long. If you have a mechanical heart valve, you will need to take an anticoagulant for the rest of your life. If you have mitral valve repair or a biological valve replacement, you may need to take an anticoagulant for several weeks after surgery, or maybe not at all. If you have a homograft valve, you will not need to take an anticoagulant. However, anticoagulants are sometimes used as treatment for other conditions related to valve disease.
These conditions include an enlarged heart, irregular heartbeat, a weakened heart and a history of blood clots. Anticoagulants have few, if any, side effects. They protect against stroke and generally do not disrupt normal living. There are some special precautions and instructions you will need to know about if you take an anticoagulant. Your healthcare team will go over this information with you.
Surgery details
Some of this information may not apply to you if you are having minimally invasive surgery or a transcatheter procedure. Please talk to your doctor or another member of your healthcare team if you have any questions about your surgery.
What happens before surgery?
Patients who are interested in having heart surgery at Cleveland Clinic can have a visit with one of our cardiologists or send in their medical records for the doctor to review. Then, the surgery is scheduled.
If you live far from Cleveland Clinic, please arrive in the area a few days before surgery.
Part of your preparation for surgery includes a presurgical appointment. You will have an evaluation and meet members of your healthcare team. You may also meet your surgeon and anesthesiologist. We will answer any questions you have, and you will get a surgical binder that contains helpful and important information about what to expect before, during and after surgery.
At this appointment, we will let you know when and where to go on the day of surgery. We will also let you know if you need more tests before your surgery.
Your presurgical appointment can take a whole day or longer, depending on the type of surgery you are having and any tests you need.
Procedure length
The amount of time your procedure takes depends on the type of procedure you are having. A general guideline is 3 to 6 hours, not including the time you spend in the prep and recovery areas.
Is the heart-lung machine used during surgery?
Yes. The heart-lung bypass machine is used during valve surgery to take over the work of the heart and lungs for a brief period of time. This keeps blood circulating throughout the rest of your body. Your heartbeat is stopped so the surgeon can operate on a “still” heart. This type of surgery is referred to as “onpump” surgery.
What happens after surgery?
After the valve has been repaired or replaced, the heart-lung machine is turned off, the heart starts beating on its own, and normal blood flow returns.
You may have temporary pacing wires and a chest tube to drain fluid. Sometimes a temporary pacemaker is attached to the pacing wires to keep your heart rhythm regular until your condition improves. Both the wires and the chest tube are put in place before you come out of surgery.
Stitches will be used to close your incision. These may be internal and/or external, depending on the type of surgery you have and the type of incision used.
You will stay in an intensive care unit (ICU) for a day or two after surgery. While you are in the ICU, we will closely monitor your heart, blood pressure, oxygen level and vital signs.
Your recovery continues in a special step-down nursing unit. You will be here for about 3 to 5 days, but the amount of time you spend in the hospital depends on the type of surgery you have and how quickly you recover.
Recovery
Your doctor will give you specific recovery guidelines, including information on activity, returning to work, how to care for your incision and general health guidelines. Every patient has a different experience after valve surgery. In general, you can expect to be sore and possibly tired for a while. This is due to the trauma from the surgery and is not a sign of how your heart valves are working. It may take 2 to 3 months to fully recover from surgery and most patients are able to drive 3 to 8 weeks after surgery. Your recovery time will be shorter if you have a robotic or minimally invasive procedure.
How you feel after surgery depends on your overall health, how the surgery went, and how well you take care of yourself after surgery. Patients with more severe symptoms before surgery may have a greater sense of relief after surgery. Call your doctor if you are concerned about your symptoms or the speed of your recovery.
Staying healthy
An important part of staying healthy after surgery is a healthy lifestyle and taking medications as prescribed. Depending on your lifestyle, you may need to make changes that include:
- Quitting smoking
- Treating high cholesterol
- Managing high blood pressure and diabetes
- Exercising regularly
- Maintaining a healthy weight
- Eating a heart-healthy diet
- Participating in a cardiac rehabilitation program, as recommended
- Following up with your doctor for regular visits
Follow-up care
Your first post-op appointment will be during the first week after you leave the hospital. If you are unable to come to Cleveland Clinic for this appointment, please let us know as soon as possible so we can make arrangments for you to see your local doctor. Your first appointment is very important. We will make sure you are taking the right types and amounts of medications and check for any problems with your healing and recovery.
Your next visit will be with your primary care doctor or cardiologist 6 weeks after you leave the hospital. Your doctor will check to see how your recovery is going, make sure you are taking the right types and amounts of medications, and give you the okay to return to normal activities like driving and working.
Medications, surgery and other treatments will not completely cure your heart valve disease. You will need to see your doctor for lifelong follow-up (exams and tests) to make sure your heart valves work as they should.
You will need regular appointments with your cardiologist at least once per year. Please be sure to keep these appointments, even if you do not have symptoms. Talk to your cardiologist about how often you need to be seen.
Call your doctor if you have any new symptoms or if your symptoms become worse or happen more often. Do not wait until your next appointment to tell your doctor about changes in your symptoms. All patients seen at Cleveland Clinic’s Heart, Vascular & Thoracic Institute have access to a phone line that is staffed by registered nurses 24/7. We are here to support you and answer your questions throughout your care and after you return home.
How to Protect My Valves
How can I protect my heart valves?
Bacterial or infective endocarditis is an infection of the heart valves or the heart’s inner lining (endocardium). It occurs when germs (especially bacteria, but occasionally fungi and other microbes) enter the blood stream and attack the lining of the heart or the heart valves. Bacterial endocarditis causes growths or holes on the valves or scarring of the valve tissue, which usually cause a leaky heart valve. Without treatment, bacterial endocarditis can be deadly.
To reduce your risk of bacterial endocarditis:
- Practice good oral hygiene habits every day. See your dentist every 6 months, brush and floss regularly, and make sure dentures fit properly.
- Call your doctor if you have symptoms of an infection, including a fever over 100 degrees F (38 degrees C); sweats or chills; skin rash; pain, tenderness, redness or swelling; a wound or cut that won’t heal; a red, warm or draining wound; sore throat, scratchy throat or pain when swallowing; sinus drainage, nasal congestion, headaches or tenderness along upper cheekbones; persistent dry or moist cough that lasts more than two days; white patches in your mouth or on your tongue; nausea, vomiting or diarrhea.
- Don’t wait to get treatment. Colds and the flu do not cause endocarditis, but infections, which may have the same symptoms, do cause endocarditis. To be safe, call your doctor and describe the symptoms and remind your doctor that you are a heart valve patient.
Who's at risk?
You are most at risk of developing bacterial endocarditis if you have:
- An artificial heart valve, including bioprosthetic and homograft valves
- Previous bacterial endocarditis
- Certain congenital heart diseases
- Heart valve disease that develops after heart transplantation
If you have any of these conditions, talk to your doctor about taking a preventive antibiotic before certain medical and dental procedures. Ask your doctor about the type and amount of antibiotic you should take, how much you should take, and which procedures require the medication. Follow the above tips to reduce your risk of infection.
A bacterial endocarditis identification card is available from the American Heart Association. Ask your doctor for a card or go to americanheart.org and search for “bacterial endocarditis wallet card.” Be sure to carry this card with you.
Patient Services
MyChart
Cleveland Clinic’s MyChart® is a secure, online tool that connects you to portions of your electronic medical record from the privacy of your home. Utilize this free service to manage your healthcare at any time, day or night. With MyChart you can view test results, renew prescriptions, request appointments and more. You can also manage the healthcare of your loved ones with MyChart • Caregiver.
- To register or learn more, log on to MyChart.
Chat with a Heart Nurse
For over 15 years heart, vascular & thoracic resource nurses have been offering assistance to people who have questions or concerns about heart, vascular and thoracic conditions. Nurses are available to help with questions on symptoms, diagnoses, treatment options, Cleveland Clinic services and doctors, etc. The nurses are available weekdays from 8:30 a.m. – 4 p.m., Eastern Time, through phone, secure live chat or email. If you need help, you may contact a nurse.
Appointments
Contacting Cleveland Clinic
Ready to Schedule an Appointment?
To make an appointment with the Valve Center - Call toll free 844.522.2193.
Virtual Second Opinion
Virtual Second Opinion program connects patients to the expertise of top Cleveland Clinic specialists without the time and expense of travel. Through our secure web platform, patients can submit their detailed health information, medical records and diagnostic test results. The most appropriate Cleveland Clinic expert is assigned to the consultation and will render a detailed second opinion. The report includes commentary about the diagnosis and treatment options or alternatives and recommendations regarding future therapeutic considerations. Patients are also able to send additional questions to the physician who provided the report. Online medical second opinions are available for more than 1,200 medical diagnoses.
Why Choose Us?
Why Choose Cleveland Clinic
Cleveland Clinic’s Sydell and Arnold Miller Family Heart, Vascular & Thoracic Institute is one of the largest centers in the United States for the diagnosis and treatment of heart valve disease.
Our cardiovascular imaging specialists use state-of-the-art procedures to determine the type and severity of heart valve disease and plan treatment accordingly. Our surgeons in the Department of Cardiovascular Surgery perform more than 3,000 heart valve surgeries each year. More than half of our heart surgery patients are considered complex; many have had previous surgeries or need more than one procedure at one time. We are also experienced in caring for younger patients who need to make life-long treatment decisions about their valve care and surgery.
Our medical teams are dedicated to research to help develop and bring into practice innovative approaches for the most advanced treatment available. Cleveland Clinic has made key contributions in the development of the transcatheter aortic valve (TAVR) approach and continues to play a role in expanding the use of it to more patients.
We perform valve repair and replacement of the mitral valve, aortic valve, pulmonic valve and tricuspid valve with approaches that work best for the individual. Many procedures can be performed through minimally invasive means and sometimes as a robotic-assisted surgery, all with the goal of helping patients return to an active life.
We invite you to review our outcomes and chat online with a Heart & Vascular nurse online to learn more.
Resources
Learn More
- Learn more about valve disease by visiting Cleveland Clinic’s Heart, Vascular & Thoracic Institute website
- Watch videos on valve disease presented by Cleveland Clinic specialists
- Read posts about valve disorders on our daily blog, Health Essentials from Cleveland Clinic
- Sign up for our e-newsletter, and get tips on maintaining a heart healthy lifestyle, recipes and essential health news









