Overview

Prostate cancer is the most common cancer in men, and the second leading cause of cancer death among men in the United States. Every year, about 185,000 new cases of prostate cancer will be diagnosed nationally. About one in six men will be diagnosed with prostate cancer during his lifetime, but only one in 35 will die of it. More than two million American men alive today have been diagnosed with prostate cancer at some point.
Prostate cancer is a malignant tumor that usually begins in the outer part of the prostate. In most men, the cancer grows very slowly. In fact, many men with the disease will never know they have the condition. Early prostate cancer is confined to the prostate gland itself, and the majority of patients with this type of cancer can live for years without any problems.
Prostate cancer is characterized by both “grade” and “stage.” The size and extent of the tumor determine its stage. Early stage prostate cancer, Stages T1 and T2, are limited to the prostate gland. Stage T3 prostate cancer has advanced to tissue immediately outside the gland. Stage T4 prostate cancer means it may have invaded adjacent structures such as the rectum, bladder and/or pelvic wall.
Diagnosis
Here is a look at the tools a physician will use to determine the aggressiveness of a prostate cancer. Fortunately, most prostate cancers have not spread at the time they are diagnosed, and the cancer is most often confined to the prostate gland.
Prostate-specific antigen (PSA) is a protein produced by the prostate gland. A screening test that measures the amount of PSA in the bloodstream has been in use since the late 1980s. Elevated PSA levels may indicate prostate cancer or other non-cancerous condition, such as prostatitis or benign prostatic hyperplasia (BPH)
A Gleason score, on the other hand, is used to estimate the aggressiveness of a tumor in an individual diagnosed with prostate cancer. A pathologist assigns a Gleason score after reviewing the prostate biopsy. The pathologist will assign a primary and a secondary score of 1 to 5 each, and the final score is the sum of these scores. In general, Gleason scores below 5 are not considered cancer; 6 are low-grade; 7 are intermediate-grade; and 8 to 10 are high-grade (the most aggressive cancers). In addition to Gleason scoring, a new Grade Group method is also used, with 1 being the lowest grade and 5 being the highest grade cancers
The tumor-nodes-metastasis (TNM) is used to estimate the extent of a cancer. The tumor (T) portion of the score describes the primary tumor status, ranging from T0 (no evidence of a primary tumor) to T4 (tumors that have spread and involve structures other than the seminal vesicles). The node (N) portion of the score describes lymph node status, ranging from NO (no regional node metastasis, or disease spread) to N3 (metastasis larger than 5 cm in any node). The metastasis (M) portion describes the level the disease has spread from MO (no metastasis) to M1 (distant metastasis).
The most appropriate treatment plan for a patient is created using a combination of PSA levels, Gleason score and TNM score.
Who should be screened for prostate cancer with a PSA test?
Recently, there has been some controversy regarding the effectiveness of routine PSA screening. Here’s the reasoning:
PSA doesn’t tell the whole story. It is important to understand that the PSA test is not perfect. Many men who do not have prostate cancer have elevated PSA levels. False-positive tests may lead to unnecessary biopsies. Also, low levels of PSA don’t necessarily rule out the possibility of cancer. And low-grade cancers found by a biopsy triggered by PSA may not need any treatment at all.
Other risk factors also are important. These include family history, age, race and free PSA (the percent of PSA in the bloodstream that is unattached to protein).
PSA isn’t the only test that is informative about the risk of prostate cancer. The OPKO 4K and PHI blood tests are additional alternatives. Both give a more accurate assessment of the risk of having a cancer that needs treatment.
The Future of Prostate Cancer Screening Is Here. Cleveland Clinic has partnered with Cleveland Diagnostics, Inc. to develop a more comprehensive PSA test. The test, known as IsoPSA®, can help zero in on molecular structural changes in PSA protein instead of just focusing on the concentration of PSA in the blood. A preliminary study in 2017 showed that IsoPSA® outperformed traditional PSA testing in predicting the overall risk of prostate cancer and the risk of clinically significant cancer, and a study in 2019 revealed that IsoPSA® could reduce unnecessary prostate biopsies by more than 40% while reliably determining the presence of high-grade disease.
Recently, the U.S. Preventive Services Task Force (USPSTF) upgraded their recommendation about PSA screening from a D grade (don’t screen) to a C grade, indicating that they believe that the decision about whether to be screened for prostate cancer should be an individual one, based on discussion with their physicians about the potential benefits and harms of screening. This upgrade was based on long-term results from the European Randomized Study of Screening for Prostate Cancer (ERSPC). This study showed that men ages 55 to 69 who were screened by PSA had a 25 percent reduction in the risk of dying of prostate cancer and a 35 percent reduction in the risk of needing palliative treatment for metastatic (advanced) prostate cancer compared to those who were not screened.
Our best advice: Consider your risk factors and discuss the pros and cons of getting a PSA or IsoPSA® test with your doctor.
To learn more about your personal prostate cancer risk, we offer an interactive risk calculator.
Fusion Guided Biopsy: A Targeted Way to Look for Prostate Cancer
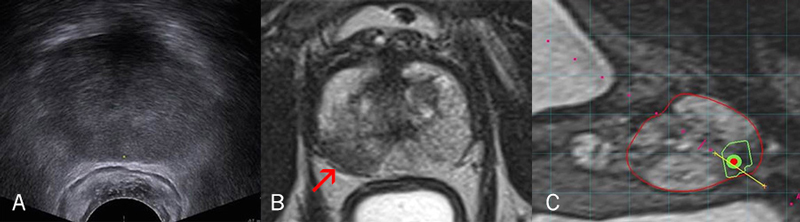
An ultrasound scan of the prostate (A) doesn’t provide as much detail as an MRI scan (B) does. The MRI reveals a dark area (arrow) that suggests a tumor. When the MRI and ultrasound images are fused (C), the surgeon has an even clearer target to biopsy. The prostate is outlined in red, the suspected tumor in green and the biopsy needle in yellow.
For men with an elevated PSA with or without prior biopsy, Cleveland Clinic urologists are using a new technology to look for prostate cancer. The approach is called fusion guided biopsy, which harnesses the power of high-resolution multiparametric MRI prostate imaging with real-time ultrasound-guided prostate biopsy to enable precise targeted biopsy of suspicious areas of the prostate that may harbor aggressive prostate cancer. It blends the power and detail of an MRI scan with the real-time convenience of ultrasound.
Here’s how it works: A patient first undergoes a specialized, high-resolution MRI scan, which is good at identifying suspicious areas in the prostate that may be cancerous. Later, in an outpatient setting, the urologist inserts an ultrasound probe into the patient’s rectum to examine the prostate. Special software “fuses” the images from the previous MRI scan with the live ultrasound images. The result is a threedimensional, highly detailed view of the prostate, highlighting the suspicious area so that a biopsy needle can be precisely positioned to obtain a sample for testing.
What you can expect if you are diagnosed with prostate cancer
At Cleveland Clinic, we tailor care to each patient, factoring in the type of cancer, age, whether the tumor has spread and overall health. However, the process of evaluation and treatment decision is similar for all men. Here is a general look at what you can expect if you are diagnosed with prostate cancer:
Your doctor will review your PSA levels, Gleason score and TNM score and meet with you to create an individualized treatment plan and arrange any additional testing that may be needed. If it is unlikely the cancer has spread outside the gland, staging studies such as bone scans and computed tomography scans may not be needed. If your cancer has a higher likelihood of spreading, you may need these studies or a PET scan to determine where the cancer may have spread.
Your doctor will discuss the plan and next steps with you and your family. Options may include active surveillance, surgery, radiation therapy, brachytherapy, cryotherapy, high-intensity focused ultrasound, hormone therapy or chemotherapy (see the treatment portion of this guide for more information on each).
Consider your options carefully. Unlike many cancers, prostate cancer usually allows a significant window of time to weigh your decision. (Your doctor will let you know if your cancer is aggressive, and if you need to begin treatment immediately). Take notes and ask questions. Make sure you understand all of the information before you and your physician agree on a course of treatment.
Once you have started treatment, you will have regular follow-ups with your doctor. The frequency of visits will depend on the aggressiveness of the cancer. In patients with no evidence of cancer after initial treatment, the usual recommendation is PSA testing every six months. Those with metastatic disease need more frequent testing and office visits to monitor their ongoing response to therapy.
Your Doctors
During the course of your diagnosis and treatment, there will be many team members involved in your care. These will include your:
Urologist
Your urologist specializes in the health of the male reproductive organs and urinary tract. A urologist will be the first specialist you will see if your primary care doctor suspects an issue with your prostate. The urologist performs any biopsies, surgery, cryotherapy, or brachytherapy (together with a medical oncologist) you may need.
Medical Genito-urinary oncologist
Aphysician with special training in the nonsurgical treatment of prostate cancer (such as immunotherapy, hormonal therapy and chemotherapy). Your medical oncologist will make your cancer diagnosis and recommend the best treatment options for you. He or she will oversee your progress throughout your entire treatment and help coordinate any care you may need from other specialists.
Pathologist
Laboratory tests are a vital part of diagnosis, treatment planning and monitoring of prostate cancer. Physicians rely on pathologists to provide expert diagnosis, second opinions and subspecialty consultation.
Radiation oncologist
A physician who specializes in administering radiation therapy (strong beams of energy) to kill cancer cells or keep them from growing and dividing. Radiation therapy, including intensity modulated radiotherapy, may be used in conjunction with surgery or chemotherapy to treat cancer.
Treatment Options for Early Stage Disease
Watchful Waiting or Active Surveillance
Watchful waiting, now more commonly called “active surveillance with selective delayed intervention,” requires no treatment for a discovered prostate cancer until your doctor detects signs that the cancer is growing more aggressively. This option is reserved for patients who have cancer that is confined to the prostate gland and that is defined as low to medium in aggressiveness. It is most often offered as an option to older men who are in poor health because it avoids potential risks and side effects of treatment. Active surveillance can be an option for younger men who want to avoid potential side effects of treatment or postpone it as long as possible.
What are the risks of active surveillance?
There is a chance that the slow-growing cancer could suddenly speed up in growth and spread beyond its original site or no longer be curable. Treatment can be riskier in older patients, increasing the chance of side effects and lengthening the recovery period. Also, patients have to be willing to return to the doctor’s office more frequently for blood tests, rectal exams and biopsies to check on disease progression. Worry about having cancer and knowing that it isn’t being treated may become emotionally overwhelming.
What are the benefits of active surveillance?
There is a good chance that a prostate cancer patient may never develop symptoms or require treatment. Even if the cancer grows, most prostate cancers grow very slowly. Newer treatments may be developed while cancer is under surveillance. Research has shown that at least for the first eight years, the life expectancy of men who choose this option may be no different than those who choose to treat their cancer aggressively. The risk of impotence and urinary incontinence associated with treatment also is avoided with active surveillance.
Using Genomics to Improve Active Surveillance
The current risk of being diagnosed with prostate cancer in the U.S. is 17 percent, while the lifetime risk of death is only 3 percent. This finding suggests that the majority of newly diagnosed prostate cancers do not require treatment, and active surveillance is an appropriate approach.
Despite this knowledge, surveillance is currently underutilized. About two-thirds of men diagnosed with low-risk prostate cancer continue to undergo immediate treatment with radiation or surgery. There are several reasons why surveillance hasn’t been more widely adopted, including patients’ fear of leaving cancer untreated and the lack of a way to distinguish slow-growing from aggressive tumors at the time of diagnosis.
Now, a new genetic-based test, developed at Cleveland Clinic with manufacturer Genomic Health, Inc. called the Oncotype DX Prostate, can help your doctor more accurately determine just how aggressive your cancer is. It defines someone’s risk and might help to determine best treatment strategies.
The test results, which are individual to each person based on his genetic information, create a Genomic Prostate Score (GPS) that ranges from 0 to 100. This score is combined with other factors to help doctors further determine prostate cancer risk before starting treatment. The test must be ordered by a physician, who will then get a report of the GPS, and can meet with you to share the results, discuss the implications and help you decide on the best options for you.
Surgery
Complete removal of the prostate — radical prostatectomy — is one of the most common treatments for prostate cancer.
Most of the surgical procedures for prostate cancer are done in ways that attempt to spare the nerves that control erections. These nerve-sparing surgeries reduce, but do not eliminate, the risk of incontinence and impotence.
What should a prostate cancer patient know about surgery?
A review of prostate cancer patients treated at Cleveland Clinic with robotic-assisted laparoscopic surgery, open radical prostatectomy, brachytherapy, cryotherapy and active surveillance found no difference in the rate of sexual function at all time points following treatment. The rates of urinary continence were similar with all treatments at six months.
This underscores the fact that the best indicator of surgical outcomes is the experience of the surgeon, not the technique used. Cleveland Clinic surgeons have a large experience with all methods of prostatectomy, and many new approaches have been developed here. Whether a patient has an open, laparoscopic or robotic prostatectomy, pain and recovery time are similar. Patients should learn their surgeon’s level of experience when examining treatment options.
Cleveland Clinic surgeons were the first in the world to use the single-port technique for prostate surgery.In this method, surgeons enter the body through a single incision. This minimally invasive approach is being offered at Cleveland Clinic to provide patients with an additional treatment option for prostate cancer.
Robotic surgery uses a computer-enhanced surgical system that provides:
- A 3-D view of the surgical field, including depth, magnification and high resolution
- Instruments designed to mimic the movement of the human hands, wrists and fingers, allowing an extensive range of motion and more precision
- Master controls that allow the surgeon to manipulate the instruments, translating the surgeon’s natural hand and wrist movements into corresponding, precise and scaled movements
Open Prostatectomy
During an open radical prostatectomy, the entire prostate is removed through an incision in the lower abdomen. Since the prostate wraps around the urethra, once it is removed the surgeon must reconnect the bladder with the urethra.
Robot-Assisted Surgery
Robot-assisted surgery, a type of minimally invasive surgery (MIS), uses robotic equipment to imitate surgical movements. MIS procedures allow surgeons to operate through small ports rather than large incisions. Surgical robotics combines minimally invasive techniques with highly advanced clinical technology. The results of robotic and open surgery are equal, with similar length of stay and recovery time. The most important factor in getting a good result is choosing a surgeon experienced in the technique.
How does the new technology assist the surgeon?
The 3-D vision system magnifies the surgical field up to 15 times and improves the surgeon’s ability to perform precise dissection of tissue, thereby reducing blood loss. Robot arms remain steady at all times and robot wrists make it easier for surgeons to manipulate tissue and work from all kinds of angles and positions they would have difficulty reaching otherwise.
What happens after surgery?
Following surgery, patients typically stay one or two days in the hospital. During this time, the staff checks patients daily and provides detailed post-operative instructions at discharge. Patients are able to continue follow-up either at Cleveland Clinic or with their local physician.
Radiation Therapy
Radiation therapy is the use of high-energy X-rays, electron beams or radioactive isotopes to kill cancer cells and eliminate tumors. Radiation ionizes or damages the chromosomes in the cell so that they cannot multiply. Radiation can be produced from a machine outside the body (external radiation) or by putting materials that produce radiation into the area where the cancer cells are found (internal radiation or brachytherapy).
Radiation therapy is a local treatment — aimed directly at the cancer. Like other treatments such as surgery or chemotherapy, both normal cells and cancer cells are affected. The body, however, is able to repair the healthy cells that have been damaged and restore them to their proper function. Cancer cells, however, cannot repair this damage and are rendered harmless. Successful radiation therapy depends on delivering the proper amount of radiation to the cancer in the best and most effective way, so that the normal cells still repair damage while the cancer cells are destroyed.
Here is a closer look at the different types of radiation therapy:
Brachytherapy
In this form of radiation therapy, radioactive pellets — each about 1/4-inch long and 1/32-inch thick are implanted in the prostate. These pellets can be temporary (removed after the proper dose is reached) or left permanently. The number of pellets implanted (up to 300 or more) depends on the size and shape of the prostate. The implant procedure takes about one hour and is done on an outpatient basis. Although the pellets deliver a higher dose of radiation than the external beam procedure, the radiation travels only a few millimeters and is, therefore, unlikely to extend far beyond the prostate, but still far enough to treat any extension of the cancer beyond the prostate gland.
Who is eligible for brachytherapy?
This therapy may work best in low, intermediate and some high-risk cancers and may not be a good option for men with more aggressive forms of prostate cancer, or cancer that has spread to other parts of the body.
What are the risks of brachytherapy?
Even though radiation does not travel far with this form of therapy, because of the prostate’s proximity to the urethra, brachytherapy may cause more acute urinary irritation than external beam therapy. Some patients (one in 10) need a catheter at times to help them urinate while the radiation remains most active, but this is rarely needed for more than a few weeks. Also, despite a low risk, because pregnant women and small children are more susceptible to the effects of radiation, patients undergoing brachytherapy are advised to not have pregnant women or children (under 18 years old) sit in your lap for more than 20 minutes per hour for the first two months.
What are the benefits of brachytherapy?
Cleveland Clinic began its prostate brachytherapy program in 1996. More than 5,000 patients have been treated since then. Our cure rates, as defined by PSA, are identical for up to 10 years as patients treated at Cleveland Clinic with radical prostatectomy or external beam radiotherapy.
Unique features of our Brachytherapy Program
- The first group to publish the improvements gained by treating patients within one session where the treatment planning and treatment occurs on the same day. This also results in lower cost and greater convenience for the patient since one less visit is necessary
- The lowest rectal side effect profile of any published series
- The largest series of patients with high-risk prostate cancer treated without hormone therapy or supplemental external beam radiation
External Beam Radiation
External beam radiation therapy is the most common form of radiation therapy. Before treatment begins, detailed planning or simulation is performed. During simulation, the specialists will use measurements from scans and calculations to determine the precise location to aim the radiation. Simulation may take up to an hour. During the treatment, the patient is positioned on a table so that a beam from a machine outside of the body may be aimed at the tumor. The radiation treatment itself lasts only a few minutes and is generally given five times a week for several weeks.
Some technical variations of external beam radiation are:
- High-dose, three-dimensional radiation therapy (3-DCRT)
- Intensity-modulated radiation therapy (IMRT)
- Image-guided radiation therapy (IGRT)
- Volumetric modulated arc therapy (VMAT)
What are the benefits of external beam therapy?
The benefits of this focused-beam therapy are that it minimizes damage to nearby tissue and structures and the treatment is not painful. Beam therapy can be used as an alternative to surgery to treat cancers that have spread into the pelvis and cannot be surgically removed, or to help reduce pain and shrink tumors in advanced disease that can’t be cured. Compared with surgery, incontinence is a less common occurrence and preservation of sexual function may be slightly higher. Cleveland Clinic pioneered hypofractionated intensity-modulated radiotherapy, in which large daily doses of radiotherapy precisely target the tumor while sparing surrounding healthy tissue. This may shorten the duration of prostate cancer treatment by several weeks. Cure rates as defined by PSA are identical for up to 10 years to those of patients treated at Cleveland Clinic with radical prostatectomy.
What are the side effects of external beam therapy?
The side effects of radiation therapy are, for the most part, specific to the area of the body being radiated. In the case of prostate cancer, the most common side effects requiring treatment are rectal bleeding and urinary stricture. General side effects of radiation may include skin irritation and fatigue. Radiation therapy as a treatment for prostate cancer also can cause erectile dysfunction and changes in urinary frequency and urgency.
There are medications and techniques that can be used to control side effects. Side effects should be discussed with the radiation oncologist so that they can be managed properly.
What about follow-up care?
After radiation therapy sessions are complete, patients visit the doctor for periodic follow-up exams and tests.
Why does organ motion during radiation therapy matter?
Internal organs move naturally during therapy and the prostate occasionally moves outside of the intended radiation field during treatment. Since doctors can’t predict which way — or how much — organs will move, the tumor may not get the right amount of radiation. In addition, other nearby tissue and organs may receive radiation they shouldn’t receive. At Cleveland Clinic, daily image guidance is used to precisely align the target and minimize dose to the organs nearby.
SBRT: New radiation therapy option may improve outcomes
A new, focused therapy being used at Taussig Cancer Institute — called stereotactic body radiation therapy (SBRT) — may prove a better option for prostate cancer patients than the gold standard of external beam radiation.
SBRT administers a series of five stronger, well-targeted doses of radiation to the prostate, with less radiation to surrounding tissue. This is quite simpler for patients than the roughly 40 treatment sessions required over an up to nine-week period required with external beam therapy.
Patients also benefit from SBRT’s ability to target the prostate with realtime tracking during treatment, which increases precision and further reduces the exposure to surrounding organs. Nearly all newly diagnosed prostate cancer patients are candidates for SBRT.
What about proton beam therapy?
A handful of sites nationwide are now offering proton beam therapy, a type of radiation therapy that uses protons (positively charged particles) to deliver radiation directly to tumors. These protons (versus the X-ray beams used in traditional radiation therapy) precisely target and kill the tumor cells, while minimizing damage to surrounding healthy tissue.
At Cleveland Clinic, we have chosen not to offer proton beam therapy. There is no long-term data to show that this option is any better than standard radiation therapy. Recently published research also suggests that complication rates with proton beam therapy are actually higher, not lower, than with standard radiation therapy.* At this time, we want to offer our patients only those therapies that have proven to be effective through long-term data and have the fewest side effects.
Ablation technologies
High-Intensity Ultrasound (HIFU)
A relatively new treatment for localized prostate cancer — high intensity focused ultrasound or HIFU— may help some men avoid surgery or radiation therapy. HIFU produces fewer side effects than more traditional treatments.
How does HIFU therapy work?
HIFU is a focal therapy technique that targets a specific area of the prostate rather than the whole gland. High-intensity sound waves target the tumor through an ultrasound probe inserted into the rectum. The probe heats to 80°C (176°F) and kills the cancerous tissue. The surgeon controls the probe’s movements with great precision using a robotic arm.
What are the pros of HIFU therapy?
- There’s less down time and pain. HIFU is an outpatient procedure, so no hospital stay is needed. The treatment generally lasts about an hour and, once a catheter is in place, the patient can go home. Patients typically do not need pain medications after HIFU because it isn’t as invasive as other treatments, and doesn’t involve a surgical incision or radiation.
- It has fewer side effects. Many men worry that they’ll lose the ability to get an erection after prostate cancer treatment. The inability to control the bladder is another common side effect of more traditional treatments. Men who opt for HIFU are less likely to have erectile dysfunction or urinary incontinence after the procedure.
- Other treatments are still an option. If HIFU isn’t effective and the cancer remains or returns, patients can still have other treatments, including surgery. Some treatment options such as radiation therapy generally aren’t used a second time because of increased risk for negative side effects.
What are the cons of HIFU therapy?
- It’s not right for everyone. HIFU is typically used only for localized prostate cancer (cancer that hasn’t spread outside the prostate) and it is best suited for men who are in the early stages of the disease. In more advanced stages when the cancer has moved beyond the prostate, HIFU therapy isn’t effective.
- It’s relatively new. As a treatment for prostate cancer, HIFU has been in use for about two decades outside of the United States. In the U.S., the Food and Drug Administration (FDA) approved HIFU for prostate-related treatment in October 2015. (The approval was for use in prostate tissue removal and not specifically for prostate cancer treatment.) HIFU has an 86 percent, five-year success rate in Europe for low-stage prostate cancer. And close to 80 percent of those treated have remained free of cancer for seven years.
- It’s not widely available. Because of the fairly recent FDA approval, not all hospitals offer the treatment. Cleveland Clinic began offering HIFU in 2017. Men should discuss this and other treatment options with their physician.
Traditional treatment for high-grade or locally advanced prostate cancer (Gleason score eight or above) or tumors that have minimal spread beyond the prostate gland (clinical stage T3) has been a combination of hormones and high-dose external beam radiation. While this remains a good choice for many men, especially if they are older or have associated medical issues, Cleveland Clinic surgeons have gained substantial experience with surgery for more advanced cancer in the past 10 years. Potential advantages of surgery include the ability to perform an extended lymph node dissection, which can yield important information about prognosis and may be curative in men with minimal disease in the lymph nodes; complete pathologic staging of the removed prostate, allowing an informed decision based on the potential benefits of post-surgical (adjuvant) radiation; avoiding or delaying the need for hormone therapy and avoiding the potential late side effects of external radiation. Some men may be eligible for participation in clinical trials of medication given prior to surgery (neoadjuvant therapy), an approach pioneered by physicians working in tandem in the Taussig Cancer and Glickman Urological & Kidney Institutes.
Cryotherapy
In this treatment, four to eight small needle-shaped probes are inserted into the prostate in order to freeze the gland to temperatures lethal to prostate cancer cells. This minimally invasive, incision-free procedure is performed either as an outpatient procedure or one-night hospital admission. With this treatment, patients recover in a matter of days and usually experience minimal after effects.
Cleveland Clinic urologists have extensive experience in using cryotherapy for treatment of prostate cancer both as initial therapy and for recurrence of cancer following radiation therapy. This treatment can be used in three ways:
- For treatment of the entire prostate upon first diagnosis of prostate cancer
- For “salvage” therapy to treat cancer that has recurred in the prostate following prior therapy such as radiation or brachytherapy
- For treatment of only the affected portion of the prostate, called “focal therapy.” Focal therapy can be used in select men whose cancer is small enough that it may be controlled with less widespread freezing
How does cryotherapy work?
Cryosurgeons use 3-mm or smaller diameter cryoprobes (needles) supercooled with argon gas, inserted through the skin into the prostate under ultrasound guidance. The target tissue is repeatedly frozen to -40 degrees Celsius, resulting in tumor destruction.
What are the risks associated with cryotherapy?
As with any prostate cancer therapy, cryotherapy can potentially cause side effects or damage to adjacent organs. Damage to the urethra is minimized by the use of a urethral warming catheter that circulates warm fluid through its chambers. Damage is also minimized by precise monitoring of temperature using probes placed near vital areas.
How is the procedure performed?
- Primary cryotherapy — Four or more cryoprobes are placed into position. Freezing begins slowly under ultrasound and computer monitoring. When the ice ball reaches a lethal chill, the argon is turned off and helium is turned on to thaw the gland. The process is repeated as soon as it is thawed, and the entire procedure is completed within two hours. Following surgery most men are permitted to return home within 24 hours, usually on the day of the procedure. A catheter may remain in place for seven to 10 days.
- Focal Cryotherapy — Traditional treatment of prostate cancer targets the entire gland because at least 80 percent of men have small “satellite” tumors in various sites throughout the prostate. In selected patients in whom a dominant or solitary tumor can be identified, cryotherapy can be limited to this one area. Focal therapy is most commonly used for men wishing to minimize the likelihood of impotence.
- Salvage cryotherapy Although external beam radiation and brachytherapy are highly effective, some patients will experience recurrence of cancer following treatment. Primary and focal cryotherapy, described above, can be used to treat patients whose cancer recurrence is limited to the prostate.
In addition to urethral slough (shedding dead cells), incontinence and impotence can occur after cryotherapy. A very rare complication is a fistula, a hole that develops between the urethra and rectum and that requires surgical repair. These complications are more common for salvage cryotherapy.
Who is eligible for cryotherapy?
The most important requirement for cryotherapy is having cancer limited to the prostate. Like other local therapies (prostatectomy and radiation), cryotherapy works only if cancer is contained in its targeted site. Men with large prostates — measuring greater than 70 to 90 grams on ultrasound — may require hormone therapy to shrink the gland prior to treatment.
Treatment Options for Advanced Stage Disease
When disease spreads, or metastasizes outside the prostate region, the folowing therapies are commonly used:
Hormone Therapy
Hormone therapy is a prostate cancer treatment that decreases the level of the male hormone testosterone to slow the growth of the tumor. This may be accomplished with drugs that cause the cells that make testosterone to stop, or with surgery that removes the testes, where most testosterone is produced. Hormone therapies can’t cure advanced prostate cancer, but can be given alone or in combination with other forms of treatment in the hopes of improving quality of life, extending survival or both.
Research on the value and effects of hormonal therapies is ongoing. The most common form of hormone therapy uses drugs referred to as leutinzing hormone releasing hormone agonists, or LHRH agonists. Examples of these drugs include triptorelin (Trelstar®), leuprolide (Lupron®, Eligard®, Vantas®) and goserelin (Zoladex®). Blocking testosterone slows the rate of cancer growth. A different class of drugs, the antiandrogens flutamide (Eulexin®), bicalutamide (Casodex®) and nilutamide (Nilandron®), work by preventing the body — and thus the cancer cells — from using testosterone.
A new class of drugs called androgen biosynthesis inhibitors are oral agents that selectively block the production of hormones from the adrenal gland responsible for prostate cancer growth. The first drug in this class is abiraterone acetate (Zytyga®). Similarly, enzalutamide (Xtandi®), a new and more powerful antiandrogen was also recently approved by the FDA. These are important drugs that have changed the management of men with advanced prostate cancer. The timing of their use varies and is routinely individualize based on the needs of the patient. At the present time however these agents are restricted to men with advanced disease who are no longer responding to hormone therapy or to those who have received chemotherapy and are in need of additional treatment.
What are the risks of hormone therapy?
Hormone therapies that decrease testosterone are associated with many side effects including lowered libido, impotence, hot flashes, weight gain, breast tenderness and enlargement, loss of muscle and bone mass, and fatigue. Hormone therapy has been associated with increased risk of metabolic syndrome, diabetes, reduction in HDL (“good” cholesterol) and cardiovascular disease. While it’s possible that hormone therapies may delay death, they cannot prevent it. Eventually, advanced prostate cancer can become resistant to hormone therapy and that therapy no longer works. When this occurs patients can receive additional FDA approved treatments proven to extend survival.
What are the benefits of hormone therapy?
Hormone therapy can shrink tumors, thus reducing symptoms and pain, and possibly extending the lives of men with prostate cancer. It can also shrink the prostate and improve the outcome with radiation therapy.
When is hormone treatment used for prostate cancer?
Hormone treatment does not cure cancer. The purpose of hormone therapy is first to delay the progression of the cancer, and second to increase survival while maximizing quality of life. If the patient doesn’t respond to initial hormone treatment, the doctor might try other hormonal methods before recommending another form of treatment.
Who is a candidate for hormone treatment?
Hormone treatment is often used in men receiving radiation to the prostate. Men whose disease has spread to the bone or lymph nodes will typically receive hormone therapy. Patients and their physicians must consider the effects on quality of life, cost of the treatment, and how effective and safe the treatment is likely to be for that individual.
Immunotherapy
Enhancing someone’s immune system to become more effective at killing cancer cells has been recognized as a potential treatment strategy in prostate cancer. Sipuleucel-T (Provenge®) represents a novel immunotherapeutic compound (made with a patient’s own cells) designed to stimulate the natural ability of immune cells already in the blood to attack prostate cancer cells more effectively and extend survival.
How is Sipuleucel-T made?
Patients undergo blood collection and their dendritic cells (scavenger cells in our body that look for foreign material) are isolated and sent to a central processing facility where the cells are cultured and treated to recognize prostate cancer more effectively. Following this, the product is returned to the healthcare provider where it is administered intravenously to the patient. Blood collection, processing and treatment administration is every two weeks, for a total of three infusions.
What are the side effects?
There are minimal side effects with this treatment. Outside the blood collection process, administration of Sipuleucel-T (Provenge®) can lead to fever, chills, muscle pain and headaches. Contrary to other immunotherapies, no concerns for autoimmunity exist.
Chemotherapy
Chemotherapy involves the use of drugs to kill cancer cells. Chemotherapy may be taken orally or injected into a vein. Chemotherapy is usually a systemic treatment, meaning the drugs enter the bloodstream, travel through the body and can kill cancer cells anywhere in the body, including the prostate.
Chemotherapy is given in cycles of treatment followed by a recovery period. The entire chemotherapy treatment generally lasts three to six months, depending on the type of medications given.
When is chemotherapy given?
Until recently chemotherapy was reserved for patients with advanced prostate cancer in whom hormone therapy no longer is effective. A recent U.S. trial demonstrated a significant survival benefit when chemotherapy is given up-front with hormone therapy to men with advanced disease. Patients presenting with distant metastases should discuss the need for this approach with their treating physician. Chemotherapy is given to cause the cancer to shrink and/or disappear. Even if the cancer is not eliminated, symptoms may be relieved. Metastatic disease may be present at diagnosis or, in some cases, cancer can return in a distant location months or years after initial treatment.
What are the side effects?
Because chemotherapy acts to kill rapidly dividing cancer cells, it also kills other rapidly dividing healthy cells in our bodies, such as the membranes lining the mouth, the lining of the gastrointestinal tract, the hair follicles and the bone marrow. As a result, the side effects of chemotherapy relate to these areas of damaged cells. The good news is that the damaged noncancerous cells will be replaced with healthy cells, so the side effects are only temporary.
The specific side effects depend on the type and amount of medicines given and for how long. The most common, temporary side effects of chemotherapy include nausea and vomiting, loss of appetite, hair loss, mouth sores and diarrhea.
There are medications available to control certain side effects, such as nausea and vomiting, or diarrhea. Although it may take some time, side effects related to chemotherapy will resolve when chemotherapy is stopped.
Radionucelotides
Radionucleotide therapy is the use of radioactive isotopes to kill cancer cells. Until recently, bone-targeting radioisotopes — strontium-89 (89Sr), samarium-153 lexidronam (153Sm) — were commonly used in to treat men with prostate cancer with extensive multifocal painful bone metastases. Although these agents yield some symptom improvement, they did not extend survival.
Recently, Radium-223 (Xofigo®), an alpha particle emitting radiopharmaceutical was FDA approved for men with advanced prostate cancer and painful bone metastases in whom disease has progressed after hormone therapy. This treatment extends survival and is capable of delaying bone complications from prostate cancer (called skeletal symptomatic events).
How is Radium-223 administered?
Once patients are deemed candidates for this treatment by their medical oncologist, Radium-223 is administered intravenously by a trained nuclear medicine physician once a month for six months. Radium-223 targets the bone compartment only. This radiation is deadly to the cancer cells in your bones but does limited damage to nearby healthy cells. During treatment with Radium-223, patients undergo blood testing and are evaluated by their medical oncologist prior to each administration.
What are the side effects?
Radium-223 can be absorbed by organs other than bone, primarily the bone marrow and digestive system, which can result in side effects in those healthy tissues. Nausea, diarrhea, vomiting, fluid retention in legs or feet and low blood counts can occur. Unlike with other radionucleotides, there are no restrictions regarding contact with other people immediately after treatments.
Patient Services
Medical Concierge
Complimentary assistance for out-of-state patients and families. 800.223.2273, ext. 55580, or email medicalconcierge@ccf.org.
Global Patient Services
Complimentary assistance for national and international patients and families. Call 216.444.6404 for more information.
MyChart
Cleveland Clinic MyChart® is a secure, online personal healthcare management tool that connects patients to their medical record. Patients can register for MyChart through their physician’s office or by going online.
Appointments & Locations
Still have questions about prostate cancer?
If after reviewing this guide you have additional questions, Cleveland Clinic’s Cancer Answer Line can help. Two oncology clinical nurse specialists and their staff can provide information and answer questions about cancer.
The Cancer Answer Line is operational from 8 a.m. – 4:30 p.m., ET, Monday – Friday. Please call toll-free 866.223.8100.
Ready to schedule an appointment with a prostate cancer specialist?
If you would like to set up a consultation with a Cleveland Clinic specialist, please call the Cancer Answer Line toll-free at 866.223.8100. Same-day appointments are available.
Locations
Cleveland Clinic Cancer Specialists are located in Cleveland, regionally throughout Northern Ohio and in Florida. View a complete list of cancer care locations.
Virtual Second Opinion
If you cannot travel to Cleveland Clinic, help is available. You can connect with Cleveland Clinic specialists from any location in the world via a phone, tablet, or computer, eliminating the burden of travel time and other obstacles. If you’re facing a significant medical condition or treatment such as surgery, this program provides virtual access to a Cleveland Clinic physician who will review the diagnosis and treatment plan. Following a comprehensive evaluation of medical records and labs, you’ll receive an educational second opinion from an expert in their medical condition covering diagnosis, treatment options or alternatives as well as recommendations regarding future therapeutic considerations. You’ll also have the unique opportunity to speak with the physician expert directly to address questions or concerns.
Why Choose Us?
Through a multidisciplinary approach, Cleveland Clinic specialists in the Taussig Cancer Institute work with urologists in the Glickman Urological & Kidney Institute to explore all medical and surgical options to ensure that our prostate cancer treatment program will result in a successful outcome for each patient.
Many prostate treatment methods were pioneered here, giving us one of the world’s largest experiences in treating localized cancer using surgical and non-surgical methods.