The CTICU
When you wake up, you will be in the Cardiothoracic Intensive Care Unit (CTICU). A team of specially trained physicians and nurses will monitor your care and help you recover safely and quickly.
The CTICU is a busy place. You can expect bright lights and many noises. These noises are the monitors and different types of equipment. Many of these machines continuously monitor your heart rate and rhythm and blood pressure to help your surgeon determine how well your heart is functioning. Try to tune the equipment noises out and relax.
Endotracheal Tube
You will become aware of the endotracheal tube (breathing tube) that was inserted while you were asleep. The tube is connected to a respirator that assists your breathing. While it is in place, you will not be able to talk or swallow.
The nurse will anticipate your needs and ask you questions that require only a yes or no answer. Nod or shake your head yes or no. The breathing tube will be removed when you are fully awake and able to breathe on your own. Once it is removed, you will be able to talk, however you may have a sore throat and a hoarse voice.
Deep breathing and coughing exercises, as well as changes in position, are extremely important to prevent postoperative pneumonia.
Deep Breathing and Coughing Exercises
When the breathing tube is removed, the nurses and respiratory therapists will help you do deep breathing and coughing exercises to inflate your lungs and cough out any secretions that have settled in your lungs during surgery.
Changing Positions
You should change your position frequently while in bed.
Drainage Tubes
You will have drainage tubes, called "chest tubes", to drain fluid which accumulates around your heart and lungs during surgery. The drainage from these tubes will be bloody at first. The tubes are removed when the drainage is clear and decreases in amount.
IV Lines
Fluids and medications are administered through an IV line in your neck. Immunosuppressant drugs will be administered through this IV until you are able to take fluids and eat.
Pain
You may experience pain when you first wake up. You will be given medications to control pain. Our pain control program is designed to keep you as comfortable as possible. However, if the medications affect your breathing and/or blood pressure, your physician may decrease the amount of pain medication given to you.
If you would like to use other methods of pain control, such as soothing music or relaxation tapes, small tape players with headphones are allowed in the CTICU.
Change in Heart Rate
It is normal for your new heart to beat faster at rest. Also, your heart rate will not rise as quickly with increases in activity. This may cause you to feel light-headed if you get up too fast from a resting position. You will need to get up slowly from lying or sitting and will need to warm-up when exercising.
Length of Stay
The length of stay in the CTICU varies with each patient. Your transplant team will determine the best time to be transferred to the Transplant Special Care Unit. This usually takes place within 2-3 days after transplant.
Types of Infections
Because you are taking immunosuppressant medications, certain viruses or bacteria which are normally harmless can cause you to become sick. These are called "opportunistic infections." The types of infections include:
- Bacterial
- Viral
- Fungal
- Other (pneumocystis and tuberculosis)
Bacterial Infections
- Bacterial infections are the most common types of infections that can occur after transplant. Bacteria are found on the skin or in body cavities. Normally, these bacteria do not cause problems, but may lead to infections when you are taking immunosuppressant medications.
- Bacterial organisms include staph, strep, and pseudomonas, among others.
- Bacterial infections may occur at any site within the body including the blood, lungs, urinary system, and incisions. If a bacterial infection is suspected, you will need to come to the hospital for blood, urine, and sputum cultures.
- A culture involves taking a sample of your blood, urine, or sputum (phlegm). The sample is evaluated under a microscope 24, 48, and 72 hours after it is taken to detect evidence of any bacterial growth. If bacterial growth is found, it is identified and tested against the panel of antibiotics to determine which antibiotic is effective in killing that bacteria. You will start taking an antibiotic either by mouth or intravenously (IV), depending upon the severity of the infection.
- It is very important to finish all of the prescribed antibiotics, even if you are feeling better after a few days. If all of the antibiotics are not taken, some of the bacteria may not be killed, and will continue to multiply, causing another infection that may be resistant to the original antibiotic.
Viral Infections
- Viruses are the most common cause of infections in transplant patients after the first month. Viral infections include:
- CMV (Ganciclovir)
- Herpes (simplex or zoster)
- Hepatitis
- During the pre-transplant screening, you were tested for previous exposure to CMV, herpes, hepatitis, and HIV.
- Testing positive for previous exposure to hepatitis B or C would not prevent you from being considered for transplant if there is no liver damage present.
CMV (Ganciclovir)
- CMV is a common infection following heart transplant, accounting for about 25 percent of all post-transplant infections. More than half of all Americans have had previous exposure to CMV, a benign illness, causing flu-like symptoms. If you or your donor had prior CMV exposure, you will be treated with oral valganciclovir for month one, then acyclovir for months two and three after the transplant to prevent CMV infection from occurring.
- When you are taking immunosuppressant medications, CMV may cause a more serious illness and may result in hospitalization. Symptoms can range from feeling "lousy", fever, chills, diarrhea, abdominal pain, headache, cough, or flu-like symptoms. Call your doctor if any of these symptoms occur.
Herpes
- The herpes virus may affect as many as 40 percent of the transplant population. Once you have herpes, it lives in a dormant state in your body. Sometimes, it becomes active and most commonly presents itself as a cold sore or fever blister on your lips, esophagus, genital area or anus. If you have had a herpes sore in the past, you will most likely have one again, often in the same place.
- The herpes virus can also appear as "shingles." Shingles are painful blisters along the pathways of nerves on the surface of the skin. The most common sites are the chest, sides of abdomen, and face.
- Avoid anyone with active chicken-pox. It can cause a more severe infection in transplant recipients who were never exposed to the virus, or it may cause shingles in those who previously had chicken-pox.
- Herpes is not life-threatening, but it can be uncomfortable. To prevent a more serious infection, take your herpes medication (Acyclovir) at the first sign of a herpes sore. Acyclovir may be given intravenously, by mouth, or as a topical cream, depending upon the severity of the illness.
Hepatitis
- There are several types of hepatitis: Type A, Type B, and Type C.
- Hepatitis may be contracted through hepatitis-contaminated blood, body secretions, dirty needles, food, contaminated water, sexual intercourse or exchange of body secretions.
- Symptoms of hepatitis include:
- Jaundice (yellowing of the skin)
- Nausea
- Vomiting
- Abdominal pain
- Fever
- Weakness
- Fatigue (feeling over-tired)
- Treatment of hepatitis is difficult, and prevention is best.
- Some patients may receive a heart from a donor who tested positive for hepatitis B or C, but who had no symptoms or clinical history of hepatitis. In this case, special follow-up after transplant may be required.
HIV
- HIV is the virus that produces AIDS (acquired immune deficiency syndrome). The HIV virus may be contracted through sexual contact (heterosexual or homosexual), contaminated blood products, intravenous drug use with contaminated needles, or from mother to child by way of the placenta or birth canal.
- There is an extraordinarily small chance that HIV virus may be contracted through an organ transplant. All blood, organ, and tissue donors are thoroughly screened for HIV infection through a careful screening of medical and sexual history and by blood testing. The history of the donor is obtained as completely as possible because blood testing may not be 100 percent sensitive for the virus.
- Although there is a very small chance that you could contract HIV through an organ transplant or blood transfusion, you must know that every precaution has been taken to assure that the organ and blood are safe. Every effort is made to select donors who will not transmit infection. The transplant team always attempts to make recommendations in your best interest.
Fungal Infections
- Fungal infections may range from very mild (thrush) to life-threatening. Examples of fungal infections include:
- Candida
- Aspergillosis
- Histoplasmosis
Candida
- Candida is a yeast that grows in moist areas of the body, such as the mouth, arm pits, groin or genital area. Candida is also known as thrush or monilia.
- When it occurs in the mouth, it looks like white, fuzzy patches over the roof of your mouth, on your tongue, your throat, or in your esophagus (the tube that goes from your mouth to your stomach). It can be treated with a mouthwash (Nystatin) or troches (Mycelex).
- When it occurs on the skin, candida can be treated with several types of lotions or creams.
- Women can get yeast infections in the vagina. Vaginal yeast infections cause itching and drainage that is white, lumpy and foul smelling.
- If Candida spreads inside the body, it can become a more serious infection, requiring intravenous treatment with antifungal medications such as Amphotericin B.
Aspergillosis
- Aspergillosis may be contracted by breathing fungal spores in damp, dusty places such as attics, basements, barns, or constructions sites.
- Care should be taken to avoid these places, or if necessary, wear a face mask in those areas.
Histoplasmosis
- Histoplasmosis is an air-borne fungal disease found in bird droppings.
- Transplant recipients should avoid exposure to bird droppings, especially in enclosed areas.
Other Infections
Pneumocystis
- Pneumocystis is a pulmonary (lung) infection that occurs mainly in patients who are taking immunosuppressant medications. Symptoms include cough, fever, malaise (feeling lousy), and shortness of breath. Transplant patients are given Bactrim DS every other day for the first year after transplant to help prevent this infection. Patients who are allergic to sulfa drugs may be treated with Pentamidine Aerosol every four to six weeks, or Dapsone instead of Bactrim.
Tuberculosis
-
Tuberculosis (TB) is a mycobacterial infection that is contracted by breathing infected air-borne droplets. Potential transplant recipients may receive a skin test during the transplant evaluation to determine previous exposure to TB.
Symptoms of tuberculosis include:
- Pneumonia-like symptoms
- Cough
- Coughing up blood
- Night sweats
- Fever
Your immune system is made up of mostly white blood cells that fight infection. It can also work against your new heart, treating it as an unwanted, foreign object. To prevent this from occurring, you take immunosuppressant medications - to suppress or work against your natural immune system so that rejection does not occur.
However, the same medications that help prevent rejection also increase your risk for infection. For the first six months after surgery, the likelihood for rejection is highest, so you will be taking higher doses of these medications. This makes you even more vulnerable to infection. You must take caution to protect yourself from infection.
Recovery at Home
Recovery after your heart transplant is similar to the recovery after any heart surgery. It takes about six to eight weeks for your incisions to heal.
At first, you may have some muscle or incision discomfort in your chest during activity. Itching, tightness, or numbness along your incision are also normal. Follow the guidelines below to ensure proper healing:
Keep your incisions clean and dry.
- If your incisions are healing you may take a shower (no longer than 10 minutes).
- Use gentle soap and water to cleanse the site. Do not saturate.
- Do not rub your incisions with a washcloth until the scabs are gone and the skin is healed.
- Do not use any ointments, lotions or dressings on the incision.
Protect your incision.
- Do not drive a car for six to eight weeks after your surgery. Your cardiologist will clear you to drive.
- Do not lift anything over 10-20 pounds for six weeks after your surgery.
Nutrition.
Good nutrition is an important part of healing. You will need to eat a diet that is low in salt and fat, but also one that includes a variety of healthy foods to help you heal. If you are having trouble with your appetite or understanding your dietary guidelines, please ask your transplant team to speak to a dietitian.
Signs of infection - what to look for.
If you have any of these signs of infection, call your doctor.
- Increased drainage and/or oozing from the incision
- Increased opening of the incision
- Redness around the incision
- Warmth along the incision line
- Increased body temperature (greater than 101 degrees F or 38.4 degrees C)
Call your doctor:
- If you have any signs of incision infection.
- If your sternum (breastbone) feels like it moves, or it pops or cracks with movement.
Taking your medications as directed
You will need to take medications the rest of your life to prevent your body from rejecting your new heart and to treat other medical problems. Always take your medications as directed. By the time you leave the hospital, you should be taking all of your medications without help from the nurses.
You must know:
- The names of your medications and what they look like
- What they are used for
- The dosage (how much to take and how often)
- The possible side effects
- What times to take them
Points to Remember
- Always report changes in your condition to your transplant coordinator or transplant cardiologist.
- Never stop or change your medications without first consulting your transplant coordinator or transplant cardiologist.
- Always call the transplant coordinator before taking any new medications other than those prescribed by the transplant team. This includes any over-the-counter medications, nutrition supplements or herbal therapies. Some medications may interact with your transplant medications and cause side effects. For example, St. John's Wort affects your cyclosporin level and should never be taken after transplantation.
- Take your medications at the same time every day. Develop a system that helps you remember to take your medications at the right time(s) each day. Keep a record of your medications and when you take them. Bring an updated list of your medications and records to each follow-up appointment.
- If you forget to take a dose, resume your normal medication schedule.
- Do not take a double dose at one time.
- If you are ill and vomit soon after taking your medication or have diarrhea for more than one day, call your doctor. Do not take a second dose of your medication without talking to your doctor.
- Special containers, such as weekly pill boxes may help you remember to take your pills. But, store all remaining medications in their proper containers, with medication name, dosage, and expiration date listed, to avoid confusion and loss of potency.
- Keep all medications in a dry place, away from moisture, heat, or direct light.
- Keep all medications with you when you travel. Do not pack them in suitcases that may be lost or detained.
- Always bring your medications with you to your follow-up visits.
- Don't wait until you're almost out before you refill your prescriptions. Some pharmacies need to order your immunosuppressants, so keep ahead of schedule. Check your supply before vacations, holidays, and other occasions when you may not be able to obtain it. Your Transplant Coordinator is available to call in refill orders to your pharmacy during normal office hours (Monday through Friday 8:00 a.m. - 4:00 p.m.)
- Talk to your transplant coordinator if you are uncertain about a medication or its dose.
- Call the transplant team if you have any side effects.
Immunosuppressive Drugs
- Cyclosporine
- Azathioprine
- Mycophenolate Mofetil
- Prednisone
- Tacrolimus
Anti-Infective Agents
- Co-trimoxazole
- Acyclovir
- Ganciclovir
- Nystatin
- Clotrimazole
Anti-Ulcer Medications
- Ranitidine
- Famotidine
- Omeprazole
Anti-Hypertensive Medications
- Calcium Channel Blockers
- ACE Inhibitors
- Clonidine
- Minoxidil
- Diuretics
Lipid Lowering Medications
These medications are used in conjunction with a low-cholesterol diet to help reduce your lipid levels and to help reduce the risk of traditional and/or transplant coronary artery disease.
Preventing Infection at Home
Remember these points to protect yourself from infection:
- Take care of cuts or wounds and wash hands thoroughly:
Keep minor cuts and wounds clean. Wash them with soap and water or hydrogen peroxide, dry your skin and cover the cut with a sterile bandage.
Go to the emergency room near your home if you have a deep cut, or one that bleeds a lot. Be sure to tell the health care providers that you are a transplant patient.
Call your doctor if your wounds become red and drain anything but clear liquid.
Frequently wash your hands with soap and warm water, especially before preparing food, and after using the bathroom or after touching soiled linens or clothes. Lather well, rubbing your hands back and forth together, to clean all surfaces, including the nail beds and webbing between your fingers.
Shower or bathe daily using a mild soap. Special soap is not needed at home. If you have dry skin, apply a mild skin lotion after bathing.
Prednisone and cyclosporine, two medications that you must take, can cause acne.
Keep your skin as clean and oil free as possible and use a washcloth and mild soap. You may want to avoid soaps that contain pumice or coconut oil. Some over-the-counter acne products may be helpful, but be sure to use non-comedogenic skin care products and cosmetics
Make an appointment with a dermatologist (skin doctor) if acne becomes a problem.
Overexposure to the sun can also cause skin irritation as well as cause dry skin, sunburn, blisters and can increase the risk of skin cancer. Some of your medications may make you more sensitive to the sun's rays.
Always wear a sunblock lotion, sun protective factor (SPF) of 15 or greater when outdoors in bright sunlight. Wear a broad-brimmed hat and protective clothing such as light pants instead of shorts, long-sleeved shirt, and socks to protect your feet and lower legs. When swimming, wear a T-shirt over your bathing suit.
Check your skin for new markings; especially new irregular shaped, raised, red, black or brown markings. If you notice any new skin markings, see a skin doctor (dermatologist) for prompt evaluation and treatment.
- Practice good dental hygiene:
In some patients, cyclosporine (Neoral) can cause gums to swell, become tender, and sensitive to heat and cold. Poor diet can also cause gum disease. Sore, bleeding gums can easily become infected. Good dental care may help prevent infection.
Examine your mouth and gums every day. If you have red or swollen gums, contact your transplant coordinator. Be sure to brush your teeth and gums thoroughly after each meal with a small, soft toothbrush and fluoride toothpaste. Use foam sticks instead of a toothbrush if your gums are especially sore. Also use dental floss every day and keep dentures clean and fitting properly.
Your doctor may tell you to use an antibacterial mouthwash rinse. Avoid commercial mouthwashes or throat lozenges that contain a high concentration of alcohol - they may irritate or dry your mouth.
Prepare a gargle by dissolving one teaspoon each of salt and baking soda in a quart of warm water. (A smaller portion of this can be made by stirring 1/4 teaspoon each of salt and baking soda into eight ounces of warm water.) Rinse your mouth and gargle with this solution at least four to six times a day, especially after meals and before going to bed.
Have your teeth cleaned and checked by a dentist at least every six months. Tell your dentist that you have had a transplant before your appointment so he or she can take precautions to prevent possible infection. Also be sure to call your transplant coordinator for an antibiotic prescription at least one week before any of your dental appointments.
If a mouth sore develops, eat foods that are warm or at room temperature and avoid eating acidic foods and beverages (such as tomatoes and oranges).
- Take action to prevent infection by avoiding people who have colds or the flu:
Friends and family will want to visit you when you return home. It is important to teach them how they can help you best.
Limit your visitors for the first couple weeks and instruct visitors to avoid sending or bringing live plants. If your visitors have cold or flu symptoms, ask them to return when they are feeling well. Before visiting with an infant or child, check with the Transplant Team.
- Keep your immunizations current:
Get a flu shot every fall (by October 15). You cannot get the flu by getting the immunization. Encourage your adult family members to get flu shots also. You can arrange to get the flu shot from your doctor or Transplant Team.
Ask your doctor if you should get a pneumovax (pneumonia) vaccine. Ask your doctor how often you should get this shot, and whether your adult family members should also get the shot.
Do not receive any vaccines (other than tetanus or flu shot) without first talking to your doctor. Do not receive any live virus vaccines or be in contact with people who recently received one. A live virus vaccine may trigger an infection in someone who is taking immunosuppressant medications.
Make sure you receive the 3-shot Hepatitis B series.
- Be sure your environment is as safe as possible:
Do not go into crowded places for the first three months after your transplant. If you cannot control how far away you can stay from other people, it is probably a crowd. Do not work in or visit any form of construction site.
Keep your house clean and free of excess dust. Dust can be harmful to you after your transplant. If you absolutely must go near this type of area, wear a mask provided by the Transplant Team. You may have pets, but have other family members or friends clean the litter box, cage or yard. In addition, do not add any new pets to your home, especially birds.
If you enjoy fishing, use caution with fish hooks, fish fins, and fillet knives. Protective gloves should be worn when handling these items. Also avoid gardening for the first six months after your transplant. Wear garden gloves when gardening. Soil has many molds and fungi that can be sources of infection. Do not mow the lawn yourself and avoid areas where people are mowing. A lawn mower blows bacteria from the grass which can cause an infection.
Stay away from hot tubs, whirlpools, saunas or steam baths. Germs tend to multiply in these.
Be sure to ask your Transplant Team when you can safely return to work or school.
Preventive Care Recommendations
Adult Females:
Screening For Breast Cancer
Starting at Age
- Starting at age 40*
- *If your grandmother, mother or sister have had breast cancer, you may want to begin screening at age 35 or as recommended by your doctor.
Preventive Care
- Breast physical examination and screening mammography.
How Often?
- Breast physical exam every year by a health care provider.
- For women after transplant: breast physical exam and screening mammography should be performed once a year.
Screening For Cervical Cancer
Starting at Age
- Starting at age 18
Preventive Care
- Pap smear and pelvic examination.
How Often?
- Every year for three years starting at age 18, then every three years if all three Pap smears were normal and NPV negative and if you do not have any of these risk factors:
- HIV-positive
- Cigarette smoker
- Multiple sex partners
- Prior abnormal Pap smear or cervical dysplasia
- If any of these risk factors apply, then have a Pap smear and pelvic exam every year.
- For women after transplant: Pap smear and pelvic examination should be performed every year, regardless of age.
Screening For Cholesterol
Starting at Age
- 40
Preventive Care
- Total cholesterol.
- HDL every five years.
How Often?
- If you have a personal or family history of cardiovascular disease, you may require more frequent screening and at an earlier age.
- After transplant: Cholesterol should be checked at least once a year.
Screening For Colorectal Cancer
Starting at Age
- 45
Preventive Care
- Stool testing for blood plus sigmoidoscopy or colonoscopy.
How Often?
- Stool testing every year.
- Sigmoidoscopy every five years.
- Colonoscopy every 10 years.
- If you have a parent, brother or sister who have had colorectal cancer, you should have a colonoscopy every five years, starting at age 40.
Adult Males:
Screening For Cholesterol
Starting at Age 30
Preventive Care
- Total cholesterol triglycerides, HDL and LDL.
How Often?
- Once per year.
- If you have a personal or family history of cardiovascular disease, you may require more frequent screening and at an earlier age.
- After transplant: Cholesterol should be checked at least once a year.
Screening For Colorectal Cancer
Starting at Age
- 50
Preventive Care
- Stool testing for blood plus sigmoidoscopy or colonoscopy.
How Often?
- Stool testing every year.
- Sigmoidoscopy every five years.
- Colonoscopy every 10 years.
- If you have a parent, brother or sister who have had colorectal cancer, you should have a colonoscopy every five years, starting at age 40.
Screening For Prostate Cancer
Starting at Age 50
Preventive Care
- Digital rectal exam and PSA Testing.
How Often?
- Digital rectal exam every year.
- PSA testing every year.
Dental Care
Why is good dental care important?
In some patients, cyclosporine (Neoral) can cause gums to swell, become tender, and sensitive to heat and cold. Poor diet can also cause gum disease. Sore, bleeding gums can easily become infected. Good dental care may help prevent infection.
Here are some general guidelines:
- Examine your mouth and gums every day. If you have red or swollen gums, contact your transplant coordinator.
- Brush your teeth and gums thoroughly after each meal with a small, soft toothbrush and fluoride toothpaste. Use foam sticks instead of a toothbrush if your gums are especially sore.
- Use dental floss every day.
- Your doctor may tell you to use an antibacterial mouthwash rinse. Avoid commercial mouthwashes or throat lozenges that contain a high concentration of alcohol - they may irritate or dry your mouth.
- Keep dentures clean and fitting properly.
- Prepare a gargle by dissolving one teaspoon each of salt and baking soda in a quart of warm water. (A smaller portion of this can be made by stirring 1/4 teaspoon each of salt and baking soda into eight ounces of warm water.) Rinse your mouth and gargle with this solution at least four to six times a day, especially after meals and before going to bed.
- Have your teeth cleaned and checked by a dentist at least every six months. Tell your dentist that you have had a transplant before your appointment so he or she can take precautions to prevent possible infection. Also be sure to call your transplant coordinator for an antibiotic prescription at least one week before any of your dental appointments.
- If a mouth sore develops, eat foods that are warm or at room temperature and avoid eating acidic foods and beverages (such as tomatoes and oranges).
Skin Care
A dermatology assessment will be done pre-transplant and annually post-transplant.
Follow these guidelines for skin care:
Taking Care of Cuts or Wounds
- Keep minor cuts and wounds clean. Wash them with soap and water or hydrogen peroxide, dry your skin and cover the cut with a sterile bandage.
- Go to the emergency room near your home if you have a deep cut, or one that bleeds a lot. Be sure to tell the health care providers that you are a transplant patient.
- Call your doctor if your wounds become red and drain anything but clear liquid.
- Have a tetanus shot every 10 years.
Daily Hygiene
- Frequently wash your hands with soap and warm water, especially before preparing food, and after using the bathroom or after touching soiled linens or clothes. Lather well, rubbing your hands back and forth together, to clean all surfaces, including the nail beds and webbing between your fingers.
- Shower or bathe daily using a mild soap. Special soap is not needed at home.
- If you have dry skin, apply a mild skin lotion after bathing.
Acne
Prednisone and cyclosporine, two medications that you must take, can cause acne. To lessen skin problems:
- Keep your skin as clean and oil free as possible.
- Use a washcloth and mild soap.
- Avoid soaps that contain pumice or coconut oil.
- Some over-the-counter acne products may be helpful.
- Use non-comedogenic skin care products and cosmetics.
- Make an appointment with a dermatologist (skin doctor) if acne becomes a problem.
Sun Protection
Overexposure to the sun can cause dry skin, sunburn, blisters and increase the risk of skin cancer. Some of your medications may make you more sensitive to the sun's rays.
To avoid overexposure:
- Always wear a sunblock lotion, sun protective factor (SPF) of 15 or greater when outdoors in bright sunlight.
- Wear a broad-brimmed hat and protective clothing such as light pants instead of shorts, long-sleeved shirt, and socks to protect your feet and lower legs.
- When swimming, wear a T-shirt over your bathing suit.
- Check your skin for new markings; especially new irregular shaped, raised, red, black or brown markings. If you notice any new skin markings, see a skin doctor (dermatologist) for prompt evaluation and treatment.
Immunizations
Get a flu shot every fall. You cannot get the flu by getting the immunization. Encourage your adult family members to get flu shots also. You can arrange to get the flu shot from your doctor or Transplant Team.
Ask your doctor if you should get a pneumovax (pneumonia) vaccine. Ask your doctor how often you should get this shot, and whether your adult family members should also get the shot.
Do not receive any vaccines (other than tetanus or flu shot) without first talking to your doctor. Do not receive any live virus vaccines or be in contact with people who recently received one. A live virus vaccine may trigger an infection in someone who is taking immunosuppressant medications.
Make sure you receive the 3-shot Hepatitis B series and two shots Hepatitis A series (if you tested negative).
Living a Full Life Again
During the months of illness before heart transplant surgery, you and your family made many adjustments. The purpose of having heart transplant surgery was to make you feel better and to live a full life again. Let's review some areas of life often affected by your transplant.
- Return to Work
- Finances
- Family Adjustment
- Dealing with Emotions
- Sexual Activity
Daily Activity and Exercise Guidelines
Caring for your personal hygiene
By the time you leave the hospital after your heart transplantation, you should take care of all your personal hygiene, (bathing, shaving, dressing). Continue to perform these activities at home.
Light chores
It takes about six weeks for your sternum (breastbone) to heal after heart transplantation. During this time, you may do light household chores such as laundry, shopping, cooking, and washing dishes. But, do not lift objects that weigh more than 10 pounds. These include suitcases, grocery bags, full laundry baskets, pets or children.
Also avoid activities that require pushing or pulling heavy objects, such as shoveling snow or mowing the lawn. Your doctor will tell you when you can resume these activities during your heart transplantation follow-ups.
Driving after your heart transplantation
You may not drive for at least six weeks. However, you may be a passenger as often as you like. For the first two weeks after your heart transplantation, you may want to stick close to home to avoid infections or becoming overtired. Over time, increase your outings and begin to get back to activities you enjoy after your heart transplantation. Your doctor will tell you when you can begin driving a car.
Pace yourself
Spread your activities throughout the day. Schedule the most important ones early. Reschedule unfinished activities for another time. You may climb stairs, but you may need to slow your pace or rest midway if you become tired.
Get a good night's sleep
Many people complain of trouble sleeping for a time after any heart transplantation surgery. This can be due to the affects of anesthesia, discomfort related to healing, changes in your daily routine, or concerns you may have. Without enough rest, you may feel overtired and irritable. If you cannot sleep, try these tips:
- If you have pain, take your pain medication about a half hour before bedtime. Arrange pillows to help keep you in a comfortable position.
- Avoid napping too much during the day. But keep in mind that during your recovery it is important to balance activity with rest.
- If you are nervous or anxious, talk to your spouse or partner. Get things off your mind.
Begin a Lifelong Exercise Program After Your Heart Transplantation
Regular exercise is a vital part of your new lifestyle. The transplanted heart is only 70 percent as efficient as a normal heart. So, you must exercise regularly to maintain physical fitness.
Exercise will help you:
- Develop more stamina
- Maintain your ideal weight by burning calories
- Keep your muscles and bones strong and healthy
- Lower your blood pressure, cholesterol, blood sugar levels
- Manage stress and give you a sense of well-being
Exercise after your transplant
Your doctor or cardiac exercise specialist will give you a home program based on your needs, current abilities and the new response patterns of your heart. Follow these guidelines when you return home.
To be safe, follow these exercise tips:
- Know the type and level of exercise that is right for you.
- Exercise three to six times per week.
- Set up a regular exercise schedule. This should be separate from your normal activities of daily living.
- Exercise should be aerobic. Aerobic exercise involves large muscle groups and includes repetitive movement. Such activities include walking, cycling or swimming.
- Exercise should include at least five minutes of warm-up and cool-down.
- Work up to an exercise program that includes 40-60 minutes of activity, three to six days each week, at your appropriate intensity level.
- Exercise at a "moderate" intensity. An appropriate amount of activity should not exhaust you.
- Focus on increasing your distance or time - not speed.
- Wear comfortable clothes and shoes.
- Avoid exercising in temperatures below 30 degrees and above 80 degrees Fahrenheit.
Be alert for signs of exercising too hard. These include:
- Excessive shortness of breath
- Dizziness
- Chest discomfort
- Exhaustion
If these symptoms occur, stop the activity and rest. Call your doctor if these symptoms last longer than 20 minutes or if they occur on a regular basis.
Cardiac Rehab
In the hospital after your transplant, an exercise specialist provided basic guidelines on your exercise program. This is commonly referred to as Phase I Cardiac Rehabilitation. Upon discharge, it is important to continue with your exercise program.
A Phase II cardiac rehab program can help you learn about your transplant, lifestyle changes and assist you in maintaining your exercise program.
Phase II cardiac rehab is offered at Cleveland Clinic, or you can be referred to a program closer to your home.
For more information on Cardiac Rehabilitation, contact the Preventive Cardiology and Rehabilitation Program at 216.444.9353.
Return to Work
Before your heart transplant, you may have been on disability. With your new heart, your disability may be stopped. Most transplant patients are physically able to return to work. Studies have shown that people who return to work feel better about themselves and do better physically, as well.
Depending upon the type of work or your company's sick leave policy, you may or may not be able to return to your former job. However, we do not expect you to remain inactive.
If you are out of work, it is important to explore other job options for the future. You should look for ways to re-enter the job market. This may involve job retraining.
Vocational Rehabilitation Services (VRS) is available to provide you with many types of assistance to return to employment. This help can take the form of counseling, training, and job placement. VRS can provide training through technical schools, junior colleges, and colleges. A referral for these services can be made by your Social Worker.
Sometimes, after transplant, there are barriers to return to work. Some employers are hesitant to hire transplant patients. The "Americans With Disabilities Act" provides some protection from this discrimination.
This, together with education, can help employers begin to feel confident that transplant patients can be good, reliable employees. Patients who can maintain an employee status with their employers (whether active or on leave) during the wait for transplant seem to have an easier time returning to work after transplant.
Staying active is very important. If you are retired, volunteer for a local school, hospital, or charitable organization. This will allow you to remain physically and mentally active.
Finances
Finances may play a big part in your recovery and the outlook for the future. If you have concerns about your finances related to insurance, disability, medications or employment, please discuss this with your social worker. There are many resources available to help you. Please call 216.445.7119 with any financial questions.
Family Adjustment
This may be a stressful time for your whole family. Roles may have changed during the pre-transplant period. Spouses, children, and other relatives may have taken over daily responsibilities. Now, it is time to re-establish your family roles and relationships.
Families feel better and cope better when they discuss each member's feelings about the transplant and plans for the future.
Young children may be overlooked in this process - whether they are your children or your grandchildren. It is important to discuss their feelings and fears as well. The transplant team social worker is available to help children and families adjust to illness and health.
Dealing with Emotions
After the excitement of the heart transplant, some people have feelings of a "let down." You or your family may notice mood changes or times of feeling "down" or "blue."
Other patients may become irritable. They may have quick bouts of anger or "fly off the handle" at little things. This may be related to high expectations after the transplant and attempting to live up to them. It may also be related to normal healing or medications (steroids). These are normal emotional responses that will diminish with time.
Remember, you need medications. Therefore, you must anticipate some side effects. As your doses are safely decreased, mood changes will lessen.
It may also help to share your feelings with your spouse, a friend, or clergyman. Open discussion of feelings will help you and your family understand how you feel. Support groups are available for patients who have had transplants.
If you still don't feel quite right after the early stages of recovering, and you feel your emotional changes are interfering with your ability to enjoy life, tell a member of the transplant team. Supportive counseling may be helpful.
For more information:
Sexual Activity
Many patients and their partners feel nervous about resuming sexual activity after surgery. The amount of energy it requires to perform intercourse with a spouse or regular partner is similar to climbing about one or two flights of stairs or walking about one half mile (0.8 km) at a brisk pace.
If you cannot perform these activities without getting angina, or shortness of breath, or becoming overtired, please allow additional recovery time before resuming sexual activity. For the first six to eight weeks, you may need to use a low stress position to limit pressure or weight on the breast bone. Keep in mind that a sexual relationship has both physical and emotional aspects.
- Talk openly with your partner.
- Have sex when you are rested and physically comfortable.
- Create realistic performance expectations - it may take time to return to an active sex life.
- Relax and focus on lovemaking not on your new heart or any past failures.
- Be caring, honest and loving with each other.
Anxiety for either partner as well as some medications may interfere with sexual arousal and performance. Discuss any concerns with your doctor.
Soon, you and your partner will return to a satisfying emotional and physical relationship.
Birth Control
- Women must use some form of birth control after transplant.
- Let us know if you need to see a doctor for birth control.
- Women who wish to become pregnant should discuss this with their doctor.
Substances to Avoid
As a heart transplant patient, you have agreed to avoid tobacco and illicit drugs and to limit alcohol. All of these substances can be harmful. There are several reasons for limiting alcohol:
- Alcohol is an appetite stimulant.
- Most alcoholic beverages contain no vitamins or minerals, but plenty of calories.
- Increased alcohol consumption can cause blood triglyceride levels to rise, increasing the risk of coronary artery disease.
- Cyclosporine levels may be affected by alcohol.
Limit your daily alcohol intake to one 6-ounce glass of table wine, or one 12-ounce beer, or 1.5 ounces of distilled liquor (gin, rum, vodka, whiskey) per day.
If you need help in avoiding these substances, please contact your doctor, nurse, or social worker.
Complications
Heart Transplant surgery is a major operation and therefore may involve complications. Below is a list of possible complications after surgery. Our goal is to minimize your risk, but always educate you on what might occur.
Hypertension (HTN)
Cause
- Cyclosporine
- Prednisone
- Previous hypertension
Prevention/Action
- Monitor blood pressure
- Exercise regularly
- Follow a low-salt diet
- Take anti-hypertensive medications
- Avoid weight gain
- Follow-up with your doctor regularly
Acute Rejection
Cause
- Natural immune system
- Stopping medications
Prevention/Action
- Biopsy
- X-ray
- Heart function analysis
- Report rejection symptoms
- Take immunosuppressants
- Follow-up with your doctor regularly
Infection (there's always an increased risk for infection after transplant)
Cause
- Immunosuppressants
Prevention/Action
- Avoid people who have a cold, flu or other illness
- Follow good personal hygiene
- Frequently wash hands
Kidney Dysfunction
Cause
- Cyclosporine
- Other medications
- Heart failure
- Hypertension
Prevention/Action
- Monitor creatinine
- Monitor cyclosporine levels
- Monitor blood pressure
- Take anti-hypertensive medications
- Follow-up with your doctor regularly
Bone Marrow Suppression
Cause
- Immunosuppressants
Prevention/Action
- Monitor white blood cell count
- Follow up regularly with your doctor
Increased risk of cancer—especially skin and lip cancer
Cause
- Immunosuppressants
- Sun exposure
- Smoking
Prevention/Action
- Reduce sun exposure and wear protective clothing, use sunscreen
- Don't smoke!
- Follow-up with your doctor regularly
Bone Loss/Weakness
Cause
- Steroids
Prevention/Action
- Follow-up with your doctor regularly
- Female patients: ask your doctor about taking estrogen supplements
- Exercise regularly
Impotence
Cause
- Hypertension
- Pre-transplant condition
- Medications
Prevention/Action
- Monitor your blood pressure as recommended
- Take anti-hypertensive medications as prescribed
- Ask your doctor for a urological evaluation
- Follow-up with your doctor regularly
Liver Disease
Cause
- Cyclosporine
Prevention/Action
- Keep all scheduled lab appointments so your response to the medication can be evaluated
- Follow-up with your doctor regularly
- Ask your doctor how often you should get an abdominal ultrasound
High Potassium Level
Cause
- Immunosuppressant medications
Prevention/Action
- Keep all scheduled lab appointments so your response to these medications can be evaluated
- Eat low-potassium foods, as recommended
Coronary Artery Disease - due to chronic rejection or developing naturally over time
Cause
- Immune system changes
- Lipids
- Hypertension
- Obesity
Prevention/Action
- Take immunosuppressant medications and vasodilator medications as prescribed
- Follow a heart-healthy diet
- Monitor your cholesterol levels with annual blood tests (or more frequently, as recommended)
- Ask your doctor how often you need a cardiac catheterization
- Follow-up with your doctor regularly
Biopsy Complications (scar tissue in the neck and heart)
- Frequent biopsies
Prevention/Action
- Follow-up with your doctor regularly for early detection and treatment of this complication
High Blood Pressure
Hypertension after transplant can be caused by many factors, such as your medications, changes in the function of your kidneys, or too much sodium (salt) in your diet.
At home, you will be asked to check and record your daily blood pressure, heart rate and weight.
We strongly encourage you to purchase an automatic blood pressure monitor which can provide an accurate assessment of your heart rate and guidelines:
- Eat a diet low in sodium (salt) and fat. (See also Hypertension and the Dash Diet) Ask your doctor if you also should limit your daily potassium level.
- Maintain your ideal body weight. (See also Prevention: Weight Management).
- Do not smoke. (See also Prevention: Smoking).
- Follow a regular exercise program. (See also Prevention: Exercise).
Follow your doctor's guidelines about alcohol use. In general, you should limit your daily alcohol consumption to no more than two drinks per day for men and one drink per day for women and lower-weight individuals. One drink equals:
- 1.5 ounces of 80 proof liquor (example: whiskey, vodka, or gin) OR
- 5 ounces of wine OR
- 12 ounces of beer or wine cooler
Take your blood pressure medications as prescribed.
Bring your blood pressure records to each visit and report high blood pressure readings in-between visits.
Malignancies
Transplant patients have an increased risk of developing malignant tumors and cancers. Because transplant patients need to take immunosuppressant medications, malignant cells may escape detection and destruction by the immune system and develop into a tumor.
Tumors that are common in the general population, such as breast cancer, lung cancer, and colon cancer, do not seem to occur more frequently in transplant patients. Skin cancers are the most common tumor in transplant patients. Sun exposure is the major risk factor for skin cancer.
Lymphomas occur with increased frequency in transplant patients.
Signs and symptoms may include:
- Enlarged lymph nodes or swelling beneath the skin
- Fever, excessive fatigue, weight loss, poor appetite and sweating
- Nodules, which can be detected on routine chest x-rays
If you have any of these signs or symptoms, please contact your doctor for prompt evaluation. Lymphomas are diagnosed by biopsy of a lymph node or nodule. Other tests may be performed to determine if other organs are involved.
Check your neck, armpits, and groin area for lumps or new growths. Report signs of these to your doctor.
Treatment consists of a change in the immunosuppressant medication dosage and/or schedule, and sometimes chemotherapy or radiation therapy.
Rejection
Body's Immune System
The immune system is the body's defense against foreign invaders. Made up of mostly white blood cells, its job is to destroy germs such as bacteria and viruses, and help to fight other diseases.
Your white blood cells are made up of different teams of fighter cells, called B and T cells. B cells fight germs by producing antibodies. Antibodies are strong weapons against infections, causing germs to become harmless.
T cells kill foreign invaders, such as germs and cancer cells. Each time your body has an immune reaction, it memorizes the foreign body (antigen) and how it was stopped so that it can respond quickly the next time that same antigen is introduced.
The immune system is very helpful and powerful, but it cannot tell the difference between "bad invaders," such as germs, and "good invaders," such as a transplanted heart. As a normal response, your body's immune system sees the new heart as a foreign invader and attempts to destroy it. Immunosuppressant medications are given to stop this process.
If the immune system is able to attack the transplanted heart, it is called rejection. Rejection must be detected and treated quickly to prevent damage to the transplanted heart.
Rejection may seem frightening to some transplant patients, but deaths from rejection are uncommon. Most cases of rejection are detected by biopsy and tissue staining and occur without any symptoms.
Types of Rejection
Rejection can be hyperacute, acute or chronic.
Hyperacute Rejection
Hyperacute reactions occur if you have been exposed to the same or similar antigens found in the donor heart. Previous exposure to these antigens may have occurred through blood transfusion, pregnancy or prior transplants. Hyperacute rejection occurs rarely, because transplant recipients undergo testing to determine if they have pre-formed antibodies which increase the risk for this problem. However, when it does occur, the body's immune system reacts swiftly and strongly, sometimes causing failure to the new organ within the first few hours after transplant.
The PRA (panel of reactive antibodies) test is performed by taking a sample of the recipient's blood and mixing it with samples of blood from multiple donors in the community. Blood from many volunteers is obtained because together they represent most of the human antigens to which a potential recipient may have been exposed.
A cross-match test is done when a local potential donor is found. The organ procurement agency will send a sample of the donor's blood to be combined with a stored sample of the recipient's blood. If the recipient's blood cells destroy donor cells, it means that pre-formed antibodies have reacted with donor antigens. The cross-match is termed "positive" and indicates that a heart transplant with this donor may be risky. Usually the procedure is canceled because of the high likelihood of hyperacute rejection.
Recipients with pre-formed antibodies (high PRA) may have a longer waiting time because of the need to match with an appropriate donor. It is important to note the PRA can change with time or exposure to blood, and occasional retesting may be necessary.
Acute Rejection
There are two forms of acute rejection: cellular and vascular.
Acute cellular rejection: This type of rejection occurs after the recipient's white blood cells realize that the transplanted organ is foreign and mount a defense against it. Immunosuppressants block the immune response. Without these medications, transplanted organs would probably fail within two to four weeks as a result of acute cellular rejection.
The chances of acute cellular rejection are greatest during the first six months after transplant. Most people have one or more episodes of acute rejection during that time. The chance of acute cellular rejection decreases with time and remains very low after the first year because of immunosuppressive medications and tolerance to the transplanted organ.
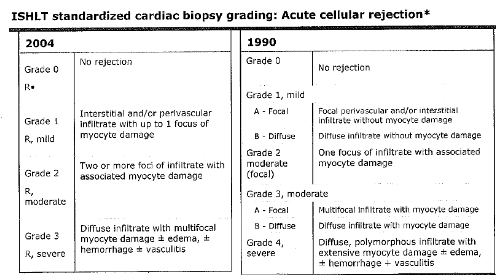
Source: International Society of Heart and Lung Transplantation:
"Classification of Acute Rejection"
Note: Acute vascular rejection has a different grading system.
Acute vascular rejection: Acute vascular rejection is a type of acute rejection that occurs early after transplant (within the first four months) in a small number of patients. Vascular rejection causes damage to the innermost layer of the coronary arteries. This leads to scarring and a decrease in blood flow, potentially leading to other heart complications. It is also believed that patients with vascular rejection are more prone to developing post-transplant coronary artery disease.
Vascular rejection has been dramatically reduced with the change to triple therapy drug treatment. Findings of vascular rejection are now rare.
Symptoms of Rejection
It is important to know the signs and symptoms of rejection. In most cases, rejection does not cause any signs or symptoms. In more advanced stages, you may feel:
- Shortness of breath
- Irregular pulse
- Swelling of the feet, legs and hands
- Fatigue (feeling overtired)
- Unexplained weight gain over one to three days
- Low blood pressure
- Low grade fever
Most patients do not have symptoms. If symptoms occur, please call your transplant coordinator or cardiologist right away.
Nutrition Guidelines
The foods you eat can help you heal and resist infection after organ transplantation. Other foods may need to be avoided. Here are some general guidelines for nutrition following organ transplantation:
- Eat a healthy, well-balanced diet. Eat foods from all the food groups.
- Drink plenty of fluids (unless you are told to restrict your fluids). Water is the best.
- Wash fresh fruits and vegetables thoroughly before eating.
- Do not eat raw seafood (fish or shellfish).
- Make sure eggs, chicken or pork are fully cooked and well-done.
- Following a Proper Diet After Your Organ Transplantation.
Keeping a healthy diet is one of your most important jobs after your organ transplantation. Your diet plays an important role in helping you heal, avoiding weight gain, and maintaining your health into the future.
The four key areas you need to focus on for your diet following organ transplantation include:
- Follow a low-sodium diet.
- Eat foods low in fat and cholesterol.
- Control your weight by balancing your meals with exercise.
- Include a variety of healthy foods in your diet.
1. Follow a low-sodium (salt) diet.
Sodium causes your body to hold in (retain) fluids. A diet high in sodium can lead to high blood pressure. Prednisone, a medication often prescribed after heart transplant, causes you to retain sodium and fluids. So if you are taking this drug, controlling sodium in your diet is even more important. Your doctor will tell you how much sodium you should have in one day - usually 2000 mg is the upper limit. Sodium is found in table salt and many of the foods we eat, most commonly, preserved foods, canned foods, luncheon meats, cheeses and snacks.
Here are some tips to limit sodium in your diet following your organ transplantation:
- Avoid the salt shaker and seasoning salts. Use herbs and spices instead.
- Read food labels. Find out how much sodium is in the foods you eat. Choose foods with labels that state "low salt" or "low-sodium."
- Eat less canned and processed foods (canned and frozen foods, cheeses, and luncheon meats). Natural is better.
- Stay away from "fast" foods.
- When dining out, ask if MSG (a food additive) is in the food before you order. If it is, select another menu item or ask that the meal be prepared without MSG.
- Read stomach, cold, and headache medication labels for sodium content.
- Choose no-salt snacks and crackers.
- Avoid smoked, cured, salted, processed or canned meat, poultry or fish.
- Check with your doctor before using a salt substitute.
- Remember, to improve the effectiveness of your diuretic ("water pill") take it along with following a low-sodium diet.
2. Eat foods low in fat and cholesterol.
A high-fat diet will lead to high blood cholesterol, which is a major risk factor for coronary artery disease. This disease can reduce blood flow to the heart and damage your new heart. Because cyclosporine tends to raise blood cholesterol levels and prednisone tends to cause weight gain, you may have an increased risk of developing coronary artery disease after heart transplant. The best way to decrease this risk is to decrease the amount of fat in your diet.
Here are some tips for a low-fat and low-cholesterol diet:
- Limit red meat to two times per week and try to have one "vegetarian day" each week.
- Eat no more than 6 ounces of meat, fish or poultry (chicken and turkey) per day (3 ounces is about the size of a deck of cards).
- Remove visible fat or skin before cooking.
- Steam, boil, broil, grill, microwave or bake instead of frying.
- Choose non-fat (skim) milk dairy products.
- Cut back on added butter and margarine, salad dressing, gravy and sauces.
- When dining out, ask how food is prepared and make healthy choices.
- Choose healthy low-fat snacks.
3. Control your weight by balancing your meals with exercise.
Weight gain is very common after transplant, as one side effect of your medications is an increased appetite. If you are overweight, your heart must work harder to pump blood and it can lead to increased cholesterol, triglycerides, blood sugar, and blood pressure.
So, it is important to achieve and maintain an optimal weight. Here are some guidelines:
- Eat low-fat foods.
- Watch out for fat-free foods that often replace fat with high-calorie sugars.
- Control your portion sizes. Read labels to find out fat content, calories and portion sizes.
- Eat smaller, more frequent meals so you can feel full without increasing calories.
- Limit your intake of sweets and sugars, such as table sugar, brown sugar, corn syrup, honey, regular sodas, rich desserts, and candy. Instead, use fresh fruit as dessert on a daily basis and save heavy desserts for special occasions.
- Exercise five to six times per week.
- Choose healthy low-calorie snacks.
- Set realistic goals—weight loss should be gradual, no more than one to two pounds per week.
4. Include a variety of healthy foods in your diet.
A healthy, balanced diet will help you maintain your weight, control your blood pressure, cholesterol and blood sugar and help you feel better.
Include a variety of foods in your diet. Try to eat foods from each food group.
Eat foods high in fiber. Fresh fruits and vegetables, legumes (beans), and grains contain many vitamins, lower blood cholesterol and may also protect against cancer and heart disease.
To protect against high blood pressure, eat foods rich in potassium, calcium, and magnesium. Certain diuretics contribute to loss of potassium and magnesium, so if you are taking these drugs, this is even more important to include: fresh fruits (especially bananas and strawberries), dried fruits, skim milk, and fresh vegetables. Some medical conditions (such as kidney disease) and medications (potassium-sparing diuretics), may require you to LIMIT the amount of potassium in your diet.
Talk with your doctor about including potassium-rich foods in your diet.
Infection-When to Call the Doctor
It is up to you to recognize the symptoms of infection and get treatment as soon as any of these symptoms occur.
Note: Prednisone can mask the usual signs of infection so make sure you get treatment promptly. Don't wait!
Call your healthcare provider right away if you notice any of these symptoms:
- Fever over 101 degrees F (38.4 degrees C)
- Record your temperature once a day to help you quickly detect a fever
- Sweats or chills
- Feeling "lousy" or flu-like symptoms (chills, aches, headaches or feeling a decrease in your energy level without any obvious cause)
- Skin rash
- Pain, tenderness, redness or swelling
- Wound or cut that will not heal
- Red, warm or draining sore
- Sore throat, scratchy throat or pain when swallowing
- Sinus drainage, nasal congestion, headaches or tenderness along upper cheekbones
- Persistent dry or moist cough that lasts more than two days
- White patches in your mouth or on your tongue
- Nausea, vomiting or diarrhea
- Trouble urinating: pain or burning, constant urge or frequent urination
- Bloody, cloudy or foul-smelling urine
Life Post-Transplant
After you leave the transplant center, our goal is to help you adjust and live a healthy life. At the transplant center, we will help you address the following issues:
- Nutrition Guidelines
- Activity and Exercise Guidelines
- Cardiac Rehab
- Substances to Avoid
Living a Healthy Lifestyle
Follow-Up Appointments
- When to Call the Doctor in Between Appointments
Preventive Care Recommendations
- Dental Care
- Skin Care
- Immunizations
Living a Full Life Again
- Return to Work
- Finances
- Family Adjustment
- Dealing with Emotions
- Sexual Activity
Follow-Up Appointments
Lifelong follow-up appointments with your doctor are very important after heart transplant. Some of your heart transplant medications can affect your body in different ways. Your doctor will monitor your body's responses after heart transplant and will adjust your medications as needed.
Visits with your cardiologist after your heart transplant
When you first leave the hospital after heart transplant, you will need to visit your cardiologist often (about once a week). You will need to stay in the Cleveland area with a family member or friend for the first month after your heart transplant. Later, your visits will be less frequent.
If you need to arrange housing after your heart transplant, discuss this with your social worker or housing specialist.
It is important to bring all your medications and your daily log to the doctor at each visit following your heart transplant. The following information should be recorded in your log:
- Names of medications, dose, and time you take them
- Daily weight
- Daily temperature
- Daily heart rate (pulse)
- Daily blood pressure
- Comments, events, or questions you want to ask
This information helps your doctor adjust your medications and care to make your heart transplant recovery as effective as possible.
Your appointments with your cardiologist may include:
- Blood tests
- An electrocardiogram (ECG or EKG)
- A chest x-ray
- A heart biopsy
- A visit with your doctor and transplant coordinator
To detect the development of coronary artery disease (chronic rejection), your doctor will check your heart's arteries and overall function several weeks after your transplant. Two tests will be performed: a cardiac catheterization and intravascular ultrasound.
These tests will be repeated once a year.
Keeping in contact with your transplant coordinator
You may need additional appointments with other specialists or doctors on the day of your appointment with your cardiologist. The post-transplant coordinator will schedule these visits. If you would like to make an appointment that has not been scheduled, please discuss this with your transplant doctor or transplant coordinator.
Notify your transplant coordinator if you have been prescribed any new medications by any other doctors.
Follow-up with other doctors
Prevention and early detection is best. Some of the problems we may be looking for after transplant include hypertension, coronary artery disease, anemia, low white blood cell counts, skin cancers or other types of malignancy. It is important to see the following doctors for regular exams or as they are needed:
Ophthalmologist
You should see an ophthalmologist for annual eye exams including glaucoma and cataract evaluations. Eye doctor appointments are important, since prednisone can cause vision changes.
Gynecologist
Female patients should visit a gynecologist yearly for a pelvic examination and PAP smear, regardless of age. Mammograms should be performed regularly, as recommended by your doctor.
Internal Medicine or Family Medicine Doctor
Male patients over age 50 years should have an annual PSA (prostate specific antigen) blood test.
Dentist
Regular follow-up appointments with your dentist are important. Your gums may become swollen and bleed easily. Tell your dentist about your transplant so antibiotics can be prescribed for any dental procedure.
Dermatologist
Wear sunscreen, protective clothing and a hat when outdoors because of an increased risk of skin cancer. If you notice any unusual skin growths, darkened spots or bumps, see a dermatologist as soon as possible. You may also want to consult a dermatologist if acne is a problem for you after transplant.
Preventive Cardiology Specialist
It is very important to control your risk factors for heart disease. If you have risk factors, such as high blood cholesterol, diabetes, hypertension, being overweight, smoking or high stress or anger, a preventive cardiology specialist can help you reach optimal control.
When to Call the Doctor in Between Appointments
Sometimes you need to see your doctor before your next heart transplant follow-up. In between follow-up visits, call your heart transplant doctor or heart transplant nurse if you have:
- Nausea, vomiting, or diarrhea
- Blood in the urine or stool
- Sustained high blood pressure
- Lightheadedness or dizziness
- Frequent headaches
- Swelling in the ankles or feet
- Sudden weight gain
- Signs of infection
- Signs of rejection