Overview
Approximately 5.7 million people in the U.S. have heart failure, leading to more than 300,000 deaths annually and one of the most common reasons for hospitalizations. The condition is characterized by the heart’s inability to pump enough blood to meet the body’s needs.
Choosing Your Care
If you suffer from heart failure, experts from Cleveland Clinic Florida’s Heart, Vascular & Thoracic Institute can help. The Section of Heart Failure within the Heart, Vascular & Thoracic Institute is where heart failure patients receive care. The primary goal of treating patients with heart failure is to decrease the likelihood of disease progression, thereby decreasing the need for a heart transplant, advanced heart failure treatments, the need for hospitalization and the risk of death. It is also to lessen symptoms and improve quality of life. However, for a small percentage of patients, heart failure is relentless, and Cleveland Clinic Florida has a multidisciplinary team of caregivers from South Florida to the Treasure Coast specializing in heart failure to provide the best options for advanced treatment therapies.
USING THIS GUIDE
Please use this guide as a resource as you learn about treatment options for heart failure and advanced heart failure. As a patient, you have the right to ask questions and to seek a second opinion.
What is advanced heart failure?
Often called congestive heart failure, but more commonly heart failure, it means your heart muscle is not functioning as well as it should. Most heart failure patients develop this chronic disease as a result of hypertension, diabetes, cardiomyopathy, coronary artery disease, valvular heart disease, metabolic syndrome or a history of alcohol or drug abuse.
Advanced heart failure can be the final stage of a long-standing illness. Patients may gradually decline over years of treatment and develop symptoms at rest, very poor quality of life, and have escalating symptoms despite the best medical care. Other patients may be perfectly healthy and suddenly develop severe or acute heart failure after a heart attack or viral infection that attacks the heart muscle. Other conditions can also cause rapid, severe heart failure.
The American Heart Association and American College of Cardiology developed the four Stages of Heart Failure, referring to them as Stage A (at risk to develop heart failure) through Stage D (the most severe). When a patient progresses to Stage D, this is considered advanced heart failure.
In addition, there are two kinds of heart failure. If the left ventricle (lower left chamber of the heart) is not contracting with enough force, it is called systolic heart failure — or heart failure with reduced ejection fraction (EF). If the ventricles are stiff and do not relax and fill properly, it is called diastolic heart failure — or heart failure with preserved EF. Ejection fraction is the measurement of blood that is pumped out of your heart with each heartbeat.
Symptoms

What are the symptoms of heart failure?
You may not have any symptoms of heart failure, or the symptoms may be mild to severe. Symptoms can be constant, or can come and go. Symptoms are due to the changes that occur in your heart and body and include:
- Shortness of breath or difficulty breathing with exercise, at rest, or when lying flat in bed. Shortness of breath occurs when fluid backs up into the lungs (congestion), or when your body does not have enough oxygen-rich blood to let you go on with your activity or exercise without a rest period. Even though you think of breathing as a lung problem, your heart condition can cause periods of shortness of breath. In some cases, symptoms may cause you to wake up suddenly at night, disrupting your normal sleep patterns.
- A dry, hacking cough or wheezing
- Swollen ankles, legs and abdomen, and weight gain. Less blood to the kidneys causes you to retain fluid and water, resulting in edema (swelling) and water weight gain.
- The need to urinate while resting at night. Gravity causes more blood to get to the heart and kidneys when you are lying down.
- Tiredness (fatigue) and weakness during exercise or activities occur because the heart is not pumping enough oxygen-rich blood to major organs and muscles.
- Dizziness, confusion, difficulty concentrating or fainting may occur because the heart is not pumping enough oxygen-rich blood to the brain.
- Rapid or irregular heartbeats (palpitations): When the heart muscle does not pump well, the heartbeat speeds up to help the heart get enough oxygen-rich blood to major organs and muscles, or the heartbeat may become abnormal.
Other symptoms include a feeling of fullness (bloating) in your stomach, loss of appetite or nausea.
If you have heart failure, you may have one or all of these symptoms. However, some people with heart failure do not have any symptoms. Patients with advanced heart failure generally have symptoms at rest or with minimal exertion such as dressing, bathing, shaving, walking stairs, and even with conversation.
Diagnosis

How is it diagnosed?
To diagnose heart failure, your doctor will first ask you questions about your symptoms and medical history. Your doctor will want to know:
- If you have any other health conditions such as diabetes, kidney disease, high blood pressure, heart rhythm disorders, high cholesterol, coronary artery disease or other heart problems
- If you have a family history of heart disease or sudden death
- If you smoke or use tobacco
- If you drink alcohol and how much you drink
- If you have been treated with chemotherapy and/or radiation
- What medications you are taking
Your doctor will perform a complete physical exam and will look for signs of heart failure as well as any other illnesses that may have caused your heart muscle to weaken or stiffen.
What tests will the doctor do to get a diagnosis?
Certain tests can help your doctor determine the cause and severity of your heart failure. Your doctor will tell you which of these tests you should have:
Blood tests
Used to evaluate kidney and thyroid function, as well as to check cholesterol levels and the presence of anemia. Anemia is a blood disorder that occurs when there is not enough hemoglobin (the substance in red blood cells that allows the blood to transport oxygen through the body) in a person’s blood.
B-type natriuretic peptide (BNP or NT Pro BNP) blood test
BNP is a substance secreted from the ventricles (lower chambers of the heart) in response to changes in pressure that occur when heart failure develops and worsens. The level of BNP in the blood increases when heart failure symptoms worsen, and decreases when the heart failure condition is stable. The BNP level also indicates if your heart failure condition is declining and can provide information about your prognosis. In addition, the BNP level helps your healthcare provider determine if your shortness of breath is due to heart failure.
Cardiac catheterization
An invasive imaging procedure that involves putting a catheter into a blood vessel in the arm or leg and guiding it to your heart with the aid of a special X-ray machine. There are two types of cardiac catheterization, left and right. In a left heart catheterization, contrast dye may be injected through the catheter, and X-ray videos of your valves, coronary arteries and heart chambers are taken. Cardiac catheterization is also called coronary angiography. Right heart catheterization does not require contrast dye and is used to measure heart function.
Chest X-ray
This shows the size of your heart and whether there is fluid buildup around the heart and lungs. Echocardiogram (echo)
A graphic outline of the heart’s movement. During an echo, a special ultrasound wand is used to record pictures of the heart’s valves and chambers to study the pumping action of the heart. Echo is often combined with a Doppler test to find changes in the blood flow across the heart’s valves and the pressure in the heart’s chambers.
Echocardiogram (echo) — A graphic outline of the heart’s movement. During an echo, a special ultrasound wand is used to record pictures of the heart’s valves and chambers to study the pumping action of the heart. Echo is often combined with a Doppler test to find changes in the blood flow across the heart’s valves and the pressure in the heart’s chambers.
Ejection fraction (EF)
A measurement of the blood pumped out of the heart with each beat. Your EF can be measured in the doctor’s office during an echocardiogram (echo) or other tests such as a multigated acquisition (MUGA) scan, cardiac catheterization, nuclear stress test, or magnetic resonance imaging (MRI) scan of the heart. A normal EF ranges from 55 percent to 70 percent. It is important for your doctor to know your EF, which can go up and down based on your heart condition and the effectiveness of the prescribed therapies. It is important to have your EF measured initially and as needed, based on changes in your condition. Ask your doctor how often you should have your EF checked. (See EF box below for more information.)
Electrocardiogram (EKG or ECG)
This test records the electrical impulses in the heart. During the test, small, flat sticky patches called electrodes are placed on your chest. The electrodes are attached to an electrocardiograph monitor that charts your heart’s electrical activity on graph paper.
Genetic testing – In some cases, your doctor may suspect a specific heart condition that is passed along the family via inheriting a genetic mutation (a change in the coding of some proteins) in your body. This is becoming increasingly recognized as one out of five patients with heart failure may have such abnormalities. It can sometimes be identified with a careful medical history of family members and confirmed by a blood test. The benefit to undergoing genetic testing is that once a disease-causing gene is identified, other family members may get checked to determine if they are vulnerable to the same disease. This allows doctors to follow those at risk, while many treatment strategies are under development with the hope of preventing the progression of diseases with genetic mutations.
Multigated acquisition (MUGA) scan
A nuclear scan that evaluates the pumping function of the ventricles.
Stress test
An exercise stress test is used to provide information about how the heart responds to stress. It usually involves walking on a treadmill or pedaling a stationary bike at increasing levels of difficulty, while the ECG, heart rate and blood pressure are monitored. If you are not able to do activity, medications may be used to “stress” the heart. This is called a pharmacological stress test.
More About the Ejection Fraction
Your ejection fraction (EF) can go up and down, based on your heart condition and the therapies that have been prescribed. Your EF is used to measure how well your heart pumps with each beat to determine the level of systolic dysfunction. Data obtained on an echocardiogram can tell us if you have heart failure with diastolic dysfunction.
Left ventricular ejection fraction (LVEF) is the measurement of how much blood is being pumped out of the left ventricle of the heart (the main pumping chamber) with each contraction. Right ventricular ejection fraction (RVEF) is the measurement of how much blood is being pumped out of the right side of the heart to the lungs for oxygen. In most cases, the term “ejection fraction” refers to LVEF.
| EF % | Pumping ability of the heart |
|---|---|
| Above 50% | Normal |
| Below 50% | Below normal |
Treatments

What is the treatment for heart failure?
Depending on the cause of your heart failure, initial treatments for mild to moderate heart failure will include regular exercise, quitting smoking, treatment for hypertension (medication and a low-sodium diet), lipid disorders (cholesterol) treatment, discontinuing alcohol or certain drugs, an angiotensin converting enzyme inhibitor (ACE-I), an angiotensin II receptor blocker (ARB) ) or sacubitril/valsartan (Entresto). Beta blockers are essential for all patients with heart failure. Often as heart failure becomes advanced, patients may become intolerant of beta-blockers or other heart failure medications. Most patients with heart failure also receive aldosterone antagonists (spironolactone and eplerenone), which reduce reduce the risk of death and the need for hospitalization. Your doctor will check to make sure you are taking the medications proven to help.
How do you know if it advances?
If heart failure is advancing, you’ll notice an increase in these symptoms: shortness of breath, fatigue and reduced ability to exercise. For Stage B people diagnosed with systolic left ventricular dysfunction, but who do not currently have symptoms of heart failure (pre-heart failure), the diagnosis is usually made when an EF of less than 40 percent is found during an echocardiogram test. This includes people with prior heart attack, valve disease and cardiomyopathy. Patients at Stage C often have known systolic heart failure and current or prior symptoms.
What are the treatment options?
All people with Stage B heart failure should take a medication such as an angiotensin converting enzyme inhibitor (ACE-I) or angiotensin II receptor blocker (ARB) or sacubitril/valsartan (Entresto) and a beta-blocker. Surgery or interventional options for coronary artery blockage, heart attack, and valve repair or replacement (as appropriate) should be discussed.
Usual treatments for Stage C heart failure include:
- Medications such as an angiotensin converting enzyme inhibitor (ACE-I) or angiotensin II receptor blocker (ARB) and a beta-blocker will be prescribed to help the heart muscle pump with less work
- An aldosterone antagonist will be prescribed
- Hydralazine/nitrate combination may be prescribed if symptoms persist or you cannot tolerate ACE-I
- Diuretics (water pills) are used in most patients
- Digoxin is used in many patients with persistent symptoms
- Restrict dietary sodium (salt) to 2,000 mg per day
- Monitor weight daily and report a change of 2 pounds in 1 day or 5 pounds over the course of a week
- Restrict fluids (as appropriate)
- Implanted defibrillator with or without cardiac resynchronization therapy (biventricular pacemaker) may be recommended
- Catheter-based mitral valve repair (Mitraclip) may be recommended
Patients should be evaluated to determine if the following treatments are available options: heart transplant, ventricular assist devices, surgery options, continuous infusion of intravenous inotropic drugs, end-of-life (palliative or hospice) care, or research therapies.
What are my options for surgical management of heart failure?
Coronary Artery Bypass Graft (CABG) Surgery
The most common surgery for heart failure treatment is bypass surgery. If a coronary artery becomes blocked, less oxygen-rich blood reaches the heart muscle. The heart muscle becomes “starved” for blood (ischemia) and is unable to pump normally; heart failure occurs. Your doctor will determine if your heart failure is caused by coronary artery disease and if you have blockages that can be “grafted” or bypassed. Although patients with heart failure are at an increased surgical risk, new strategies before, during and after surgery have decreased the risk and improved outcomes.
Valve Surgery
As heart failure progresses, remodeling of the left ventricle causes the papillary muscles (which support the mitral valve leaflets) to stretch out of shape, causing the valve to leak. Mitral valve repair usually involves reshaping the leaflets and providing support to the mitral valve with a ring. Experience at Cleveland Clinic has shown that repair of the mitral valve:
- Preserves the natural anatomy of the heart
- Improves cardiac function
- Decreases symptoms
- Improves survival
- Decreases complications and risks
If the aortic valve does not open fully or if it leaks, surgical aortic valve replacement may be an option.
Percutaneous Valve Procedures
A less invasive procedure than open heart surgery, called a percutaneous heart valve replacement, can be performed for patients with heart failure who have narrowing or leakage of the heart valves. This newer interventional procedure involves the insertion of an artificial heart valve using a catheter. The entry portal is via the femoral vein or artery, or directly through the myocardium. An expandable prosthetic heart valve is inserted at the site of the diseased native valve. Likewise, sometimes a leaking mitral valve can be repaired with a procedure performed in the cath lab where the valve is stapled with a clip. This mitral clip procedure does not require a chest incision and the hospitalization may be as short as two days.
Heart Transplant
When medications and surgery fail to manage heart failure symptoms and progression, cardiac transplant is considered as a treatment option. Cleveland Clinic is one of the largest heart transplant programs in the United States with excellent survival rates due to the following: selection of appropriate candidates and donors; improvement in pre-transplant support; advances in immunosuppressant medications, and better protection from infection. Heart transplant involves replacing a diseased heart or heart and lungs with a healthy donor organ or organs. The donor organ is completely removed from someone who has died, then kept cool in a special solution as it is transported. The diseased heart is removed, leaving the back walls of the atria (heart’s upper chambers). The heart is sewn, atria to atria into the chest, the blood vessels are reconnected, and blood flows through the new heart into the body.
Before someone is placed on the heart transplant list, they complete a thorough, careful evaluation process. A multidisciplinary team of heart doctors, nurses, social workers and other healthcare professionals reviews the medical history, diagnostic test results, social history and psychosocial evaluation results to see if the patient is able to survive the heart transplant procedure and then comply with the continuous care needed to live a long healthy life.
Once the person is approved to be placed on the list, they must wait for a donor to become available. This process can be long and stressful. In some cases, a person may need to be bridged to a heart transplant with an LVAD or may be offered an LVAD if heart transplant is not a suitable treatment option for them (see page 9).
Percutaneous Valve Procedures
A less invasive procedure than open heart surgery, called a percutaneous heart valve replacement, can be performed for patients with heart failure who have narrowing or leakage of the heart valves. This newer interventional procedure involves the insertion of an artificial heart valve using a catheter. The entry portal is via the femoral vein or artery, or directly through the myocardium. An expandable prosthetic heart valve is inserted at the site of the diseased native valve.
Likewise, sometimes a leaking mitral valve can be repaired with a procedure performed in the cath lab where the valve is stapled with a clip. This mitral clip procedure does not require a chest incision and the hospitalization may be as short as two days.
FAQ's
What if I progress to Stage D advanced heart failure?
Stage D is end stage, irreversible. Patients who develop severe advanced heart failure may benefit from special treatments, such as a ventricular assist device (VAD) or cardiac transplantation. If your quality of life is very poor, or your doctor has told you that your condition is very severe, please ask about these treatments.
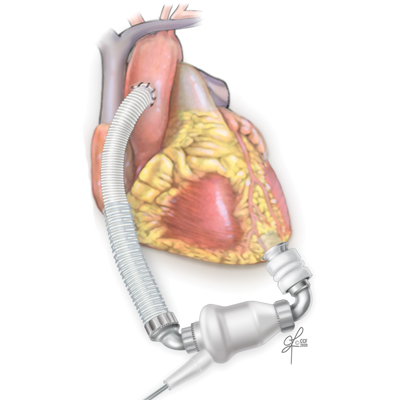
What is an LVAD?
A left ventricular assist device (LVAD) is a mechanical pump used to restore blood flow and support heart function in people who have advanced heart failure. The device operates like a healthy heart by taking blood from the left lower chamber of the heart and pumping it through the body to the organs.
How is the LVAD used for advanced heart failure?
A left ventricular assist device (LVAD) is often thought of as the “bridge to transplantation” for those whose medical therapy has failed and are hospitalized with end-stage systolic heart failure. This device helps your heart pump blood throughout your body. Cleveland Clinic is one of the few institutions worldwide that has access to all clinically available mechanical ventricular assist systems, including the Heartmate II®, HVAD, and Impella® devices, allowing us to choose the device that will best suit an individual patient’s clinical needs, whether it be a permanent or temporary solution. Cleveland Clinic also participates in clinical trials so we are able to offer the newest technology developed for our patients.
For selected individuals with severe refractory heart failure, we offer the option of permanent LVAD therapy — or “destination therapy.” Destination Therapy refers to the implantation of an LVAD for the long-term, rather than as a bridge to transplantation.
It is a permanent support device for advanced stage heart failure patients who do not qualify for a heart transplant.
Who is eligible to receive an LVAD?
An LVAD is a treatment option for certain patients with end-stage heart failure. Your doctor will determine if an LVAD is an appropriate treatment for you, based on your medical condition, symptoms, age, body size and the presence of other medical conditions.
An LVAD may not be the appropriate treatment choice for some patients who have blood clotting disorders, irreversible kidney failure, severe liver disease, severe lung disease, or infections that cannot be treated with antibiotics.
How will it be determined that you’re a good candidate for the LVAD?
To determine if an LVAD is the best treatment for you, patients are evaluated by a team from Cleveland Florida’s Heart & Vascular Center. In addition, your team cares for you after you get your LVAD as an inpatient and after you leave the hospital for all follow-up outpatient appointments. The team consists of:
- Heart failure cardiologists
- Cardiac surgeons
- Nurse practitioners and physician assistants
- Social workers
- Bioethicists
- Palliative medicine specialists
- Cardiac rehabilitation specialists
- Dietitians
- And other team members as needed; for example, you may need to see a lung specialist or kidney doctor if these organs have been affected by your illness
Tests may include routine blood work, chest X-ray, electrocardiogram (EKG), echocardiogram, left and right heart catheterization, or others. These tests may be ordered by your heart failure cardiologist or by the surgeon. Some of these tests may have been performed before and will only be repeated if they were not recently performed (within the last six to 12 months), depending on the type of test.
What are the risks of the LVAD implantation procedure?
As with any surgical procedure, there are risks to the LVAD implantation procedure. Your doctor will talk with you about the specific risks and potential benefits of this procedure. Some of the possible risks include bleeding, development of blood clots, respiratory failure, kidney failure, stroke, infection and device failure. Special precautions are taken to decrease these risks.
There may be other possible risks. When you meet with your doctor, please ask questions to make sure you understand why the procedure is recommended and the potential risks of the procedure for you.
How does the LVAD work?
An LVAD does not replace the heart. It receives blood from the left ventricle and delivers it to the aorta. It assists the patient’s own heart to pump blood throughout the body, decreasing the work of the left ventricle.
The LVAD may provide blood pressure support; maintain or improve other organ function by improving blood flow to the kidneys, liver, brain and other organs; when used as destination therapy or bridge-to-transplant, improve the patient’s strength and ability to participate in activities (i.e., cardiac rehabilitation); and allow the patient to be discharged from the hospital.
What are the components of the LVAD?
There are a few different types of LVADs available at Cleveland Clinic. The type of LVAD selected will depend on each patient’s individual needs and medical condition. The components of the LVAD vary according to the specific device used. In general, the device consists of a pump unit (which is implanted in the chest), a controller, and an energy or power supply.
How will I live with my LVAD?
To enhance quality of life, all patients with an LVAD must carefully follow the guidelines provided by their healthcare team.
After the implantation procedure, a detailed education program is provided to you and your caregivers to ensure safe and proper use of the device. You’ll learn how to manage the device and trouble-shoot potential emergency situations. You’ll be required to demonstrate your knowledge about the device before you are discharged from the hospital. You’ll also need to exhibit independence with self-care activities before you are discharged.
In addition, you’ll be given guidelines about your activities, including showering and resuming sexual activity; as well as information on your medications, diet, and when to call the doctor.
At home, you’ll need to have an accurate scale as well as a thermometer. Some patients will need to monitor their blood pressure at home. Your nurse will provide specific guidelines. You will receive information about how to reach the healthcare team when necessary. At Cleveland Clinic, a medical team member will always be available to answer your questions, 24 hours a day, seven days a week.
Why Choose Us?
Our heart specialists are the best in the country. The Heart & Vascular Institute at Cleveland Clinic Florida is one of the region’s leading centers for comprehensive cardiac care. Cleveland Clinic Florida ranked #1 in the Miami-Fort Lauderdale metro area and is a top hospital in Florida, according to U.S. News & World Report’s “2019-20 Best Hospitals” rankings.
Cleveland Clinic Florida’s Section of Heart Failure consists of full-time heart failure and transplant cardiologists, heart failure surgeons, transplant surgeons, nurse clinicians, transplant coordinators and additional support staff. An integral part of our Heart Failure program, is the Cardiomyopathy Clinic which creates individualized treatment plans for patients with complex cardiomyopathies and heart failure disease.
Heart failure is the number one reason for hospitalization among patients who receive Medicare benefits. It is also the most common reason patients need to be hospitalized again within 30 days of leaving the hospital after treatment for heart failure. In addition to our Heart Failure Intensive Care unit, is a special nursing unit designed for our less critical patients with heart failure. To help reduce the risk of readmission, the staff developed and tested a multidisciplinary checklist and program used throughout the Heart & Vascular Institute to make sure every patient knows how to manage their heart failure once they go home. The use of this checklist has reduced the rates of readmission and improved patient satisfaction.
Since 2011, Cleveland Clinic Florida has maintained the American Heart Association’s Get With The Guidelines(R) Heart Failure GOLD Plus Certification for improving the quality of care for patients with heart failure. Gold Plus distinction recognizes hospitals for their success in using Get With The Guidelines treatment interventions. This quality improvement program provides tools to guide evidence-based therapies and procedures in managing heart failure across the continuum of disease progression.
Patient Services
MyChart
Cleveland Clinic's MyChart is a secure, online health management tool that connects patients to portions of their electronic medical record, allowing you to see test results, message your physician, schedule appointments and more. You can also manage the healthcare of your loved ones with MyChart • Caregiver.
Concierge Medicine
Cleveland Clinic Florida’s Concierge Medicine Program creates a unique opportunity for personalized medical care. For more information about our Concierge Medicine program, please fill out our contact form or call our direct line for patient inquires at 800.700.4275.
Appointments
Ready to schedule an appointment with Cleveland Clinic Florida’s Heart & Vascular Institute? Call 877.463.2010 for Cleveland Clinic Weston Hospital and Cleveland Clinic Indian River Hospital and 844.630.4968 for Martin Health to make an appointment that works for you.
MyConsult® Online Medical Second Opinion
MyConsult Online Second Opinion program connects patients to the expertise of top Cleveland Clinic specialists without the time and expense of travel. Through our secure web platform, patients can submit their detailed health information, medical records and diagnostic test results. The most appropriate Cleveland Clinic expert is assigned to the consultation and will render a detailed second opinion. The report includes commentary about the diagnosis and treatment options or alternatives and recommendations regarding future therapeutic considerations. Patients are also able to send additional questions to the physician who provided the report. Online medical second opinions are available for more than 1,200 medical diagnoses.
