Overview
A normal foot and ankle has 26 bones, 33 joints, and more than 100 muscles, tendons and ligaments. The average person will walk the equivalent of four times around the world in his or her lifetime. So it’s hardly surprising that nearly three-quarters of Americans will eventually experience some type of foot problem. In athletes, these problems are even more common.
Yet proper foot care is not something most of us think about until problems put us off stride.
Cleveland Clinic's Foot & Ankle Center provides comprehensive services for all adult foot and ankle problems including diagnosis, treatment and rehabilitation.
Our orthopaedic surgeons, physician assistants, podiatrists, nurse clinicians, certified pedorthists and technicians will get you back on your feet so that you can live life to its fullest.
Ankle Arthritis
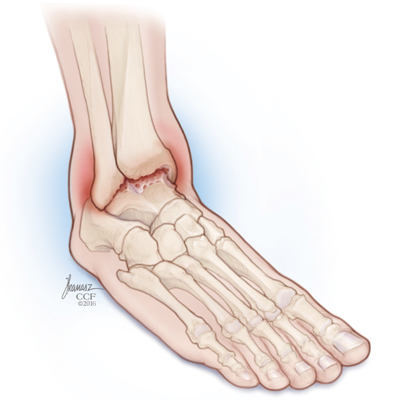
Arthritis is a general term for a group of more than 100 diseases. Arthritis is an acute or chronic inflammation of a joint and its surrounding soft tissues. The word “arthritis” means “joint inflammation.” Arthritis can affect just about any joint in the foot, from the ankle to the toes.
In ankle arthritis, progressive ankle joint deterioration occurs and the smooth “cushioning” cartilage between the shin bone and the ankle bone is gradually lost, resulting in the bones wearing against each other. Soft tissues in the joints also may begin to wear down. Ankle arthritis can be painful and eventually can result in limited motion, loss of joint function, and deformity.
The most common form of arthritis is osteoarthritis or “wear-and-tear” arthritis, which becomes more prominent as people age. Osteoarthritis also can develop after the joint sustains an injury, called “post-traumatic” arthritis.
What are the symptoms of ankle arthritis?
Symptoms of ankle arthritis often involve:
- Tenderness or pain
- Reduced ability to move or walk
- Stiffness in the joint
- Swelling in the joint
How is ankle arthritis diagnosed?
The diagnosis of ankle arthritis most likely will involve:
- A preliminary medical history in which the doctor asks questions about when and where the pain began
- A physical exam looking for signs of arthritis, such as swelling or loss of motion of the ankle joint
- X-rays looking for the tell-tale signs of arthritis, such as bone spurs and narrowing of the space between the shin bone and the ankle bone
How is ankle arthritis treated without surgery?
The initial treatment of ankle arthritis involves several different nonsurgical treatments, including:
- Anti-inflammatory drugs to reduce ankle swelling and discomfort
- Physical therapy
- Braces to support or stabilize the ankle
- Weight control
- Nutritional supplements
- Steroid medication injected into the ankle to decrease inflammation
- Pain relievers
What surgical treatments can help to treat ankle arthritis?
Surgery is considered if nonsurgical treatments do not provide enough relief of symptoms. There are several different surgical options for treating ankle arthritis. Physicians tailor surgery to each individual patient’s unique symptoms. The following are some of the surgical options for ankle arthritis:
- Arthroscopic surgery – This kind of surgery can help in early stages of ankle arthritis. In arthroscopic surgery, an arthroscope (a small instrument about the size of a pencil) is inserted into the ankle joint. The instrument projects an image onto a monitor that is viewed by a surgeon. The surgeon can then use tiny forceps, knives, and shavers to clean out the arthritic ankle. Arthroscopic surgery can help to remove scar tissue, damaged cartilage or bone spurs from the joint, which can ultimately help decrease symptoms.
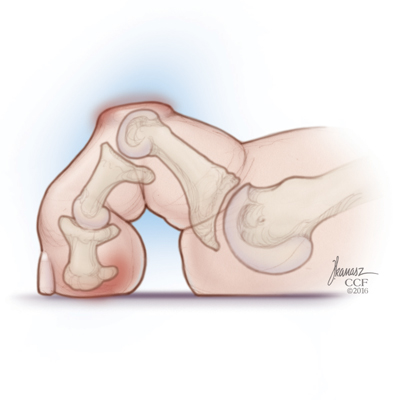
- Fusion surgery – This kind of surgery, also called arthrodesis, involves using metal plates, screws or nails to get the shin and ankle bones to heal into one bone. The goal of ankle fusion is to relieve pain and restore function to the affected ankle by eliminating the painful motion. Among the benefits of fusion surgery are pain relief, a stabilized joint, the ability to bear weight on the fused joint without pain and the ability to walk and perform usual activities. Fusion is also an excellent way to correct any deformity.
- Joint replacement surgery – This kind of surgery involves replacing a worn out ankle with an artificial one. In ankle replacement surgery, a man-made ankle joint is implanted between the shin bone and the ankle bone. Your surgeon can choose from a number of artificial ankle devices. They are generally made from metal and plastic parts, and are very durable. Unlike ankle fusion, ankle replacement preserves some of the ankle’s normal up and down motion, making it a good alternative to ankle fusion surgery in some patients with ankle arthritis. Studies show that total ankle replacement can safely relieve the pain of ankle arthritis, improve the ability to walk and improve quality of life. However, ankle replacement is a more complex procedure than ankle fusion. Not everyone with ankle arthritis is a candidate for ankle replacement. Specifically, patients with severe deformity or instability of the ankle or with associated medical problems (such as diabetes or poor blood supply) are probably best treated with a simpler procedure such as fusion. Because ankle replacement is a relatively new procedure, we do not yet know how long ankle replacements will last. Outcomes for this surgery are very good thus far.
Ankle Fracture
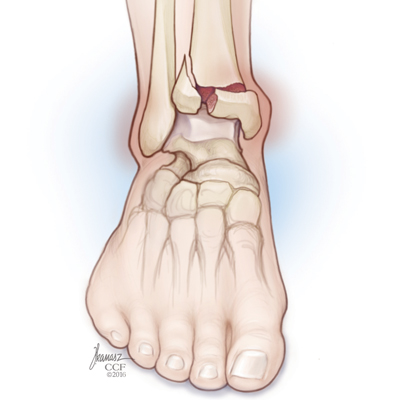
A fracture is a broken bone. If not treated properly, a fracture can lead to long-term disability. A fracture may be closed (the broken bone does not break through the skin) or open (the skin is torn over the fracture site). A stress fracture is a particular type of fracture that is common in the foot and ankle. A stress fracture is a hairline crack in a bone caused by overuse of a bone. Most fractures of the ankle are not stress fractures. Ankle fractures usually occur after a forceful twisting injury. When a fracture of an ankle bone occurs, it is essential to obtain a prompt evaluation for proper diagnosis and treatment. With early diagnosis, appropriate treatment, and correct rehabilitation, a painless, properly functioning ankle is possible.
Signs of a fracture
Accidents are the most common cause of ankle fractures and include motor vehicle, slips and falls, and sports injuries. Symptoms and signs of fractures include:
- Swelling
- Tenderness
- Pain
- Deformity
- Difficulty bearing weight
- Popping sound or sensation
How is this treated?
Treatment can include surgical or nonsurgical options. Nonsurgical treatment usually consists of a period of immobilization in a boot or cast, followed by some type of rehabilitation. Surgical treatment utilizes internal fixation devices such as screws and plates to hold the bones in the correct position until they heal together. Surgery also usually requires a period of immobilization in a boot or cast, followed by rehabilitation. Both treatments are frequently combined with a non-weightbearing period using crutches or a walker, or protected weight bearing as pain allows. Often, the decision on surgical vs. nonsurgical treatment is based on the pattern of injury, the amount of displacement, whether ligaments are also injured as well as the age and activity level of the individual.
What are the risks of treatment?
The risks of surgical and nonsurgical treatment include:
- Joint stiffness
- Nonunion (the bone fails to mend together)
- Malunion (the bone heals in the wrong position)
- Arthritis
With surgery, infection and nerve injuries can also occur, although the rate of this complication is low and the outcomes are generally good. Skin healing can be slow in this area of the body.
Ankle Sprain
Ankle sprains are an extremely common injury, with an estimated 23,000 ankle sprains occurring in the United States every single day. Many sprains occur during sports such as tennis, basketball, soccer and volleyball, but even more occur during everyday activities. Twisting the ankle on a curb and slipping going down stairs are common ways to injure the ankle. An ankle sprain occurs when the foot inverts or turns in, resulting in stretching and tearing of the ligaments on the outside of the ankle.
What are the symptoms of an ankle sprain?
- Swelling over the outside of the ankle
- Bruising
- Pain and soreness on the outside of the ankle
- Difficulty walking
- A feeling of instability in the ankle
What is the treatment for an ankle sprain?
- R.I.C.E. therapy (rest, ice, compression, elevation)
- Bracing or wearing an immobilizing boot
- Nonsteroidal anti-inflammatory medications (NSAIDs) to reduce inflammation and relieve pain
- Avoiding uneven ground
- Avoiding high intensity sports
- Supervised physical therapy — This is probably the most important aspect of treatment. Physical therapy is critical to help restrengthen the ankle and prevent future injuries
How long does it take to recover from an ankle sprain?
- Minor sprains may improve in a few weeks
- Severe sprains may take three to six months for full recovery
What long-term problems can occur after an ankle sprain?
- Injured cartilage or tendon
- Scar tissue
- Persistent pain
- Repeated ankle sprains, or chronic instability — This is the most common complication of a sprained ankle. Even though the ankle ligaments usually heal, they may be looser than normal and result in recurrent ankle sprains. If sprains continue to occur despite physical therapy and bracing, surgery can be extremely successful at tightening the ankle ligaments and stabilizing the ankle.
RICE for Foot and Ankle Injuries
If you sprain your ankle or suspect you have a fracture, use R-I-C-E until medical care is available:
- Rest – keep weight off of the ankle as soon as possible
- Ice – follow the cycle of 20 minutes on/20 minutes off ice often throughout the day
- Compression – bind the ankle with an Ace® bandage to avoid frostbite from icing and to reduce swelling
- Elevation – keep the foot and ankle above heart level by propping it on a pillow
Plantar Fasciitis
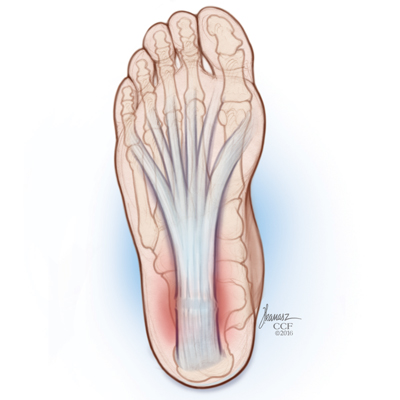
The plantar fascia is tight band of strong tissue on the bottom of the foot that helps support the arch. This band is attached to the heel bone and extends all the way to the toes. Plantar fasciitis is a common condition in which the plantar fascia becomes inflamed and painful. This condition affects virtually all people at some time, but is particularly common in runners and those who stand for prolonged periods of time. In the past, heel spurs were thought to cause heel pain, but currently the fascia is considered the primary source of discomfort in this area.
What are the symptoms of plantar fasciitis?
Because the plantar fascia attaches to the heel bone, this is where the pain is usually the worst. Because the fascia becomes particularly stiff at night, pain is usually worse in the morning when the patient begins to walk. The pain often is aggravated by standing, walking and especially running.
What is the treatment for plantar fasciitis?
The mainstay of treatment is plantar fascia stretching. This is best done by sitting cross-legged and pulling the toes back toward the shin. This stretch should be performed before getting out of bed in the morning and repeated at least hourly. You can also stretch by standing on a step and lowering the heels below the step. Other treatments include:
- Activity modification
- Heel gel pads
- Orthotic arch supports
- Avoiding barefoot walking or standing
- Anti-inflammatory medicine (by mouth, for two to three weeks)
- More supportive shoes
- Physical therapy (including ice and stretching)
- Night splint and/or a walking cast for three to six weeks
- Corticosteroid injection
- Shock wave therapy may reduce pain and promote healing of this condition. This type of energy wave treatment (i.e., strong sound waves) is often tried prior to surgery.
- Platelet-rich plasma injections
- Surgery (rarely necessary)
How long does plantar fasciitis take to get better?
Plantar fasciitis does not resolve quickly. Most patients will experience improvement slowly. It may take up to six months.
Achilles Ruptures
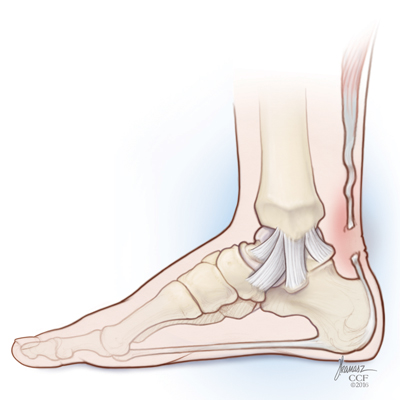
The Achilles tendon is a large rope-like band of tissue in the back of the ankle that connects the powerful calf muscles to the heel bone. Sometimes called the heel cord, it is the largest tendon in the human body. When the calf muscles contract, the Achilles tendon is tightened, pulling the heel bone and pointing the foot downward. It is vital to such activities as walking, running and jumping. A complete tear through the tendon, which usually occurs about two inches above the heel bone, is called an Achilles tendon rupture.
The Achilles tendon is under a tremendous amount of stress and can develop wear and tear over time. This may make the tendon more susceptible to rupture. Certain illnesses (such as rheumatoid arthritis and diabetes) and medications (such as corticosteroids and certain antibiotics) can also increase the risk of rupture.
Ruptures frequently occur in the middle-aged male athlete, the so-called “weekend warrior.” Injury often occurs during recreational sports that require bursts of jumping, pivoting, and running such as tennis, racquetball, basketball and badminton.
What are the symptoms of an Achilles tendon rupture?
- A sudden and severe pain at the back of the ankle or calf – often described as “being hit by a rock, or shot”
- A loud pop or snap
- A gap or depression in the tendon about two inches above the heel bone
- Initial pain, swelling and stiffness may be followed by bruising and weakness
- The patient may be unable to walk, but frequently the other muscles in the leg provide enough strength so that walking is still possible
- Difficulty standing on tiptoe and pushing off when walking
How is an Achilles tendon rupture treated?
The goal of treatment is a healed tendon with normal strength and tension allowing return to preinjury activity. Treatment may be accomplished using nonsurgical or surgical techniques.
Nonsurgical Treatment
This involves a period of immobilization in a cast or boot to allow the tendon to heal on its own. The foot is initially positioned pointing down to allow the tendon ends to begin to heal to each other. The foot is gradually brought up as the healing progresses. Weight bearing is initially limited and also progressed during the course of treatment. The major benefit of this form of treatment is that it is safe and avoids potential surgical complications. However, the tendon may not heal at the appropriate tightness which can result in weakness. The tendon is also at higher risk for a reinjury compared to surgical treatment.
Surgical Treatment
Surgical treatment involves making an incision and using stitches to repair the rupture. This results in a stronger repair with the appropriate tightness. Some repairs are augmented with graft tissue.
Both surgical and nonsurgical treatment will require an initial period of about six to 10 weeks of casting or special braces. The cast may be changed at two- to four-week intervals to slowly stretch the tendon back to its normal length. Casting may be combined with early movement (one to three weeks) to improve overall strength and flexibility.
A heel lift device and regular physical therapy follow for the remainder of treatment.
Consultation with an orthopedic surgeon will determine the treatment and follow up that is right for you.
Achilles Tendonitis
Achilles tendonitis is an inflammation of the tendon and frequently develops in association with activities that put a great deal of repetitive strain on the Achilles. These activities include basketball, running, cycling and even walking. Tendonitis often develops when there has been a change in a person’s usual activity. For example, Achilles tendonitis may develop after a jogging program is started or after a new fitness class is begun.
What are the symptoms of Achilles tendonitis?
Symptoms include pain and stiffness in the back of the ankle along the tendon, especially when stretching or bending the foot back. There may also be mild swelling along the tendon. If the tendonitis has been present for a long time, the tendon may appear enlarged as a result of scar tissue being formed in the tendon.
What is the treatment for Achilles tendonitis?
- Relative rest – This means decreasing the particular activity that likely caused the symptoms.
- Orthotics – Wedges, heel lifts and stable shoes will help correct biomechanical imbalances that may be contributing to Achilles tendonitis.
- Various braces or immobilization boots
- NSAIDs (nonsteroidal anti-inflammatory drugs) – Help decrease the swelling and inflammation that are causing the pain.
- Stretching – Once the pain has subsided, stretching is considered an important tool to prevent recurrence of Achilles tendonitis. Stretching should be gentle and proceed only until tightness is felt. If stretching becomes painful, then you are pushing too far. Leaning against a wall while trying to keep the foot and heel flat on the ground is an excellent way to stretch the Achilles.
- Calf strengthening – Calf raises can help strengthen the Achilles tendon. In particular, lowering down very slowly after going up onto the tiptoes has been shown to be beneficial in the treatment of Achilles tendonitis.
- Ultrasound is used to help stimulate formation of new tissue while phonophoresis is used to reduce swelling and promote healing.
- Shock wave therapy may reduce pain and promote healing of this condition. This type of energy wave treatment (i.e., strong sound waves) is often tried prior to surgery.
- Surgery – If symptoms fail to subside after six months of conservative treatment, surgery to repair the damaged tendon becomes an option. Surgery usually involves removal of the abnormal tendon. In severe cases, nearby tendons are rerouted to help further strengthen the Achilles.
Diabetic Foot Care
Foot problems are a major reason for hospitalizations in patients with diabetes. Because minor injuries can lead to major infections, it is important for people with diabetes to keep their feet healthy. Prevention is the key to avoiding foot problems.
What are some common diabetic foot problems?
- Foot ulcers
- Swelling
- Cuts and sores
- Corns
- Ingrown toenails
- Deep infections
- Charcot fractures
- Deformities with bony prominences
- Decreased sensation (neuropathy)
What causes diabetic foot problems?
Diabetes affects nerves in the foot, decreasing normal sensation. This loss of sensation, called neuropathy, increases the risk of injury and ulceration. Because patients with diabetes cannot feel foot injuries like those without diabetes, they may inadvertently ignore foot problems. Therefore, pain is not an early indicator of problems in diabetic patients. Poor circulation and decreased immunity to infection can also lead to serious diabetic foot problems.
What are the symptoms of a diabetic foot problem?
Swelling and redness of the foot may be the only signs of a developing problem. Drainage on a sock can indicate an ulcer. However, ulcers, infections and other problems in the diabetic foot may be painless due to neuropathy. As a result, routine self-inspection of each foot is extremely important for prevention and early detection of problems.
What can be done to prevent problems in the diabetic foot?
- Wear wide shoes with extra depth in the toe box that fit properly, and avoid large seams on socks
- Inspect each foot daily for blisters, cuts, sores and other problems
- Avoid going barefoot
- Avoid exposure to temperature extremes
- Do not self-treat corns, calluses or ingrown toenails
- See a podiatrist for routine maintenance and treatment
- Have regular foot examinations
- Avoid severe dryness and cracking of the skin by regularly applying moisturizing cream to the feet
- Control your diabetes by monitoring blood sugar levels and taking prescribed medications
- Do not ignore minor problems
How are diabetic foot problems treated?
Many diabetic foot problems can be managed without surgery by using special shoes, braces and standard wound care. Serious foot problems that have resisted nonsurgical treatment methods may require surgery.
What surgeries may be performed to treat the diabetic foot?
- Hammertoe correction
- Ulcer debridement
- Removal of infected tissue
- Lengthening of the Achilles tendon
- Removal of bone prominences
- Excision of infected bone
- Realignment of the deformed foot
- Stabilization of the unstable foot
What are the risks of treatment?
- Recurrence or worsening of infection
- Recurrence of ulceration
- Failure of the surgical incision to heal
- Failure of the bone to heal
Cleveland Clinic Diabetic Foot Care Program
The Diabetic Foot Care Program was developed to reduce the burden of foot disease on people with diabetes. Drawing on Cleveland Clinic expertise, our Diabetic Foot Care Program has three specific goals:
- To provide state-of-the-art care in Diabetic Foot Clinics located at our main campus
- To further the education of patients and health care professionals about diabetes and its effects on the feet
- To conduct research on the prevention and treatment of diabetic foot disease
Bunions
People think of a bunion as being a bump on the side of the foot near the big toe. However, bunions go deeper than what we can see. A bunion actually reflects a change in the anatomy of the foot. Essentially, a bunion develops when the big toe begins to point toward the second toe. This eventually produces the bump on the inside of the foot.
What are the symptoms of bunions?
Many people do not experience symptoms in the early stages of bunion formation. Symptoms are often most noticeable when the bunion gets worse and with certain types of footwear. These include shoes that crowd the toes and high-heeled shoes. When symptoms do occur, they may include:
- Physical discomfort or pain
- A burning feeling along the big toe
- Redness and swelling over the bump
- Possible numbness along the big toe
- Difficulty walking
What causes bunions?
One contributing factor to developing bunions is poorly fitting shoes that are too narrow. Heredity probably also plays a role, as bunions may run in families. Bunions may also develop due to inflammatory conditions, such as arthritis.
Who gets bunions?
Bunions are much more common in women. This is directly related to the popularity of narrow, high-heeled women’s shoes. Males who get bunions are usually adolescents. Males are more likely to have inherited a reason to have a bunion.
How are bunions diagnosed?
Bunions are diagnosed using physical examination and X-rays.
How are bunions treated?
Nonsurgical treatments – The treatment of a bunion always begins with nonsurgical treatments. Many of the treatments are simple. Wider, better fitting shoes are essential. Gel pads can be placed over the painful bump as well. Orthotics, night splints or toe spacers occasionally may help decrease the symptoms. Often, these measures are enough to successfully alleviate pain. Virtually all adolescent bunions are treated nonsurgically at least until the patient is done growing.
Surgical treatments – Surgery is considered if nonsurgical treatments fail to provide satisfactory relief. There are many types of surgical procedures designed to correct each patient’s individual abnormalities. Surgery involves several different steps designed to straighten out the big toe and restore more normal function to the foot. The bump is removed, tight soft tissues are released, and the bone is cut and realigned. Usually, metal pins, screws and/or plates are needed to hold the bones in the right position. Surgery can be very effective at correcting bunions, and the outcomes are generally good.
Hammertoes
Hammertoe refers to a deformity of one of the lesser toes in which the knuckle becomes bent. The knuckle may be flexible and correctable or stiff and rigid.
What causes a hammertoe?
Hammertoes are caused by a muscle imbalance in the toes. Heredity, trauma, arthritis and wearing tight shoes or stockings can all lead to hammertoe formation.
What are the symptoms of a hammertoe?
- Pain at the top of the knuckle from shoes rubbing
- Corns at the top of the knuckle or tip of the toe
- Redness and swelling of the entire toe
- Restricted or painful motion of the toe
- Pain in the ball of the foot at the base of the affected toe
How is hammertoe treated?
- Gel pads can help relieve pressure over the knuckle and tip of the toe.
- Wearing shoes and socks with a deep, wide toe box helps alleviate irritation of the hammertoe.
- Surgery can be performed if nonsurgical treatments fail.
Surgery for a hammertoe aims to correct the deformity, alleviate pain and make wearing shoes more comfortable. Surgery usually involves lengthening tight tendons and removing some of the bone in the toe to allow it to straighten. A pin is needed to hold the toe straight while it heals. This pin may stick out of the tip of the toe. While the pin is in place, the patient must not bear weight on the front part of the foot. Weight on the heel is usually allowed. After four to five weeks, the pin is removed in the doctor’s office. After hammertoe surgery, the toe is stiffer than it used to be, but it is also straighter and easier to fit in a shoe.
What are the risks of surgical treatment?
Risks include infection, problems healing the skin incision, recurrence of the hammertoe and breakage of the pin.
Appointments
To make an appointment with a foot or ankle specialist, call:
- Cleveland Appointments: 216.444.2606
- Akron Appointments: 330.344.2663
- Canton Appointments: 330.489.1362
- Dover Appointments: 330.343.3335
Virtual Second Opinion
If you cannot travel to Cleveland Clinic, help is available. You can connect with Cleveland Clinic specialists from any location in the world via a phone, tablet, or computer, eliminating the burden of travel time and other obstacles. If you’re facing a significant medical condition or treatment such as surgery, this program provides virtual access to a Cleveland Clinic physician who will review the diagnosis and treatment plan. Following a comprehensive evaluation of medical records and labs, you’ll receive an educational second opinion from an expert in their medical condition covering diagnosis, treatment options or alternatives as well as recommendations regarding future therapeutic considerations. You’ll also have the unique opportunity to speak with the physician expert directly to address questions or concerns.
Patient Services
MyChart
MyChart is a secure online tool that provides personalized health information from the privacy of your home at any time, day or night. Learn more or login now.
Virtual Visits
You can now stay connected to your healthcare team through virtual visits, using your smartphone, tablet or computer.
Why go virtual? It's an easy, convenient and secure way to see your provider face-to-face without having to leave home. This saves you travel time, parking fees and time spent in the waiting room — and you can also have a loved one or caregiver join you. If appropriate, you can also get a prescription sent to the pharmacy of your choice.
Many insurance companies cover the cost of virtual visits, so check with your insurance company ahead of time. Interested in getting started? Call your provider to find out what virtual visit options are available.
Learn more about virtual visits for scheduled appointments
Virtual Visits with Orthopaedics
New patients with common knee injuries or knee pain.
Established patients scheduling follow-up care appointments such as:
- Post-Surgical & wound check visits
- Fracture care follow-up
- Injection follow-up
- Musculoskeletal injury follow-up
- Per-operative teaching prior to surgery
Why Choose Us?
At Cleveland Clinic’s Foot & Ankle Center, our goal is simple: to restore you to your normal level of activity — as quickly as possible.
Our center uses a multidisciplinary approach, bringing all of the experts that you need together under one roof, including rheumatologists orthopaedic surgeons, podiatrists, physician assistants, nurse clinicians, certified pedorthists and technicians.