Overview

What is atrial fibrillation?
Atrial fibrillation (AF or AFib) is the most common irregular or abnormal heart rhythm disorder that starts in the atria, affecting more than 3 million Americans today. Instead of the SA node directing the electrical rhythm, many different impulses rapidly fire at once, causing a very fast, chaotic rhythm in the atria. Because the electrical impulses are so fast and chaotic, the atria cannot contract and/or squeeze blood effectively into the ventricle. Thankfully, more options to treat atrial fibrillation are available now than ever before.
At Cleveland Clinic in Florida, our multidisciplinary team of experts in the department of cardiac electrophysiology and pacing can work with you to customize the best treatment plan — which may include medical management, ablation, surgery or combined hybrid approaches — for your atrial fibrillation.
The rate of impulses in the atria can range from 300 to 600 beats per minute.
What do I need to know about atrial fibrillation?
To understand atrial fibrillation, you need to understand the heart’s normal rhythm. Here’s a quick overview:
The heart pumps blood to the rest of the body. During each heartbeat, the two upper chambers of the heart (atria) contract, followed by the two lower chambers (ventricles). These actions, when timed perfectly, allow for an efficient pump. The timing of the heart’s contractions is directed by the heart’s electrical system.
The electrical impulse begins in the sinoatrial (SA node), located in the right atrium. Normally, the SA node adjusts the rate of impulses, depending on the person’s activity. For example, the SA node increases the rate of impulses during exercise and decreases the rate of impulses during sleep.
When the SA node fires an impulse, electrical activity spreads through the right and left atria, causing them to contract and force blood into the ventricles.
The impulse travels to the atrioventricular (AV) node, located in the septum (near the middle of the heart). The AV node is the only electrical bridge that allows the impulses to travel from the atria to the ventricles. The impulse travels through the walls of the ventricles, causing them to contract. They squeeze and pump blood out of the heart. The right ventricle pumps blood to the lungs, and the left ventricle pumps blood to the body.
When the SA node is directing the electrical activity of the heart, the rhythm is called “normal sinus rhythm.” The normal heart beats in this type of regular rhythm, about 60 to 100 times per minute at rest.
Instead of the impulse traveling in an orderly fashion through the heart, many impulses begin at the same time and spread through the atria, competing for a chance to travel through the AV node. The AV node limits the number of impulses that travel to the ventricles, but many impulses get through in a fast and disorganized manner. The ventricles contract irregularly, leading to a rapid and irregular heartbeat.
Causes
What causes atrial fibrillation?
There is no one “cause” of atrial fibrillation, although it is associated with many conditions, including:
- After heart surgery
- Cardiomyopathy
- Chronic lung disease
- Congenital heart disease
- Coronary artery disease
- Heart failure
- Heart valve disease
- Hypertension (high blood pressure)
- Pulmonary embolism Less common causes:
Less Common Causes:
- Hyperthyroidism
- Pericarditis
- Viral infection
In at least 10 percent of the cases, no underlying heart disease is found. In these cases, atrial fibrillation may be related to alcohol or excessive caffeine use, stress, certain drugs, electrolyte or metabolic imbalances, severe infections, or genetic factors. In some cases, no cause can be found.
There are two types of atrial fibrillation. Paroxysmal is intermittent, meaning it comes and goes, and continuous is persistent. The risk of atrial fibrillation increases with age, particularly after age 60.
Diagnosis

How is atrial fibrillation diagnosed?
The most commonly used tests to diagnose atrial fibrillation include:
- Electrocardiogram (ECG or EKG): The ECG draws a picture on graph paper of the electrical impulses traveling through the heart muscle. An EKG provides an electrical “snapshot” of the heart. For people who have symptoms that come and go, a special monitor may need to be used to “capture” the arrhythmia.
- Holter monitor: A small external recorder is worn over a short period of time, usually one to three days. Electrodes (sticky patches) are placed on the skin of your chest. Wires are attached from the electrodes to the monitor. The electrical impulses are continuously recorded and stored in the monitor. After the monitor is removed, a technician uses a computer to analyze the data to evaluate the heart’s rhythm.
- Portable event monitor: A monitor that is worn for about a month for patients who have less frequent irregular heartbeat episodes and symptoms. Electrodes (sticky patches) are placed on the skin of your chest. Wires are attached from the electrodes to the monitor. The patient presses a button to activate the monitor when symptoms occur. The device records the electrical activity of the heart for several seconds. The patient then transmits the device’s recorded information over a telephone line to the doctor’s office for evaluation. The portable event monitor is very useful in determining what heart rhythm is causing your symptoms.
- Transtelephonic monitor: When you develop symptoms of atrial fibrillation, a strip of your current heart rhythm can be transmitted to your doctor’s office over the telephone, using a monitor with two bracelets or by placing the monitor against your chest wall. These monitoring devices help your doctor determine if an irregular heart rhythm (arrhythmia) is causing your symptoms.
These monitoring devices help your doctor determine if an irregular heart rhythm (arrhythmia) is causing your symptoms.
What are the dangers of atrial fibrillation?
Some people live for years with atrial fibrillation without problems. However, atrial fibrillation can lead to future problems.
Atrial fibrillation is associated with an increased risk of stroke, heart failure and even death.
- Because the atria are beating rapidly and irregularly, blood does not flow through them as quickly. This makes the blood more likely to clot. If a clot is pumped out of the heart, it can travel to the brain, resulting in a stroke. People with atrial fibrillation are five to seven times more likely to have a stroke than the general population. Clots can also travel to other parts of the body (kidneys, heart, intestines), and cause other damage.
- Atrial fibrillation can decrease the heart’s pumping ability. The irregularity can make the heart work less efficiently. In addition, atrial fibrillation that occurs over a long period of time can significantly weaken the heart and lead to heart failure.
Symptoms
What are the symptoms of atrial fibrillation?
You may have atrial fibrillation without having any symptoms. If you have symptoms, they may include:
- Heart palpitations: Sudden pounding, fluttering or racing sensation in the chest
- Lack of energy or feeling over-tired
- Dizziness: Feeling light-headed or faint
- Chest discomfort: Pain, pressure or discomfort in the chest
- Shortness of breath: Having difficulty breathing during normal activities and even at rest
Treatments

How is atrial fibrillation treated?
The goals of treatment for atrial fibrillation include regaining a normal heart rhythm (sinus rhythm), controlling heart rate, preventing blood clots and reducing the risk of stroke.
Many options are available to treat atrial fibrillation, including lifestyle changes, medications, catheter-based procedures and surgery. The type of treatment that is recommended for you is based on your heart rhythm and symptoms.
Medications
Initially, medications are used to treat atrial fibrillation. Medications may include:
Rhythm control medications (antiarrhythmic drugs)
Antiarrhythmic medications help return the heart to its normal sinus rhythm or maintain normal sinus rhythm.
There are several types of rhythm control medications, including procainamide (Pronestyl), disopyramide (Norpace), flecainide acetate (Tambocor), propafenone (Rythmol), sotalol (Betapace), dofetilide (Tikosyn) and amiodarone (Cordarone).
You may have to stay in the hospital when you first start taking these medications so your heart rhythm and response to the medication can be carefully monitored. These medications are effective 30 to 60 percent of the time, but may lose their effectiveness over time. Your doctor may need to prescribe several different antiarrhythmic medications to determine the right one for you.
Some rhythm control medications may actually cause more arrhythmias, so it is important to talk to your doctor about your symptoms and any changes in your condition.
Rate control medications
Rate control medications, such as digoxin (Lanoxin®), beta-blockers [metoprolol (Toprol®, Lopressor®)], and calcium channel blockers such as verapamil (Calan®) or diltiazem (Cardizem®), are used to help slow the heart rate during atrial fibrillation. These medications do not control the heart rhythm, but do prevent the ventricles from beating too rapidly.
Anticoagulant medications
Anticoagulant or antiplatelet therapy medications, such as warfarin (Coumadin®), warfarin alternatives, or aspirin, reduce the risk of blood clots and stroke, but they do not eliminate the risk. Regular blood tests are required when taking Coumadin to evaluate the effectiveness of the drug. If you are taking warfarin alternatives, regular blood tests are not required. Talk to your doctor about the anticoagulant medication that is right for you.
Lifestyle Changes
In addition to taking medications, there are some changes you can make to improve your heart health.
- If your irregular heart rhythm occurs more often with certain activities, avoid those activities and tell your doctor. Sometimes, your medications may need to be adjusted.
- Quit smoking.
- Limit your intake of alcohol. Moderation is the key. Ask your doctor for specific alcohol guidelines.
- Limit the use of caffeine. Some people are sensitive to caffeine and may notice more symptoms when using caffeinated products (such as tea, coffee, colas and some over-the-counter medications).
- Beware of stimulants used in cough and cold medications, as some of these medications contain ingredients that may increase the risk of irregular heart rhythms. Read medication labels and ask your doctor or pharmacist what type of cold medication is best for you.
Procedures
When medications do not work to correct or control atrial fibrillation, or when medications are not tolerated, a procedure may be necessary to treat the abnormal heart rhythm, such as electrical cardioversion, pulmonary vein antrum isolation procedure, ablation of the AV node followed by pacemaker placement, surgical treatment (surgical ablation or maze procedure), or excision or exclusion of the left atrial appendage.
Electrical cardioversion: A cardioversion electrically “resets” the heart. Medications alone are not always effective in converting atrial fibrillation to a more normal rhythm. Sometimes cardioversion is used to restore a normal heart rhythm and allow the medication to successfully maintain the normal rhythm. Cardioversion frequently restores a normal rhythm, although its effect may not be permanent.
After a short-acting anesthesia is given that puts the patient to sleep, an electrical shock is delivered through patches placed on the chest wall. This shock will synchronize the heartbeat and restore a normal rhythm.
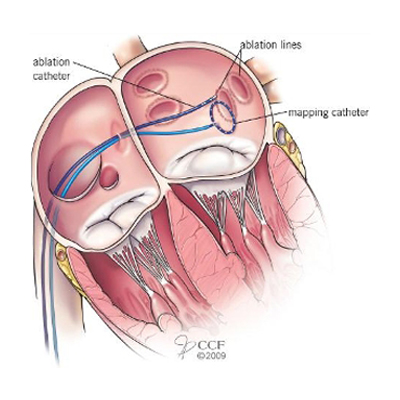
Pulmonary vein ablation: Pulmonary vein ablation (also called pulmonary vein antrum isolation or PVAI), may be an option for people who cannot tolerate medications or when medications are not effective in treating atrial fibrillation. PVAI is performed by an electrophysiologist (doctor who specializes in treating heart rhythm conditions).
Because atrial fibrillation usually begins in the pulmonary veins or at their attachment to the left atrium, energy is applied around the connections of the pulmonary veins to the left atrium during the pulmonary vein ablation procedure.
First, the doctor inserts catheters (long, flexible tubes) into the blood vessels of the leg, and sometimes the neck, and guides the catheters into the atrium. Energy is delivered through the tip of the catheter to the tissue targeted for ablation.
Frequently, other areas involved in triggering or maintaining atrial fibrillation are also targeted. Small circular scars eventually form and prevent the abnormal signals that cause atrial fibrillation from reaching the rest of the atrium. However, the scars created during this procedure may take from two to three months to form. Once the scars form, they block any impulses firing from within the pulmonary veins, thereby electrically “disconnecting” them or “isolating” them from the heart. This allows the SA node to once again direct the heart rhythm and a normal sinus rhythm is restored.
Because it takes several weeks for the lesions to heal and form scars, it is common to experience atrial fibrillation early during the recovery period. Rarely, atrial fibrillation may be worse for a few weeks after the procedure and may be related to inflammation where the lesions were created. In most patients, these episodes subside within one to three months.
Ablation of the AV node: Ablation of the AV node is another option for atrial fibrillation. During this type of ablation, catheters are inserted through the veins (usually in the groin) and guided to the heart. Radiofrequency energy is delivered through the catheter to sever or injure the AV node. This prevents the electrical signals of the atrium from reaching the ventricle. This result is permanent, and therefore, the patient needs a permanent pacemaker to maintain an adequate heart rate. Although this procedure can reduce atrial fibrillation symptoms, it does not cure the condition. Because the patient will continue to have atrial fibrillation, an anticoagulant medication is prescribed to reduce the risk of stroke.
Important note: Due to better treatment alternatives, AV node ablation is rarely used to treat atrial fibrillation.
Device Therapy
Permanent pacemaker: A pacemaker is a device that sends small electrical impulses to the heart muscle to maintain a suitable heart rate. Pacemakers are implanted in people with AF who have a slow heart rate. The pacemaker has a pulse generator (that houses the battery and a tiny computer) and leads (wires) that send impulses from the pulse generator to the heart muscle, as well as sense the heart’s electrical activity.
Newer pacemakers have many sophisticated features, designed to help with the management of arrhythmias and to optimize heart rate-related function as much as possible.
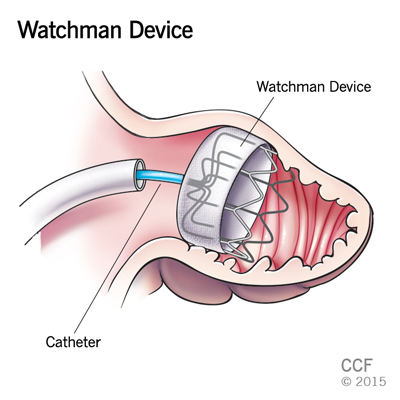
WATCHMAN™ device: The WATCHMAN device is a parachute-shaped, self-expanding device that occludes (plugs up) the left atrial appendage (LAA), which is a small, ear-shaped cavity located in the left atrium and in which clots tend to form in patients with atrial fibrillation. This device was tested in several studies that showed it was a good alternative treatment in patients with non-valvular atrial fibrillation and a history of bleeding who have an appropriate reason to seek alternative treatment to warfarin.
The WATCHMAN device is implanted percutaneously (through the skin) in the electrophysiology (EP) lab. The implant procedure does not require surgery; however, general anesthesia may be used during the procedure. A catheter sheath is inserted into a vein near the groin and guided across the septum (muscular wall that divides the right and left sides of the heart) to the opening of the LAA. The device is placed in the opening of the LAA. This seals off the LAA and keeps it from releasing clots.
The WATCHMAN device has been approved by the FDA to reduce the risk of thromboembolism from the LAA in patients with nonvalvular atrial fibrillation who:
- Are at increased risk of stroke and systemic embolism and for whom anticoagulation therapy is recommended
- Have physician approval to take warfarin
- Have an appropriate reason to want treatment with a non-medication alternative to warfarin, taking into account the safety and effectiveness of the device compared to warfarin
If you are interested in treatment with the WATCHMAN device, you can be evaluated by the electrophysiologists.
Surgical treatment
Certain patients are candidates for surgical treatment of atrial fibrillation. These include patients with one or more of the following characteristics:
- Other conditions requiring heart surgery
- Atrial fibrillation that persists after optimal treatment with medications
- Unsuccessful catheter ablation
- Blood clots in the left atrium
- History of stroke
- Enlarged left atrium
Maze procedure: During this procedure, a series of precise incisions or lesions are made in the right and left atria to confine the electrical impulses to defined pathways to reach the AV node. These incisions prevent the abnormal impulses from affecting the atria and causing atrial fibrillation.
The surgical maze procedure can be performed traditionally with a technique in which precise surgical scars are created in the atria. It may also be performed using newer technologies designed to create lines of conduction block with radiofrequency, microwave, laser, ultrasound or cryothermy (freezing). With these techniques, lesions and ultimately scar tissue is created to block the abnormal electrical impulses from being conducted through the heart and to promote the normal conduction of impulses through the proper pathway.
Many of these approaches can be performed with minimally invasive (endoscopic or “keyhole”) surgical techniques.
If a patient has atrial fibrillation and requires surgery to treat other heart problems (such as valve disease or coronary artery disease), the surgeon may perform the surgical treatment for atrial fibrillation at the same time.
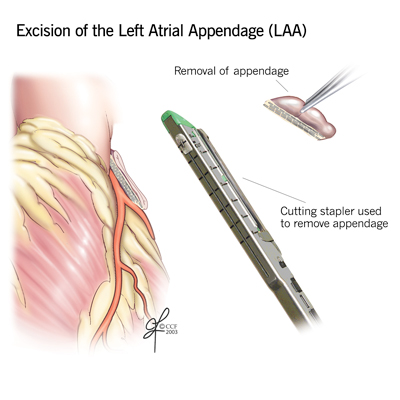
Excision or exclusion of the left atrial appendage: To prevent blood clots from forming, some patients may have a procedure to close off (exclude) the atrial appendage.
During surgical procedures to treat AF, the left atrial appendage can be removed and the tissue closed with a special stapling device, or it can be excluded with a device called AtriClip. The AtriClip is implanted from outside the heart and stops blood flow between the LAA and left atrium.
There are also several nonsurgical options to close the LAA and prevent blood clots.
AtriClip: LAA occlusion can benefit patients who need heart surgery and also have atrial fibrillation. The procedure is also helpful for those who have isolated atrial fibrillation and choose to have surgical ablation (maze procedure).
During surgery, the surgeon can either remove the LAA and sew the area closed or use a special device called the AtriClip*. The AtriClip is implanted from the outside of the heart and stops the flow of blood between the LAA and the left atrium.
*Disclosure: Cleveland Clinic has the potential to receive a royalty payment as a result of sale of the AtriClip.
If you would like to be evaluated to see if surgical closure of the LAA is the best treatment option for you, Cleveland Clinic surgeons can review your records.
Patient Services
MyChart
Cleveland Clinic’s MyChart® is a secure, online tool that connects you to portions of your electronic medical record from the privacy of your home. Utilize this free service to manage your healthcare at any time, day or night. With MyChart you can view test results, renew prescriptions, request appointments and more. You can also manage the healthcare of your loved ones with MyChart • Caregiver.
Participating in Research
Cleveland Clinic Florida is on the forefront of multiple, leading-edge research studies investigating the use of the latest catheter technologies, ablation protocols, and various imaging modalities for the catheter treatment of atrial fibrillation. We believe this proactive approach to electrophysiology research will advance and surpass the current medical therapy available for the treatment of atrial fibrillation.
During your visit at Cleveland Clinic Florida, you may be asked to enroll in one of these research studies. Please understand that participate or not participate will not affect your current or future medical care at Cleveland Clinic Florida.
To learn more about the current studies under the investigation and to learn about participating, please call 877.463.2010.
Appointments
To make an appointment with one of our heart specialists please call 877.463.2010 or you can request an appointment online.
Why Choose Us?
The Section of Cardiac Pacing & Electrophysiology at Cleveland Clinic in Florida is an integral component to the Heart and Vascular Institute located in Weston, Florida, as well as Cleveland Clinic’s Center for Atrial Fibrillation in Cleveland. The combined efforts of Cleveland Clinic’s specialists offer the most comprehensive treatment for patients with atrial fibrillation. Specialists from cardiology, cardiac surgery, cardiac imaging, emergency medicine and neurology combine their expertise to provide individual approaches for their patients.
When you visit the Heart and Vascular Institute, you will receive care from some of the leading specialists in the region utilizing the industry’s latest technology. Cleveland Clinic in Florida offers access to the most advanced electrophysiology laboratories including a hybrid operating room providing our specialists the ability to effectively treat atrial fibrillation.
