Why Choose Cleveland Clinic for Your Kidney Transplant
Established over 50 years ago, Cleveland Clinic’s kidney transplant program has completed thousands of kidney transplants, in conjunction with its affiliate program in West Virginia. Cleveland Clinic is recognized in the U.S. and throughout the world for its expertise and care. Our program is also a member of the United Network For Organ Sharing (UNOS), meeting all their requirements for kidney transplants. In 2021, Cleveland Clinic performed 306 kidney and kidney/pancreas transplants (Ohio program only)
Learn MoreKidney Transplant Program
Cleveland Clinic provides kidney transplant patients with world-class care and emotional support through the entire transplant process.
Interested in becoming a Living Donor?
Get started today by filling out our confidential online health questionnaire.
Learn MorePatient Stories
Man Benefits from HIV-Positive to HIV-Positive Kidney Transplant
Dec 1, 2022
“Although you may have HIV, there is still a chance for you. There are options for you. You can still get a kidney. You can still come get back to a normal life.”
Woman Has Transplant Because of Genetic Condition, Removes Six Pound Kidney
Mar 10, 2022
“I hope my story inspires others to consider being donors. That’s what it’s all about.”
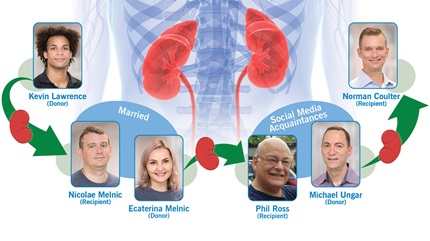
Three-Pair Kidney Swap is Transforming for Recipients and Donors
Sep 15, 2021
“You have the chance to save someone’s life or dramatically improve the quality of someone’s life. Dialysis is no way to live, and it’s actually puzzling to me that I waited so long to do this. It’s a big commitment, but it’s very safe.”