Shoulder Anatomy
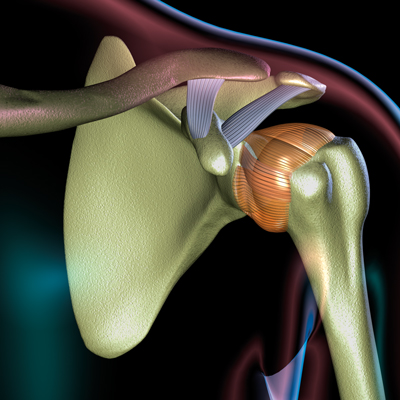
The shoulder is a large ball-and-socket joint. It is made up of bones, tendons, muscles and ligaments that hold the shoulder in place and also allow movement. The shoulder joint consists of the clavicle (collar bone), scapula (shoulder blade) and humerus (arm bone).
A group of muscles and tendons, known as the rotator cuff, stabilize the shoulder and hold the humerus within its shallow socket (the glenoid). Because of the complexity of muscles and ligaments and the lack of bony constraints, the shoulder is capable of extensive motion.
Types
Arthritis
Osteoarthritis is the wearing down of cartilage that allows bones to glide smoothly within the joints, and can occur with aging, trauma or overuse injury. Without cartilage, the bones in the shoulder begin to rub against each other, and growths called bone spurs can develop. Stiffness, swelling, pain and reduced range of motion can occur, along with a “catching” sensation in the joint.
Rheumatoid arthritis, a disorder of the immune system, produces chronic, painful inflammation of the joint’s lining, and eventual joint deterioration.
Severe osteoarthritis or rheumatoid arthritis in the shoulder may require joint replacement in the later stages.
Rotator Cuff
The rotator cuff consists of four muscles and cord-like tendons, tightly enclosed within the shoulder joint. Rotator cuff injuries are the most common causes of shoulder pain and activity restriction at all ages, and include:
Tendonitis — The mildest rotator cuff injury is tendonitis (tendon inflammation). Tendonitis can develop with repetitive overhead activities, such as playing tennis, pitching, raking, shoveling or painting. Tendonitis also can arise secondarily from joint degeneration due to osteoarthritis. It produces pain like a toothache radiating through the upper arm that can awaken you from sleep. Reaching overhead or behind your back is painful. Tendonitis is the most common cause of shoulder pain.
Tear — A torn rotator cuff, sometimes called “pitcher’s shoulder” or “tennis shoulder,” is very common and almost half of people will have a tear in their lifetime, sometimes without much pain. The rotator cuff tendons can split or tear suddenly with injury, or slowly by rubbing against bone spurs. Untreated tears can weaken the arm, make it difficult to raise it and visibly shrink muscles. Pain occurs during motion and also at night.
Bursitis
Bursitis, which typically accompanies rotator cuff tendonitis, involves painful inflammation of the bursa (the fluid-filled sac that surrounds the rotator cuff and provides lubrication and protection from the overlying bony shoulder tip, called the scapular acromion). Bursitis is most often caused by repetitive motions (overuse), or repeatedly bumping or putting pressure on the area. Less often, bursitis is caused by a sudden, more serious injury.
Impingement syndrome
Swelling and inflammation of tendons and/or bursa can place undue pressure on tendons as they pass between the upper arm bone and the shoulder tip. In its cramped space, blood flow to the swollen tendon is reduced, and it begins to fray. This syndrome is characterized by bursitis, inflammation, sometimes tearing of the rotator cuff, bone spur formation and limiting range of motion.
Symptoms include discomfort and, sometimes, acute shoulder pain when raising the arms above the head, reaching into a back pocket or while sleeping on the affected shoulder. People who frequently work with their arms above their heads may be more likely to get shoulder impingement syndrome.
Instability
When the ball (humeral head) moves or is pushed off the socket (glenoid) the shoulder becomes unstable and is at risk for partial or complete dislocation. Recurrent dislocations cause pain and unsteadiness when raising the arm or moving it away from the body, and a feeling that the shoulder is “slipping out of place” when reaching overhead.
Labral Tears
Your labrum is a cartilage cuff around the socket that encircles the head of the upper arm bone (humerus) to hold it within its shallow bony socket. This cartilage can tear with injury to the shoulder. The labrum becomes more brittle with age and thus susceptible to fraying. The long head of the biceps tendon attaches to the labrum and sometimes detaches the labrum. Tears cause aching in the shoulder, “catches” in the shoulder when moved, and pain with some activities, which may signal a torn labrum.
Frozen shoulder
Between ages 40 and 60, the joint capsule surrounding the shoulder can become inflamed or shrink, making movement painful and stiff. Reluctance to use the shoulder brings increasing stiffness, restricted motion and a persistent, dull aching. Initial severe pain fades after several months, but the shoulder becomes “frozen” and may take two to three years to “thaw” without treatment. Treatment is directed at pain relief until the acute phase passes, followed by therapy and even surgical intervention to regain motion if it does not return spontaneously.
Other causes
Less common causes of shoulder pain include infection (osteomyelitis), soft-tissue or bone tumors and nerve problems. A shoulder specialist can help pinpoint the reason. When shoulder pain is intense, it’s important to seek help promptly.
Diagnosis

If you develop shoulder pain that persists, specialists at Cleveland Clinic can help sort out the possible causes. When diagnosing any shoulder pain, the physician will take your medical history and perform a thorough physical examination, which are the cornerstones for an accurate diagnosis.
To help your doctor best understand your shoulder pain, you’ll need to provide the following information: A description of your pain, including:
- Where the pain is located and when it occurs
- When the pain started and if it is the result of an injury or accident
- Description of pain (dull, stabbing, throbbing)
- Anything that makes the pain worse or better
- Any medication you’re taking and medication allergies
Your doctor also may order imaging tests to view the joint, which may include:
X-rays — X-rays can show if there are bone changes within your shoulder.
MRI — If an X-ray looks normal, your doctors may order a magnetic resonance imaging (MRI) scan. An MRI uses magnets and radio waves to provide detailed images of soft tissues, including muscle, tendon and ligaments.
CT scan — A computerized tomography (CT) scan shows fine detailed, cross-sectional and 3-D images of bony abnormalities and to a lesser degree tendon problems. It is best used to evaluate issues with the bones and often obtained for pre-surgical planning purposes and decision making.
Ultrasound – Ultrasound is a non-invasive test that gives physicians a real-time view of the surrounding muscles and tendons of the shoulder. Plus, it does not expose patients to radiation and may be a good alternative for patients who may be unable to get an MRI or CT scan. It is best for rotator cuff issues.
Treatments

Most shoulder problems do not require surgery and are best treated with a directed physical therapy program, often with the help of anti-inflammatory medications, and at times cortisone (corticosteroid) injections. However, when necessary, our specialists are highly skilled in the latest techniques of arthroscopic surgery and total shoulder joint replacement.
Non-operative care — Most shoulder problems can be resolved with non-operative treatments such as:
Rest — When your shoulder hurts, it’s important to rest it. Refrain from reaching upward, carrying heavy objects and doing repetitive motions. Pain and inflammation will not subside if repetitive activities (such as vacuuming, raking or car-washing) continue to stress the sore shoulder. However, some movement is important.
Ice and heat — Icing the shoulder with cold packs (or bags of frozen peas or corn) when pain is severe reduces inflammation, swelling and discomfort. Apply ice for 15 to 20 minutes, three to four times each day.
Heat can also help chronic shoulder conditions. Try taking hot showers and doing recommended stretches first thing in the morning. Or, you can alternate ice and heat (taking at least a 40-minute break between each) to get the benefits of both.
Physical therapy — Orthopaedic and rheumatologic specialists can prescribe physical therapy to help you recover from a shoulder condition or injury. Physical therapists tailor range-of-motion exercises to increase flexibility in the shoulder. They also will show you strengthening exercises that help prevent muscle shrinkage, and good body mechanics to help you avoid shoulder strain.
Over-the-counter medications - Shoulder pain can be often relieved with over- the- counter- medications including non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil®) or naproxen (Aleve®), and anti-analgesia (pain-relieving) medications such as acetaminophen (Tylenol®). There are also some topical creams and ointments such as Volaren® that provide temporary numbing relief.
Prescription medications - If over-the-counter medications don't provide relief, prescription-strength NSAIDs can be prescribed. Opioid medications are rarely ever prescribed except in the early post-surgical period or in the setting of a significant fracture, as opioids are not very helpful outside of these two scenarios.
Injections — When other treatments don’t help severe shoulder pain, cortisone injections may temporarily help to “settle down” inflamed tissues within the joint, reducing pain. Your physician will review the risks and benefits with you.
Nerve blocks (or injecting anesthetics) — Can also be done by anesthesiologists for conditions, such as a frozen shoulder, to allow for more aggressive physical therapy.
Surgical Options

When shoulder problems do not respond to non-operative care, your physician may recommend surgery. Options range from minimally invasive arthroscopic surgery to total shoulder replacement.
Shoulder arthroscopy
In arthroscopic surgery, only a few small incisions are required, making recovery quicker and less painful than with an open approach. A viewing camera is inserted through one incision, and slender telescopic instruments are inserted through others. This allows surgeons to inspect and repair labral tears and rotator cuff tears, and remove spurs and bony growths to enable inflamed, cramped tendons to move more freely. They can also remove thickened, inflamed bursa and bone to create space around the rotator cuff and relieve painful impingement and can cut through tight sections of the joint capsule to release a frozen shoulder.
Arthroscopic surgery can be combined with standard “open” surgery when a larger incision is required to properly view and repair a more complex problem.
Recovery
Arthroscopy is usually an outpatient procedure. You may need pain medication during the first few days to a week, and it is typically recommended to resume light activities at waist height after a few days. Most patients recover completely and return to work or normal activities within one week to three months following the procedure. After about four to six weeks, you will start to strengthen the shoulder again. Most patients achieve their maximum improvement over three to six months. Some patients may require more time.
Benefits
This procedure improves function and decreases pain.
Who is a candidate?
Your orthopaedic surgeon will determine if you are a candidate based on your level of pain, disability and overall health.
Risks
All surgery entails some degree of risk, but the risk associated with this type of surgery is quite low. Some of the risks you should be aware of include infection, wound healing problems, bleeding and injury to nerves, blood vessels and the joint surface of the shoulder. Occasionally, patients can develop a “frozen shoulder” after the operation.
Open shoulder surgery
In some cases, your surgeon may determine that a traditional, open surgery is necessary. An incision is made on the shoulder to access the structures that need to be repaired, reattached or tightened.
Recovery
The recovery from open surgery depends on the type of procedure that was performed. Open surgery may be performed as either an outpatient procedure or require an overnight hospital stay. You will likely need pain medication for the first few days or a week following the procedure. You will begin to move your wrist, hand and elbow the day after surgery, with a physical therapy program for shoulder movement beginning about a week after surgery. Strength will return to the shoulder in about three months. Full recovery may take up to six months to a year.
Benefits
This technique is critical and necessary for access to certain ligaments and tendons in complex cases. In certain instances, an open repair may provide a better outcome than an arthroscopic procedure.
Who is a candidate?
Open procedures may be recommended when an injury is large or complex, or when the surgeon believes the results will be better than with arthroscopy. This type of repair is often required to treat severe or recurrent shoulder instability.
Risks
The risks associated with open shoulder surgery and joint replacement are quite low, and not greater than with arthroscopic procedures. Possible problems that may arise include infection, damage to surrounding nerves and blood vessels. Your medical team will closely monitor you for any signs of these complications. Rarely, patients can develop a “frozen shoulder” after the operation.
Shoulder Replacement Options
Shoulder replacement is similar in concept to knee replacement and hip replacement. When arthritis has damaged the shoulder joint, it may be replaced with a metal ball and plastic socket. Shoulder replacements have been performed since the 1950s. When the procedure is done well, a motivated patient can often return to such activities as golf, swimming and tennis.
Hemiarthroplasty
Hemiarthroplasty is essentially half a replacement. In this procedure, a surgeon may opt to only replace the ball of the shoulder joint for conditions that affect the ball and not the socket. The ball is the rounded head of the humerus, or arm bone, which rests against the socket (glenoid) in the shoulder blade. Studies show that patients suffering from osteoarthritis may see better results from total shoulder arthroplasty.
Recovery
Patients will begin supervised movement of their shoulder joint following surgery. You will likely need oral pain medication for at least several days. Most patients return home after one day in the hospital. You will need to wear a sling for up to six weeks following surgery. For the first six weeks, typically patients are able to use their hands at waist level but will not be permitted to drive. Physical therapy is key to recovery and regaining mobility. Functional recovery is present at three months, and full recovery may take up to a year.
Benefits
Compared to a full shoulder joint replacement, hemiarthroplasty preserves the normal glenoid (socket). Patients who have hemiarthroplasty are also still candidates for a full shoulder replacement, if needed, down the road. The type of hemiarthroplasty can vary based on how the metal ball is held into the bone of the humerus, with stemmed (standard or short stems), stemless, and resurfacing implants available. Stemless and resurfacing implants preserve more of the bone of the humerus and are alternatives to traditional stemmed shoulder replacement for certain patients. They can also make an easier transition to a total replacement, if needed, by preserving more bone.
Who is a candidate?
If a patient’s shoulder socket is normal and only the head of the upper arm bone, or humerus, has a severe injury, surgeons may recommend this option. The procedure may be recommended for young or very active patients because it avoids the risks of component wear and loosening that may occur with total shoulder replacements.
Other conditions that may warrant hemiarthroplasty are avascular necrosis (bone cell death) caused by interrupted blood supply, post traumatic arthritis or inadequate bone to place an artificial socket.
Risks
Possible (but rare) complications of surgery include blood clots, infection, nerve damage and other risks. Long-term complications may include continued pain, infection, loosening or dislocation of the prosthesis.
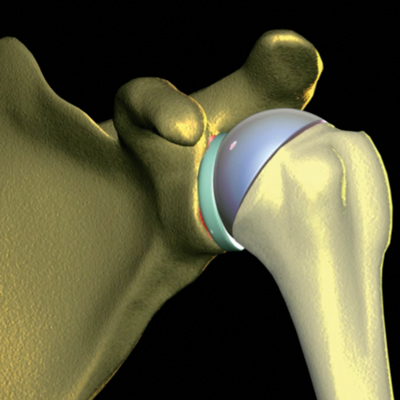
Total Shoulder Replacement
This is an option (total joint replacement) for patients who suffer from wear on both sides of the joint. In a total shoulder replacement, a metal ball is used to replace the humeral head while a polyethylene disc becomes the replacement of the glenoid socket.
Recovery
You can expect to stay in the hospital for 1-3 days following your surgery. Physical therapy is a critical component of a successful surgery. The first day after surgery, you will be beginning physical therapy and you will become increasingly comfortable with use of the arm as the weeks progress. Your physician will ensure that you have adequate pain medication to be comfortable and to be able to perform therapy. Patients should be able to dress and feed themselves within the first week. Patients should exercise care in driving and only resume doing so when they can handle the vehicle safely. Sports activities may resume after about six to eight months.
Benefits
The primary goal of total shoulder replacement surgery is to alleviate pain with secondary goals of improving motion, strength and function. The type of total shoulder replacement can also vary based on how the metal ball is held into the bone of the humerus, with stemmed (standard or short stems), stemless, and resurfacing implants available. Stemless and resurfacing implants preserve more of the bone of the humerus and are alternatives to traditional stemmed shoulder replacement in certain patients.
Who is a candidate?
Total shoulder replacement is most frequently considered for patients who have osteoarthritis, rheumatoid arthritis and, more rarely, for those who have sustained severe trauma from a shoulder fracture. A physician will exhaust all reasonable non-surgical alternatives of management before contemplating a joint replacement.
Risks
As with any surgery, risks of infection, nerve and vessel injury, bleeding and wound healing problems do exist, but they occur infrequently. Nursing and medical staff will check the arm frequently to ensure that any problems are identified and treated properly, should they arise. A replacement joint may eventually become worn and the components loosened, or even dislocated. In such cases, a revision procedure may be necessary.
Reverse Total Shoulder Replacement
Another type of shoulder replacement is called reverse total shoulder replacement. That means a metal ball is attached to the native socket, and a plastic socket is attached to the upper arm bone where the ball was natively. This allows the patient to use the deltoid muscle instead of the torn rotator cuff to lift the arm.
Recovery
Most patients can eat and return to mobility within a day of surgery, and go home – wearing a sling within 1-3 days. The sling may be used for comfort for up to four weeks. Physical therapy often starts shortly after surgery and will help patients regain their strength and flexibility, but is much simpler that a traditional total shoulder arthroplasty.
Rehabilitation will include exercises to be done at home. Be sure to contact your physician if pain interferes with physical therapy.
Benefits
Reverse shoulder replacement is a good solution for patients, such as those with irreparable rotator cuff tears plus arthritis, whose conditions cannot be solved by a standard shoulder replacement.
Who is a candidate?
People who have an unsuccessful shoulder replacement, significant rotator cuff tearing and arthritis, or severe arm weakness because of totally torn rotator cuffs may be considered for the procedure. Regular shoulder replacement is not advised for the patients who have a torn rotator cuff.
Risks
Infection is possible, though infrequent, in the wound itself or near the prosthesis. A replacement joint may become worn and the components loosened, or even dislocated. In such cases, a revision procedure may be necessary. A more rare complication could involve nerve damage surrounding the surgery area. This type of damage is known to heal with time.
Patient Services
MyChart
MyChart is a secure online tool that provides personalized health information from the privacy of your home at any time, day or night. Learn more or login now.
Virtual Second Opinion
If you cannot travel to Cleveland Clinic, help is available. You can connect with Cleveland Clinic specialists from any location in the world via a phone, tablet, or computer, eliminating the burden of travel time and other obstacles. If you’re facing a significant medical condition or treatment such as surgery, this program provides virtual access to a Cleveland Clinic physician who will review the diagnosis and treatment plan. Following a comprehensive evaluation of medical records and labs, you’ll receive an educational second opinion from an expert in their medical condition covering diagnosis, treatment options or alternatives as well as recommendations regarding future therapeutic considerations. You’ll also have the unique opportunity to speak with the physician expert directly to address questions or concerns.
Virtual Visits with Orthopaedics
New patients with common knee injuries or knee pain.
Established patients scheduling follow-up care appointments such as:
- Post-Surgical & wound check visits
- Fracture care follow-up
- Injection follow-up
- Musculoskeletal injury follow-up
- Per-operative teaching prior to surgery
If you would like to use Express Care Online for your next visit, please call your provider’s office. If you are eligible, our team will schedule your virtual visit and provide details on the cost of your appointment and setup instructions.
Appointments
To make an appointment with a shoulder specialist, call:
- Cleveland Appointments: 216.444.2606
- Akron Appointments: 330.344.2663
- Canton Appointments: 330.489.1362
- Dover Appointments: 330.343.3335
Why Choose Us?
At the Orthopaedic & Rheumatologic Institute, we offer patients the most advanced treatments for any type of shoulder pain. Our institute uses a multidisciplinary team approach, bringing all of the experts that you need together under one roof, including orthopaedic physicians and surgeons, rheumatologists and physical therapists.
Being part of Cleveland Clinic also means you have easy access to any of our other specialists to manage any related conditions. Our experienced team works closely together and helps develop an individualized plan to best meet your needs. You also can take comfort in knowing that our physicians remain the experts at the forefront of developing new approaches to treating shoulder pain.