What is the Pancreas?
The pancreas is a dual-function, glandular organ located between the stomach and spine and next to the upper part of the small intestine (duodenum). Approximately six inches in length, this thin, pear-shaped organ is part of both the endocrine and digestive systems.
The large end of the pancreas is called the head, the middle section the body, and the thin end the tail. The pancreas produces juices that contain enzymes and hormones. The main functions of the pancreas are to:
- Secrete enzymes into the small intestine to help digest carbohydrates, proteins, and fat
- Release the hormones insulin and glucagon into the bloodstream to help regulate blood sugar
Types of Pancreatic Disease

What are the different types of pancreatic diseases?
The most common pancreatic diseases treated at Cleveland Clinic’s Pancreas Clinic include acute pancreatitis, chronic pancreatitis and pancreatic cancer.
Pancreatitis
Pancreatitis is a painful inflammation of the pancreas. Pancreatic damage occurs when digestive enzymes attack the pancreas. In severe cases, pancreatitis can cause loss of blood flow to the gland, leading to serious tissue damage, infection and cyst formation.
Severe pancreatitis can cause damage if enzymes and toxins are released into the bloodstream and harm other vital organs, such as the heart, lungs and kidneys. Typically, pancreatitis develops gradually and becomes progressively worse. There two forms of pancreatitis: acute and chronic.
Acute pancreatitis is a sudden inflammation of the pancreas that occurs over a short period of time. More than 80 percent of acute pancreatitis cases are caused by heavy alcohol use or gallstones. In the latter case, gallstones passing from the gallbladder can become lodged at the ampulla (opening to the ducts that drain the gallbladder and pancreas). This blockage causes an obstruction of the pancreatic duct. Pancreatic juices can then back up into the pancreas and lead to acute pancreatitis.
Symptoms of acute pancreatitis range from mild abdominal discomfort to a severe, life-threatening illness.
Other less common causes of acute pancreatitis include:
- Altered pancreatic anatomy
- Medications
- Infections
- Trauma
- Metabolic disorders
- Autoimmune disease
In approximately 10 percent of cases, the cause of acute pancreatitis is unknown.
Chronic pancreatitis it is the result of ongoing inflammation of the pancreas and often occurs after multiple episodes of acute pancreatitis. In some cases, chronic pancreatitis is caused by prolonged, heavy alcohol use but it can also be caused by metabolic or genetic disorders. Though rare, chronic pancreatitis may run in families (hereditary pancreatitis).
Symptoms of Pancreatitis
What are the symptoms of pancreatitis?
Most patients with acute pancreatitis experience upper abdominal pain that spreads to the back. Often described as a deep “boring” sensation, the pain is aggravated by eating and slowly worsens. Swollen and tender abdomen, nausea, sweating, vomiting, fever, and increased heart rate are other signs of acute pancreatitis.
Diagnosis of Pancreatitis

How is pancreatitis diagnosed?
In most cases, acute pancreatitis is suspected when a patient has the abovementioned symptoms coupled with risk factors, such as heavy alcohol use or gallstone disease. Measuring levels of amylase and lipase in the blood can confirm a pancreatitis diagnosis. High levels of these two enzymes strongly suggest acute pancreatitis.
In general, chronic pancreatitis is suspected when a patient has abdominal pain compounded by risk factors such as:
- Heavy and prolonged alcohol use (can cause pancreas damage or scarring)
- Hereditary conditions
- Conditions such as high triglycerides or high calcium levels
- Tropical pancreatitis
- Pancreas divisum (two pancreas ducts rather than one, present at birth)
Diagnosing chronic pancreatitis can be difficult because its symptoms are similar to those of other conditions, like ulcer, gallstones, irritable bowel syndrome and pancreatic cancer. Cleveland Clinic specialists rely on a number of new diagnostic techniques — including pancreatic function tests and imaging of the pancreas gland with a CT scan or EUS — for accurate, chronic pancreatitis diagnoses. The Pancreas Clinic at Cleveland Clinic is one of a few healthcare facilities in the United States using endoscopic pancreatic function testing for diagnosing earlystage pancreatitis.
Understanding Diagnostic Tests
The Pancreas Clinic offers state-of-the-art diagnostic tests available, including:
Abdominal ultrasound – Detects gallstones and fluid from inflammation in the abdomen (ascites). Ultrasound can also show an enlarged common bile duct, an abscess, or a pseudocyst (a collection of tissue, fluid and pancreatic enzymes).
Computed tomography (CT) – Can help rule out other abdominal pain causes and determine if tissue is dying. CT can identify complications (fluid around the pancreas, abscess or pseudocyst.)
Endoscopic retrograde cholangiopancreatography (ERCP) – A tube is placed down the throat, into the stomach, then into the small intestine. Dye helps the doctor view the bile and pancreatic ducts on an X-ray.
Endoscopic ultrasound - A scope is inserted down the throat into the stomach. Sound waves show abdominal organs and may reveal gallstones. Endoscopic ultrasound can help diagnose chronic pancreatitis when an invasive test might exacerbate the condition.
Fecal elastase test – Measures elastase (an enzyme found in the pancreas) in a stool sample to test how well the pancreas works.
Magnetic resonance cholangiopancreatography – A type of MRI used to view bile ducts and the pancreatic duct.
Secretin pancreatic function test - Measures the ability of the pancreas to respond to the hormone secretin.
Treatments of Pancreatitis
How is pancreatitis treated?
Most people suffering from acute pancreatitis require hospitalization, intravenous fluids and pain medication. For the 20 percent of patients who experience severe symptoms, admittance to an intensive care unit (ICU) is necessary. Severe pancreatitis can lead to loss of blood flow, causing infection, fluid collections, and damage to the heart, lungs or kidneys.
Some cases of severe pancreatitis cause death of pancreatic tissue (necrosis). In these cases, surgery may be necessary to remove the damaged pancreatic tissue. Despite the severity of the symptoms, 80 percent of patients diagnosed with acute pancreatitis recover completely.
At the Cleveland Clinic’s Pancreas Clinic, patients with acute pancreatitis benefit from the latest in endoscopic, minimally invasive and radiographic imaging for diagnosis and treatment of pancreatic inflammation.
Just as chronic pancreatitis can be difficult to diagnose, it can be somewhat difficult to treat. Doctors will try to relieve the patient’s pain and improve nutritional and metabolic problems that result from loss of pancreatic function.
Patients with chronic pancreatitis may be prescribed:
- Pancreatic enzymes (taken at meals to help nutrient absorption)
- Pain medications
- Vitamin supplements
- Small, frequent meals
In addition to the above medical intervention, endoscopy or surgery may be necessary to:
- Relieve abdominal pain
- Restore drainage of pancreatic secretions
- Treat chronic pancreatitis caused by blockage of the pancreatic duct
- Reduce the frequency of pancreatitis attacks
- Perform pain blocks
Cleveland Clinic is one of a handful of centers performing total pancreatectomy and islet transplant for selected patients with chronic pancreatitis with no other surgical options.
Pancreatic Cancer

Pancreatic cancer is the tenth most common cancer in the United States. It is also the fourth deadliest. Approximately 37,000 people in the U.S. are diagnosed with pancreatic cancer annually.
Pancreatic cancer is a malignant disease that starts in the ductal cells of the pancreas. The disease occurs when cells in the pancreas grow, divide, and spread uncontrollably, forming a malignant tumor. In addition to cancerous tumors, there also are a variety of benign (noncanceroous) tumors that can develop in the pancreas.
Pancreatic cancer is known to spread silently, so in most cases, symptoms do not present themselves until the disease is in an advanced stage. Unfortunately, by this point, treatment options are limited.
Symptoms of Pancreatic Cancer

What are the symptoms of pancreatic cancer?
Pancreatic cancer is known to spread silently, so in most cases, symptoms do not present themselves until the disease is in an advanced stage. Unfortunately, by this point, treatment options are limited. These symptoms often include:
- Jaundice (a yellowing of the skin and/or whites of the eyes)
- Upper abdominal pain that can radiate to the back
- Weight loss
- Nausea
- Vomiting
- Weakness and fatigue
- New onset of diabetes in an otherwise healthy person
Some patients may experience additional, subtle symptoms including:
- Dark urine or light-colored stools
- Abdominal bloating
- Feelings of fullness with less-than-normal food intake
- Diarrhea
Who is at risk for pancreatic cancer?
Though the exact cause of pancreatic cancer is unknown, several factors increase an individual’s changes of developing the disease:
- Smoking (smokers are three to four times more likely to develop pancreatic cancer)
- Chronic pancreatitis
- Age (80 percent of pancreatic cancer occurs in people over age 50)
- Gender (more common in males)
- Family history (rare)
Pancreatic cancer cannot be prevented, but the odds of developing the disease are reduced significantly by not smoking, maintaining a healthy weight and eating a plant-based diet.
Diagnosis of Pancreatic Cancer
How is pancreatic cancer diagnosed?
Once a patient history and physical exam are complete, imaging tests may be performed to help diagnose pancreatic cancer. Tumors may be visible on radiographic imaging, such as a CT (computed tomography) scan or MRI (magnetic resonance imaging).
If scans do not reveal a tumor, but one is suspected, more invasive imaging, such as endoscopic ultrasound, may be used. For a definitive diagnosis of pancreatic cancer, a biopsy may be performed at the time of EUS.
Types of Pancreatic Cancer
Pancreatic cancer is classified by the specific part of the pancreas that is affected: the part that makes digestive secretions (exocrine) or the part that makes insulin and other hormones (endocrine).
Exocrine pancreatic cancer - Cancer that forms in the pancreas ducts, called adenocarcinoma. Because the exocrine pancreas makes up 95 percent of the pancreas, the majority of pancreatic cancers (95 percent) are adenocarcinomas. Sometimes these cancers are called exocrine tumors.
Other, less common, exocrine pancreatic cancers include adenosquamous, squamous cell, giant cell and acinar cell carcinomas.
Endocrine pancreatic cancer - A rare cancer that forms in the hormone-producing cells of the pancreas (also called islet cells or islets of Langerhans). Cancer arising from one of these cells is called neuroendocrine pancreatic cancer or islet cell cancer. Some of these tumors are called nonfunctional because they are not hormonally active. Others secrete hormones and are named based on the hormones they produce (such as gastrinoma, insulinoma, etc.)
Treatments of Pancreatic Cancer

Types of Pancreatic Cancer
Pancreatic cancer is classified by the specific part of the pancreas that is affected: the part that makes digestive secretions (exocrine) or the part that makes insulin and other hormones (endocrine).
Exocrine pancreatic cancer - Cancer that forms in the pancreas ducts, called adenocarcinoma. Because the exocrine pancreas makes up 95 percent of the pancreas, the majority of pancreatic cancers (95 percent) are adenocarcinomas. Sometimes these cancers are called exocrine tumors.
Other, less common, exocrine pancreatic cancers include adenosquamous, squamous cell, giant cell and acinar cell carcinomas.
Endocrine pancreatic cancer - A rare cancer that forms in the hormone-producing cells of the pancreas (also called islet cells or islets of Langerhans). Cancer arising from one of these cells is called neuroendocrine pancreatic cancer or islet cell cancer. Some of these tumors are called nonfunctional because they are not hormonally active. Others secrete hormones and are named based on the hormones they produce (such as gastrinoma, insulinoma, etc.)
What are the treatment options for pancreatic cancer?
Treatment is based on how far the cancer has spread and generally includes the following options:
Surgical Treatment
Surgery is still considered the “gold standard” treatment for cancer that has not spread outside the pancreas. Removing the tumor and surrounding tissue gives the best chance for cure for patients whose disease is localized.
Your surgeon will determine whether a tumor is resectable (removable). Experience is critical to properly planning surgery and making sure that an appropriate treatment strategy and operation is chosen.
Depending on the patient and their tumor, minimally invasive surgery (including laparoscopic and robotic surgery) is offered at Cleveland Clinic.
How much tissue will be removed and what type of surgical approach will be used depends on where the tumor is located, its size, patient’s body type/weight and any previous surgeries. Surgical resection of pancreatic cancer is generally performed as:
- Pancreaticoduodenectomy – A pancreaticoduodenectomy (or Whipple procedure) is the most common surgical treatment for cancerous or benign tumors of the head of the pancreas. The procedure involves removal of the gallbladder, bile duct, part of the stomach and duodenum, and the head of the pancreas.
- Distal pancreatectomy – This surgical option is used for cancers in the pancreatic tail and body. The procedure removes the tail of the pancreas, sometimes along with a small portion of the pancreatic body.
Medical Treatment
Medical treatment, including chemotherapy and radiation therapy, is often used to complement surgical treatment. It may be used before or following surgery, or when the tumor is advanced to extend life, if possible, or improve symptoms.
Cleveland Clinic Cancer Center Institute doctors and nurses who specialize in cancer treatment can suggest ways to make side effects more manageable and to help relieve symptoms that may occur during and after procedures.
Chemotherapy is the use of drugs that are designed to kill rapidly growing cells such as cancer cells. Chemotherapy may be injected directly into a vein (by IV, or intravenously) or given through a catheter, which is a thin tube placed into a large vein and kept there until it is no longer needed. Some chemotherapy drugs are taken by pill.
This treatment affects both normal cells and cancer cells. Your doctors will try to prevent side effects as much as possible while treating the cancer appropriately. Side effects depend largely on the specific type of drug and the amount given. They can be different for each person and may only be temporary. Common side effects of chemotherapy include nausea and vomiting, hair loss, mouth sores and fatigue.
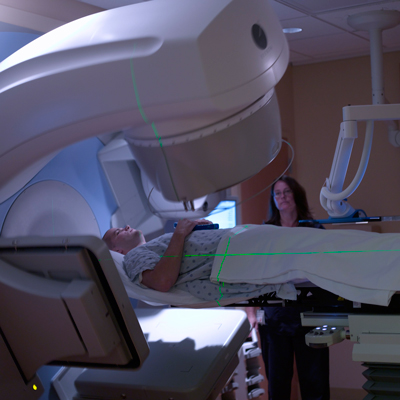
Radiation therapy is a form of high energy X-ray that kills cancer cells. It is often used in conjunction with chemotherapy before or after surgery, and in cases where the cancer is limited to the pancreas. Treatment with radiation and chemotherapy is aimed at sterilizing cancer cells before an anticipated surgical resection, called neoadjuvant therapy. Treatment with chemoradiation to reduce the size of the tumor is rarely successful.
Radiation therapy is a “focused” treatment, meaning it is designed to maximize its effect on the cancer cells while minimizing any injury to normal cells. Radiation to treat pancreatic cancer most often comes from a machine (external radiation).
Patients may notice some skin changes in the area exposed to radiation. The skin may become red, warm and sensitive — as if with a sunburn. It may also become darker and appear tanned. It may peel or become moist and tender. Depending on the dose of radiation given receive, there may be a loss of hair or decreased perspiration within the treated area.
These skin reactions are common and temporary they will subside gradually within two to four weeks of completing treatment.
What are the treatment options for islet cell tumors?
Different types of treatments are available for patients with islet cell tumors, or cancer that forms in the hormone-producing cells (islet cells) of the pancreas. Some treatments are standard and some are being tested in clinical trials. Generally, five types of standard treatments are used:
- Surgery – Types include enucleation, Whipple procedure, distal pancreatectomy, total gastrectomy, liver resection, radiofrequency ablation, or cryosurgical ablation
- Chemotherapy – Drugs that kill cancer cells
- Hormone therapy – Injections of hormones can help relieve symptoms
- Hepatic arterial occlusion or chemoembolization – This treatment is not targeted at the primary tumor, but for cases when the cancer has spread to the liver. It employs drugs or other agents to block or reduce blood flow to liver through hepatic artery to kill the cancer cells growing in liver. Chemotherapy delivered during this procedure is called chemoembolization.
Clinical Trials
For some patients, participating in a clinical trial may be the best treatment choice. Clinical trials are done to find out if new cancer treatments are safe and effective, or to see if they are better than the standard treatment. Many of today’s standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move medical knowledge forward.
Patient Services
Making Your Care Easier
Cancer Answer Line
If after reviewing this guide, you have additional questions, Cleveland Clinic’s Cancer Answer Line can help. Two oncology clinical nurse specialists and their staff can provide information and answer questions about cancer. The Cancer Answer Line is operational from 8 a.m.- 4:30 p.m., Monday - Friday. Please call toll-free 866.223.8100.
Patient Resource Center
If your care brings you to Cleveland Clinic Cancer Center, please visit the Patient Resource Center in the northeast corner of the building. It is a place for patients, their friends and families to come for cancer information.The Patient Resource Center is open from 8 a.m. to 5 p.m., Monday – Friday.
Medical Concierge
If you are traveling from out of state and need any assistance, call the complimentary Medical Concierge at 800.223.2273, ext. 55580, or email medicalconcierge@ccf.org.
MyChart
This secure online tool connects patients to their own health information from the privacy of their home any time, day or night. Some features include renewing prescriptions, reviewing test results and viewing medications, all online. For the convenience of physicians and patients across the country, MyChart now offers a secure connection to Google™ Health. Google Health users can securely share personal health information with Cleveland Clinic, and record and share the details of their Cleveland Clinic treatment with the physicians and healthcare providers of their choice.
Appointments & Locations
Making an Appointment
To make an appointment with any of our experts at Cleveland Clinic’s Pancreas Clinic, call one of the following locations:
- Cleveland: 216.445.8319
- Akron: 330.344.5487
Cancer Care Locations
Cleveland Clinic Cancer Specialists are located in Cleveland, regionally throughout Northern Ohio and in Florida. View a complete list of cancer care locations.
Virtual Second Opinion
If you cannot travel to Cleveland Clinic, help is available. You can connect with Cleveland Clinic specialists from any location in the world via a phone, tablet, or computer, eliminating the burden of travel time and other obstacles. If you’re facing a significant medical condition or treatment such as surgery, this program provides virtual access to a Cleveland Clinic physician who will review the diagnosis and treatment plan. Following a comprehensive evaluation of medical records and labs, you’ll receive an educational second opinion from an expert in their medical condition covering diagnosis, treatment options or alternatives as well as recommendations regarding future therapeutic considerations. You’ll also have the unique opportunity to speak with the physician expert directly to address questions or concerns.
Why Choose Us?
Why Choose Cleveland Clinic?
As the nation’s rate of pancreatic disease continues to climb, Cleveland Clinic’s Pancreas Clinic rises to the challenge of diagnosing and treating pancreas-related diseases. The Pancreas Clinic specializes in multidisciplinary, patient-centered treatments and innovative research for all types of pancreatic diseases and disorders.
Our clinic unites specialists from across Cleveland Clinic, including pancreatic surgeons, gastroenterologists, radiologists, anesthesiologists, psychologists and oncologists, who together work to customize the best possible treatment for patients and give them improved quality of life. This collaboration also means that patients get the care they need right away, rather than waiting for separate appointments with various specialists.
Cleveland Clinic’s Pancreas Clinic is one of the few centers in the nation that specializes in patient-centered treatments and frontline research for every type of pancreatic disorder.
The Pancreas Clinic treats disorders such as complicated acute pancreatitis, chronic pancreatitis, and pancreatic cancer. Each year, more than 1,500 patients trust the Pancreas Clinic with their healthcare needs.
The Pancreas Clinic offers a single location for patients to receive the best therapies and treatment options for pancreatic disorders. Patients travel from around the country to receive our innovative treatments and services, including:
- Endoscopic, minimally invasive and radiographic diagnostic imaging
- Islet auto transplantation
- Robotic surgery for pancreatic cancer
- Robotic pancreaticoduodenectomy
- Chronic pain management using pancreatic enzymes, subcutaneous injections of octreotide, and other alternative treatments.
Current Pancreas Clinic research may lead to the development of a new test for the early detection of pancreatic cancer.
Resources
Stay Connected
- Explore our services, locations and more
- Subscribe to Health Essentials e-News for expert insights on nutrition, health and wellness. Get free guides to common conditions, too
- For more information on Pancreatic Diseases, listen to Episode 27 and Episode 32 of our Butts & Guts podcast
- Find a wealth of family health & wellness tips
- YouTube