Overview
Minerals like calcium, phosphorus and magnesium are often taken for granted, but they are critical to your health. Too much or too little of these minerals can not only be detrimental to your body’s ability to function properly, but can also lead to other serious problems or complications. We can help.
At Cleveland Clinic’s Endocrine Calcium Clinic, our team of experts specializes in the treatment of common and rare parathyroid and calcium disorders, as well as uniquely focuses on bone and mineral regulation problems associated with the surgical treatment of obesity.
Bone & Mineral Metabolism Disorders

Osteoporosis — Osteoporosis is a condition in which there is a loss of the mineral part of the bone and thinning and disintegration of the spongy part of the bone. This increases an individual’s risk of bone breaks, especially hip or spine fractures (breaks), but other bones throughout the body are affected, too. Osteoporosis is much more common in females than in males due to the rapid loss of bone minerals experienced in women three to eight years after menopause.
- Primary osteoporosis — This is the most common type of osteoporosis. It is caused by aging and postmenopausal estrogen decline. Treatment for the condition typically includes determining the severity of the osteoporosis with a bone densitometry or DXA scan, a type of testing that quickly and accurately measures the amount of calcium in certain parts of your bones. Our team works with each patient to prevent fractures and combat the spread of the osteoporosis. They may recommend the use of medications that help to increase bone density and strength by slowing down bone resorption (destruction).
- Secondary osteoporosis — There are a large number of diseases that affect the body and secondarily affect the skeleton. Our Endocrine Calcium Clinic physicians work closely with the individual to determine what treatment option is right for them, such as therapy to address the primary cause of the disease, changing medications that are known to affect the skeleton, or taking supplements or osteoporosis medications.
Osteopenia — This condition is very similar to primary osteoporosis, but of a milder degree. Diagnosis is usually completed by a blood test or densitometry test to determine if the individual is currently losing bone or if they have risk factors for further bone thinning.
Paget’s disease — This condition differs from osteoporosis in which part of the skeleton (sometimes just one bone) suffers from greatly increased and irregular remodeling (the breaking down and regrowth of bone tissue). Bone affected with Paget’s disease is thickened but weak. The condition is diagnosed by X-rays that can show the irregular bone structure. Patients may have pain, sometimes severe, in the affected bone, or pain from compression if it’s located near nerves. Paget’s can also lead to deformation of weight-bearing bones.
The cause of the disease is currently unknown but some viruses have been suspected. Cleveland Clinic calcium specialists work with patients to help with pain management and proper treatment options. Additionally, our endocrine surgeons are available to work with a patient if corrective surgeries are necessary to improve function of the affected bone.
Hypercalcemia — Hypercalcemia means having an elevated level of calcium in the blood. Most of the time, this is a very mild condition and does not cause any symptoms. It is commonly discovered while testing for something else. If calcium in the blood increases significantly over the normal level, some symptoms may appear. The most common symptoms are thirst and frequent urination. Other symptoms are loss of bone density, bone fractures and kidney stones. High blood pressure, heartburn and mild mental disturbances are less common.
The most common cause of hypercalcemia is primary hyperparathyroidism due to the development of a tumor in the parathyroid glands.
Cleveland Clinic calcium experts recognize the complexity of this disease and use an extended diagnostic approach to ensure the right course of treatment, such as medication to control overactive parathyroid glands, rebuild bone, or reduce vitamin D or calcium levels. Our endocrine surgeons also work closely with individuals if surgery is needed to remove the parts of the parathyroid that are not working properly.
Hypocalcemia — Hypocalcemia means having a decreased level of calcium in the blood. Symptoms of hypocalcemia are related to overactive nerves and muscles and include tingling, numbness of body parts (especially around the mouth and fingertips) as well as muscle twitching. Severe hypocalcemia may lead to whole body spasms.
Hypocalcemia is diagnosed using a blood test. This condition is most commonly caused by a lack of parathyroid glands (after surgery or radiation); however, more subtle problems may be present, such as vitamin and mineral deficiencies, primary intestinal dysfunction, liver disease, gastrointestinal issues and autoimmune disorders. Our Endocrine Calcium Clinic experts use advanced diagnostics to find the root of the issue, as well as uncover and treat more rare subtle associated problems.
Vitamin D deficiency — Vitamin D is important for absorbing calcium into the blood stream. Low blood levels of vitamin D can prevent enough calcium from being available for rebuilding the skeleton throughout life. This leads to poorly calcified bone, much like in osteoporosis.
When vitamin D deficiency is prolonged and severe, it results in a bone condition known as osteomalacia. This can cause bone and muscle aching. In severe cases, fractures may occur. However, most patients have a mild form and are basically without symptoms. Diagnosis is usually made during the evaluation of low bone density from a DXA scan. Treatment by our Endocrine Calcium Clinic experts depends on the individual case and severity of the deficiency, and can range from taking of medications or supplements, wearing braces to reduce or prevent bone irregularities or surgery to correct bone deformities.
Hormonal Disorders
Hyperparathyroidism — This is a condition in which one or more of the parathyroid glands become overactive and secrete too much parathyroid hormone (PTH). This causes levels of calcium in the blood to rise (hypercalcemia).
- Primary hyperparathyroidism — This type of hyperparathyroidism is usually caused by small tumor in one or more of the glands. The only known cure for primary hyperparathyroidism is surgical removal of the affected gland(s). However, some patients can be monitored if calcium is only slightly elevated. To determine the right course of treatment, Cleveland Clinic Endocrine Calcium Clinic experts and endocrine surgeons work hand-in-hand to carefully evaluate and assess each individual’s medical need.
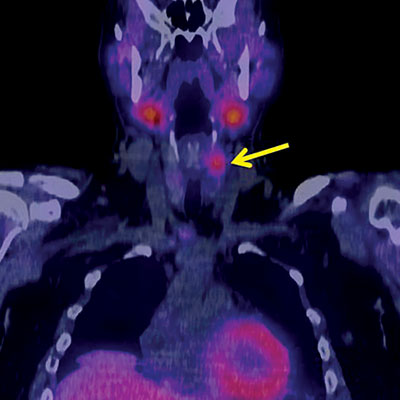
Several non-invasive tests may be used to locate the affected gland(s), including ultrasound, CT, MRI, PET and the Sestamibi scan. For surgical management of hyperparathyroidism, significant advances have been made in the past decade, including less invasive procedures and better diagnostic evaluation and monitoring. Close collaboration between endocrinologists and endocrine surgeons at Cleveland Clinic gives patients the opportunity to consider fully the pros and cons of all treatment options, whether surgery versus conservative “waiting and seeing” or medical therapy. - Secondary hyperparathyroidism — In this version of hyperparathyroidism, parathyroid hormone is elevated, but this is not caused by abnormal secretion from the parathyroid glands. Instead, it is caused by either low calcium levels (in cases of vitamin D deficiency) or elevated blood phosphorus levels, such as in patients who have severe kidney insufficiency. Our Endocrine Calcium Clinic experts can work with patients to properly correct low calcium or high phosphorus, so the secretion of parathyroid hormone returns to normal.
- Tertiary hyperparathyroidism — Tertiary hyperparathyroidism is a condition in which long-standing secondary hyperparathyroidism cannot be reversed any more — even by adequate treatment. Most commonly, this is seen in patients with kidney failure. Typically, these patients are best treated by surgical removal of the parathyroid glands.
- Hypoparathyroidism — Hypoparathyroidism is a condition in which not enough parathyroid hormone is secreted. This is most commonly caused by surgical removal of the parathyroid glands, or after radiation treatment in this area. This causes hypocalcemia (low blood calcium levels). These patients are treated with vitamin D and calcium.
- Pseudohypoparathyroidism — This very rare genetic condition is one in which the body cannot sense parathyroid hormone. These patients have symptoms of hypoparathyroidism, but have normal blood levels of parathyroid hormone. Treatment recommendations from our Endocrine Calcium Clinic experts will try to help patients maintain appropriate calcium levels. For patients who have high blood phosphate levels, a low-phosphorous diet or medication (phosphate binders) may also be needed.
Parathyroid cancer — This is a very rare disease and is characterized by having a mass in the neck. These tumors often produce parathyroid hormone. Symptoms are caused by local effects of the tumor, possible metastases (spread of the tumor to another part of the body) and hypercalcemia. If parathyroid cancer is suspected, experts may order diagnostic blood tests, parathyroid hormone test, Sestamibi scan, CT, ultrasound, angiogram or venous sampling.
Our Endocrine Calcium Clinic team works closely with each patient to make sure they get the treatment that’s right for them to properly manage their disease — and monitor them throughout the process. Treatment includes controlling hypercalcemia (too much calcium in the blood) in patients who have an overactive parathyroid gland. To reduce the amount of parathyroid hormone produced and control blood calcium levels, as much of the tumor as possible is surgically removed. Radiation therapy or chemotherapy may also be used. For patients who cannot have surgery, medication may be used.
Other conditions — Our team also specializes in managing and treating:
- Increased risk of metabolic abnormalities from disease such as inflammatory bowel disease, cancer, renal failure
- Metabolic abnormalities that occur after bariatric surgery or organ transplantation
- Renal stones and kidney failure due to parathyroid and calcium problems
Diagnostic Technology
The following tests may be used to help diagnose parathyroid and calcium disorders:
Parathyroid hormone test — A procedure in which a blood sample is checked to measure the amount of parathyroid hormone released into the blood by the parathyroid glands. A higher than normal amount of parathyroid hormone can be a sign of disease.
Blood chemistry studies — A procedure in which a blood sample is checked to measure the amounts of certain substances released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease in the organ or tissue that makes it.
DXA scan — This test is one of the most accurate ways to detect bone density-related diseases such as osteoporosis. The test usually takes around 10 to 15 minutes.
When surgery is needed, we use leading-edge imaging to identify the goiter location or involved glands. These may include:
Ultrasound exam — A procedure in which high-energy sound waves (ultrasound) are bounced off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram.
Sestamibi/CT scan — Sestamibi is a chemical that localizes in the abnormal parathyroid gland. The Sestamibi scan, especially performed with computerized tomography (CT), is the most specific test. The procedure uses a computer linked to an X-ray machine to make a series of detailed pictures of areas inside the body, taken from different angles. In some cases, an invasive test, such as arteriography or blood sampling in the neck, may be required prior to surgery.
Venous sampling — A procedure in which a sample of blood is taken from specific veins and checked to measure the amounts of certain substances released into the blood by nearby organs and tissues. If imaging tests do not show which parathyroid gland is overactive, blood samples may be taken from veins near each parathyroid gland to find which one is making too much PTH.
Appointments & Locations
Ready to make an appointment?
The specialists in the Endocrine Calcium Clinic can be reached at 216.444.6568 or 800.223.2273, ext. 46568.
Virtual Second Opinion
If you cannot travel to Cleveland Clinic, help is available. You can connect with Cleveland Clinic specialists from any location in the world via a phone, tablet, or computer, eliminating the burden of travel time and other obstacles. If you’re facing a significant medical condition or treatment such as surgery, this program provides virtual access to a Cleveland Clinic physician who will review the diagnosis and treatment plan. Following a comprehensive evaluation of medical records and labs, you’ll receive an educational second opinion from an expert in their medical condition covering diagnosis, treatment options or alternatives as well as recommendations regarding future therapeutic considerations. You’ll also have the unique opportunity to speak with the physician expert directly to address questions or concerns.
Why Choose Us
At Cleveland Clinic, our Endocrine Calcium Clinic’s endocrinologists work hand in hand with endocrine surgeons and a complete nursing staff to accurately diagnose and treat all forms of parathyroid and calcium disorders, and mineral abnormalities. This close collaboration with endocrine surgery is key especially in the evaluation and treatment of certain parathyroid disorders or cancer to ensure accurate diagnoses and optimal outcomes for patients, no matter how rare the condition.
Our laboratory facilities allow our experts to perform specialized testing not found at most medical centers. Our patients also have access to therapies using the latest forms of oral and injectable medications for many bone diseases.