What is Scoliosis?

Scoliosis is an abnormal sideways curvature and rotation of the spine — the backbone of your body. It is made up of 33 vertebrae (bones), and stretches from your head to your tailbone. Your spine houses your spinal cord, a collection of nerves and cells that connect with your brain, to form the central nervous system. When the spine curves due to diseases such as scoliosis, functional and cosmetic issues arise. These symptoms can be painful, but are rarely dangerous.
While scoliosis occurs most often in teenagers, it also occurs in adults. The good news is that treatment is available for adults with worsening or painful curves to help improve symptoms and correct the spine’s deformity.
What is Kyphosis and How is it Different From Scoliosis?
Kyphosis is another type of spinal deformity that most people refer to as having a “hunchback.”
While the normal spine has a slight curvature (kyphosis) to it, when the curve in the upper spine is more than 45 degrees it is usually referred to as “hyperkyphosis.” Some types of hyperkyphosis affect mainly children and adolescents (including congenital, postural and Scheuermann’s kyphosis). Adults most often experience what’s known as “agerelated kyphosis.”
Fractures due to osteoporosis may be a cause of age-related kyphosis. Treatments for kyphosis may include pain and/or osteoporosis medications and stretching exercises. Surgery may be recommended if the kyphosis is severe or causing pain.
Causes
There are Two Types of Scoliosis Seen in Adults
Idiopathic scoliosis – This is the type of scoliosis also seen in teenagers. Its cause is unknown but it has a genetic basis and may be a combination of abnormal development of the bones, soft ligaments or weak muscles, or abnormalities with the inner ear and balance function.
In some cases, an already-diagnosed curve progresses or begins to cause symptoms in adulthood. In other cases, it is not diagnosed until adulthood.
Degenerative scoliosis – This second common type of adult scoliosis occurs when tissue wears away due to aging (degenerative processes) in the low back, leading to the development of a curve in the spine. It tends to occur after age 40 and the problem may occur in the spine’s discs, facet joints or vertebrae. Muscle weakness may also be a contributing factor.
Symptoms
Most scoliosis causes no physical symptoms. It may cause some cosmetic abnormalities, including:
- Uneven shoulders or waistline
- One or both shoulder blades sticking out
- Leaning slightly to one side
- A hump on one side of the back
Back pain may occur and is generally muscular in nature, and will often respond to a physical therapy program. Degenerative scoliosis may also cause muscle pain and leg pain, in addition to back pain.
Adult idiopathic scoliosis and degenerative scoliosis have long been thought to lead to shortness of breath and chest pain. Today, this has been shown to be extremely rare, and patients with these symptoms should be investigated for other causes.
Diagnosis
Your doctor will discuss your medical and family history with you. He or she will examine your back to check the shape of your spine, and perform a physical and neurological exam. If a curve is detected, X-rays are used to pinpoint the location, extent and degree of curvature.
Treatments

As an adult, your spine is no longer growing, but it is important to stabilize your spine and lessen symptoms. The more active someone is, the less likely they are to experience progressive symptoms.
Medical treatments
Conservative medical treatment is the most common treatment option for patients with both idiopathic and degenerative scoliosis.
This begins with physical therapy, aerobic exercise, stretching and lengthening to improve flexibility, over-the-counter pain medications, and – if needed – mild prescription medications, typically anti-inflammatories.
If symptoms are related to neurological symptoms, an epidural steroid injection is sometimes used to decrease symptoms temporarily
Surgical treatments
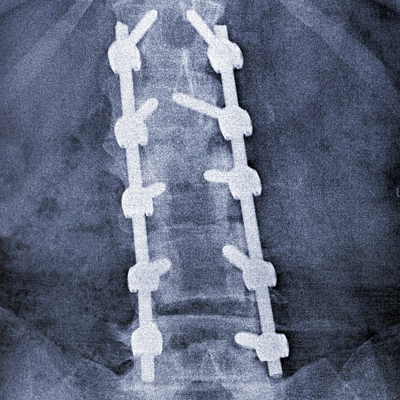
Fusion surgery may be recommended for adults with degenerative scoliosis who have spinal stenosis (a narrowing of the spinal canal in the lower back). These patients may experience leg pain and numbness and MRI is used to confirm this narrowing.
The goal of surgery is to decompress the spinal canal and relieve the symptoms and a fusion is performed to prevent further progression of the curve.
In adults, surgery for curve progression alone is rare.
Are Braces Ever Used in Adults?
Our surgeons do not believe that braces should ever be used for managing scoliosis symptoms in adults.
The reason? Any brace that provides support to the spine will unload the muscles. Any muscle that is not working becomes weaker and eventually braces will always lead to increased back pain as the muscles become progressively weaker.
Core-strengthening exercise programs and regular daily activity are much more effective at easing symptoms. The more active someone is, the less likely they are to have progressive symptoms.
Risks of Spine Stabilization Surgery
Any surgical procedure includes general risks, such as adverse reactions to anesthesia, postoperative pneumonia, blood clots in the legs, infection and blood loss requiring a blood transfusion.
Risks specific to spine stabilization surgery include injury to the nerves or spinal cord that could result in pain or even paralysis (the estimated risk of paralysis for major spinal reconstructions is about 1 in 10,000), the instrument breaking, dislodging or irritating the surrounding tissue and the pain from the surgery itself.
Risks of spine stabilization surgery vary by individual. Please discuss your risk level with your surgeon prior to surgery.
Most patients who undergo spine stabilization surgery stay in the hospital about a week and can return to work or school (including driving) two to four weeks after surgery. Patients must avoid bicycling for one month and any running, jumping or sports for three months. They can typically return to all of their regular daily activities in about four to six months.
Patient Services
MyChart
MyChart is a secure online tool that provides personalized health information from the privacy of your home at any time, day or night. Learn more or login now.
Virtual Visits with Orthopaedics
Select patients now can see our providers online from their home or office by using the Cleveland Clinic Express Care® Online tool. This service allows patients a fast, secure and easy way to receive care from their healthcare team in a live virtual visit using a smartphone (iPhone or Android), tablet or computer. The benefits of choosing a virtual visit include no travel or parking, less waiting, significant time savings, no facility fee and the convenience of seeing your physician from wherever you choose.
Virtual Visits with Orthopaedics
New patients with common knee injuries or knee pain.
Established patients scheduling follow-up care appointments such as:
- Post-Surgical & wound check visits
- Fracture care follow-up
- Injection follow-up
- Musculoskeletal injury follow-up
- Per-operative teaching prior to surgery
If you would like to use Express Care Online for your next visit, please call your provider’s office. If you are eligible, our team will schedule your virtual visit and provide details on the cost of your appointment and setup instructions.
Appointments
Make an Appointment
To make an appointment with a Center for Spine Health specialist, please call 216.636.5860 or 866.588.2264.
Virtual Visits
Whether you're a new or existing patient, you can get an initial evaluation or follow-up care from a spine specialist using your phone, tablet or computer. This means there's no travel or parking, less waiting and significant time savings. Call 216.636.5860 to schedule a virtual visit for you or a loved one and get details on cost and set-up instructions.
Why Choose Us?
Cleveland Clinic’s Center for Spine Health experts tailor treatment plans to their patients’ needs, taking into account the extent of the problem and the patient’s overall health.
We use a multidisciplinary approach, combining the expertise of orthopaedic surgeons, neurosurgeons, radiologists, rehabilitation specialists and pain management specialists.