Overview
About the knee
Your knee is the largest joint in your body. It is a complex mechanism made of bone, cartilage and ligaments. The cartilage in your knee acts as a cushion and gliding surface. When healthy, the cartilage keeps the bones in the joint from rubbing together. However, when the joint is affected by arthritis, the bones make contact and cause pain. Injuries, aging and degenerative conditions such as arthritis can cause the cartilage to break down.
Knee pain can affect every step you take. From playing sports to climbing steps, knee pain is difficult to ignore. Many home remedies can help, but if you have chronic pain or symptoms, such as swollen or red joints, it’s time to see a doctor.
Types of Pain
What are the different types of knee pain?
Knee pain has many causes. Some of the most common include:
Osteoarthritis
Sometimes referred to as “wear and tear” arthritis, osteoarthritis is a chronic condition that causes joint inflammation. It is the gradual breakdown of the cartilage in the knee. It is also called degenerative joint disease, osteoarthritis usually develops over years and is often found in patients who have had a knee infection, injury or are overweight.
As cartilage wears away, the bones around it can grow thicker and develop bony spurs. This can lead to increased friction between the bones and disrupted movement in your knee. This also can lead to problems with the synovium, a membrane in your knee that produces a liquid to keep your cartilage slippery. This membrane can become inflamed and make too much fluid. This results in swelling, or “water on the knee.” In the most severe cases, the knee can become deformed as the continued friction wears away the bone.
Common symptoms of osteoarthritis include pain, stiffness, tenderness, a limited range of motion and a grating sensation when you bend your knee. The pain is usually worse after activity.
Rheumatoid arthritis
Rheumatoid arthritis can affect joints on both sides of the body (both knees, both hands and/or both wrists). In rheumatoid arthritis, your body’s cells attack your own tissues. Symptoms typically develop gradually however, they can also appear rapidly. Rheumatoid arthritis affects three to five times more women than men and often presents between the ages of 20 and 50.
Rheumatoid arthritis may be related to a combination of abnormal immunity and genetic, environmental and hormonal factors. Over time, rheumatoid arthritis can cause cartilage to wear away, swelling in the synovium, and excess fluid in the knee. In later stages, bones can rub against each other increasing pain and other symptoms.
Bursitis
Bursitis is the inflammation of any of the fluid-filled sacs protecting the body’s joints. This is usually caused by repetitive motion or by a stress such as kneeling. Sometimes, a sudden injury can cause bursitis.
Tendonitis
The tendons – rope-like tissues connecting muscles to bone at the knee and other joints – can become painfully inflamed by repetitive and strenuous movement. Tendonitis is a common sports injury, caused by overuse of the same parts of the body. Patellar tendinitis, or “jumper’s knee,” is an inflammation or irritation of the tendon between the knee cap and the shin bone.
Baker’s cyst
A lump behind your knee could be a Baker’s cyst. A Baker’s cyst, also called a popliteal cyst, is a fluid-filled pocket that causes swelling and tightness behind the knee. Often, it is not painful. A Baker’s cyst is typically associated with arthritis or a cartilage tear, conditions that can cause your knee to produce too much fluid. The key to treatment is to find the underlying cause of the fluid accumulating in the Baker’s cyst.
Patellofemoral pain syndrome (PFPS)
Knee pain or discomfort while walking up and down stairs, jumping or squatting may be symptoms of patellofemoral pain syndrome. This common knee problem is felt toward the front of the knee. It can cause a grinding sensation when bending or straightening your leg, and can cause your knee to occasionally buckle. Sometimes called “runner’s knee,” patellofemoral pain syndrome may be caused by a kneecap that is not aligned properly, overuse, injury, excess weight or when the cartilage in the knee cap is worn significantly.
Injuries

Knee injuries can be the result of sports, falls or trauma. They typically involve the ligaments that hold two of the bones of the knee – the femur and tibia – together. Here are some of the most common types:
ACL
Injuries to the anterior cruciate ligament (ACL) are among the most common and dreaded sports injuries. Your ACL keeps your knee from moving too far out of position. Changing directions too quickly or hyperextending the knee can tear the ACL. Women are more prone to tearing the ACL than men. Surgery is often necessary to repair damage to an ACL.
MCL
A stretch or tear of the medial collateral ligament (MCL) is typically caused by a hit or blow to the outer knee. Pain is felt along the inner knee. Bracing and conservative treatment, such as rest and physical therapy, are usually sufficient to heal these injuries.
Meniscus
The meniscus is crescent-shaped cartilage between your thigh bone (femur) and lower leg bone (tibia). You have two of these cushions in each of your knees, inner (medial) and outer (lateral). The medial one is most often injured. These injuries often are caused by sudden twisting, resulting in swelling, pain and locking of the knee. Arthroscopic surgery may be necessary to remove the torn fragment when conservative treatment does not help.
Diagnosis
Physicians in Cleveland Clinic’s Orthopaedic & Rheumatologic Institute can help sort out the possible causes of your knee pain. When diagnosing any knee pain, the physician will take your medical history and perform a thorough physical examination. To help your doctor best understand your knee pain, you’ll need to provide the following information:
- A description of your knee pain (aching, tenderness, burning or swelling).
- Where the pain is located and when it occurs.
- When the pain started (and if it is the result of an injury or accident).
- Anything that makes the pain worse or better.
- Any medication you’re taking and medication allergies.
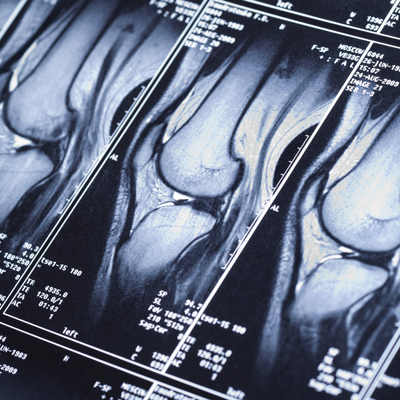
Your doctor also may order imaging tests to view the joint, which may include the following:
X-rays – An X-ray can show if there are certain problems, such as deterioration or fracture, within your knee.
MRI – In some cases, your doctors may order a magnetic resonance imaging (MRI) scan. An MRI provides significantly more detail about the soft tissues in your knee, such as the cartilage on the surface of the bones, ligaments, tendons and muscles
CT scan – Computerized tomography scans (CT) combine X-ray views from multiple angles, creating a two- or three-dimensional, cross-sectional image. These images show “slices” of bone and soft tissue.
Treatments
Most knee problems do not require surgery and are best treated with a comprehensive conservative treatment program. However, when necessary, our specialists are highly skilled in the latest techniques of arthroscopic surgery and total knee joint replacement.
Conservative care
Many types of knee pain can be relieved and/or resolved with conservative treatments such as:
Braces – In general, knee braces wrap around the knee and leg and help limit unwanted movement while supporting the knee. They can be helpful when knee ligaments are weak or to help keep the knee from “buckling.” Braces will provide support during healing, but are not a primary treatment for arthritic degeneration.
There are a variety of braces. Functional braces are designed to support knees that have suffered an impact-related injury. Rehabilitative braces provide support when recovering from a surgery or injury. Uploading/offloading braces are used by patients with arthritis and help to stabilize the knee when standing up or sitting down. Sometimes a simple compressive knee sleeve may help to reduce knee pain and swelling.
Rest — When your knee hurts, it’s important to rest it. Pain and inflammation will not subside if repetitive activities (such as vacuuming or raking) continue to stress the sore knee. However, some movement is important. Most importantly, if you experience pain, don’t push through that pain.
Ice and heat — Icing the knee with cold packs (or bags of frozen peas or corn) when pain is severe reduces inflammation, swelling and discomfort. Apply ice for 15 to 20 minutes, three to four times each day. To avoid burning the skin, make sure to place a thin towel between the ice and your leg. Heat can also help chronic knee conditions. Try taking hot showers and doing recommended stretches first thing in the morning. Or, you can alternate ice and heat (taking at least a 40-minute break between each) to get the benefits of both.
Physical therapy – Once your doctor diagnoses the cause of your knee pain, physical therapy may be the next step. Physical therapists can show you specific exercise programs that will help you recover from the injury and decrease the pain you are experiencing. They also may demonstrate stretches and low-impact exercises that can strengthen muscles around your knee, improve stability and flexibility, and reduce pressure on the joint. They can advise you on how to engage in low impact aerobic exercises, such as swimming and cycling, that may not aggravate your knee pain. Physical therapy is also an important part of recovery after knee surgery.
Neuromuscular Electric Stimulation (NMES) – These special devices use electricity to contract the muscles in your thigh. These can be used in physical therapy or worn as a wearable wrap at home. These can help to build additional muscle strength to help with recovery from knee injuries or after a knee replacement.
Over-the-counter medications - Knee pain can be often relieved with over- the- counter- medications including oral non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil®) or naproxen (Aleve®), topical NSAIDs such as Volaren® and anti-analgesia (pain-relieving) medications such as acetaminophen (Tylenol®). There are also topical creams and ointments that can provide temporary numbing relief.
Vitamins and Supplements – There are many vitamins and supplements that you can take for your health, but the two that have been shown to help with the pain related to knee osteoarthritis are Glucosamine and Chondroitin. Your provider may talk to you about these and other natural supplements that may help with knee pain.
Prescription medications - If over-the-counter medications don't provide relief, prescription-strength NSAIDs can be prescribed. Opioid medications are rarely ever prescribed except in the early post-surgical period or in the setting of a significant fracture, as opioids are not very helpful outside of these two scenarios.
Injections — You may consider injections to reduce pain and inflammation before or after attempting other conservative treatments. Corticosteroid (“cortisone” or “steroid”) injections may temporarily help to “settle down” inflamed tissues within the joint, reducing pain and swelling. Viscosupplementation (“gel”) injections, if approved by insurance, can help to cushion and lubricate the knee joint, further reducing pain and swelling. Other types of injections, like platelet rich plasma (PRP), can be discussed with one of our Cleveland Clinic Joint Preservation Center physicians.
Nerve blocks and ablations — These treatments to nerves can be performed by pain management physicians to lessen the pain around the knee if other conservative treatments are not successful. These are sometimes attempted as an alternative to surgery if a patient may not be a suitable surgical candidate.
Weight loss - Maintaining a healthy weight is an important part of treating knee pain. If you do have excess weight that could be affecting your knee, your doctor may recommend that you lose weight to help reduce pressure on your knee. The Cleveland Clinic can provide multiple options to help you achieve these weight loss goals.
Surgical Options
Arthroscopy
Arthroscopy is a relatively minor surgery performed with the use of a miniature camera (arthroscope). Arthroscopic knee surgery is commonly used to diagnose and treat knee pain. This surgery takes about an hour and patients go home the same day. During the procedure, an orthopedic surgeon can repair tissue or remove injured fragments to ease knee pain. Advances in arthroscopy have made this process more accurate and effective than ever before.
Recovery – In most cases, arthroscopy is an outpatient procedure. Patients can often return to office work within a week or two and to a normal lifestyle within a month or two. Physical therapy is often important for regaining mobility after surgery.
Benefits – This surgery involves only small incisions for the arthroscope and other tools, meaning a quicker recovery. Arthroscopy can provide relief from knee pain and improve mobility, allowing patients to return to a normal, active lifestyle with greater comfort.
Who is a candidate? – Patients with knee problems such as ACL tears, meniscus tears and focal cartilage tears are good candidates for arthroscopic surgery. The surgery can be performed on patients of all ages, depending on the condition of the knee.
Risks – Knee arthroscopy is a safe procedure with few complications. Risks may include swelling, stiffness, bleeding, blood clots, infection or continuing knee problems.
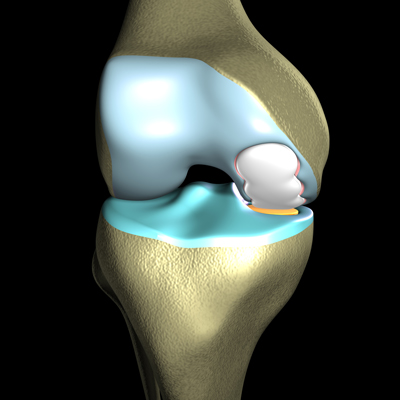
There are three compartments to the knee. In a resurfacing, only the damaged areas are replaced.
Focal Knee Resurfacing
For the right patients, resurfacing is a great alternative to a knee replacement. This procedure replaces only a specific area of the knee cartilage surface. Broken down cartilage is removed and replaced with a custom-made, metal implant that is cemented to the bone.
Recovery – Patients are encouraged to walk soon after surgery. Many are able to drive after a week or two. Physical therapy is an important part of getting back mobility in your knee.
Benefits – Knee resurfacing may be the wave of the future in treating severe knee pain. It is less invasive than a knee replacement. Because less bone is cut away, patients are left with more of a “real knee.” It also can feel more natural than a knee replacement because the implant is custom-made to fit a patient’s knee. Recovery can be shorter than it is with a knee replacement.
Who is a candidate? – Knee resurfacing may be ideal for younger, more active patients. It can be effective for patients with focal cartilage defects and early to mid-stage osteoarthritis.
Risks – Possible (but rare) complications of surgery include blood clots, infection and nerve damage. Long-term complications may include continued pain, infection or a loosening of the implant.
Durability – Knee resurfacing is a new procedure and is predicted to last 10 to 15 years.
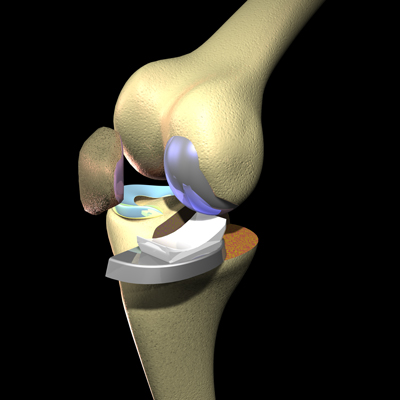
Partial knee replacement
Partial knee replacement may be an option for you if parts of your knee are free of disease or injury. This minimally invasive procedure may be possible when just one the three compartments of your knee are damaged. In a partial knee replacement, arthritic cartilage and the underlying bone are removed and replaced with an implant in the affected compartment. This means less soft tissue disruption and a shorter recovery time than with a total knee replacement.
Recovery – Patients are up and walking the day of surgery. Physical therapy is key to recovery and regaining mobility. Patients can be back to full activity in about 6-8 weeks. Low impact exercises and activities are recommended following surgery.
Benefits – Compared to a total knee replacement, a partial knee replacement has a shorter recovery time, less post-operative pain, less blood loss during surgery and less soft tissue disruption. In addition, the patient’s healthy bone and soft tissues are preserved, which leads to a better range of motion and knee function than is typical with a total knee replacement. Patients who have partial knee replacements also are still candidates for a total knee replacement, if needed, down the road.
Who is a candidate? – The ideal candidate has osteoarthritis that is severe, isolated to one compartment of the knee and whose pain can no longer be managed with non-operative treatments. Patients with severe deformity or lack of motion typically are not good candidates.
Risks – Possible (but rare) complications of surgery include blood clots, infection, nerve damage and other risks. Long-term complications may include continued pain, infection, and failure of the implant
Durability – Approximately 85 percent of partial knee replacements are still functioning well at 15 years.
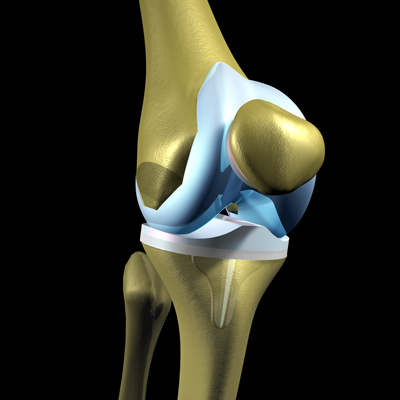
Total knee replacement
When all of the parts of a knee need repair, total knee replacement may be the best option. This involves removing broken down cartilage and bone and replacing it with the right artificial joint for you. This prosthesis is made of plastic and metal and provides fluid and free movement. It is attached to the bone with acrylic cement or can be press-fit, allowing bone to grow into the implant. Surgeons also perform any needed ligament repair. To work properly, the new joint needs support from the patient’s muscles and ligaments.
Recovery – Following a total knee replacement, most patients spend only one to two days in the hospital however, many are done as an outpatient procedure. Patients can stand and move the joint the day after surgery and use a cane, walker or similar aid for several weeks. Physical therapy is crucial to restore motion to your joint. After six weeks, most patients are able to put full weight on their knee with the use of a cane. Full recovery and rehabilitation typically takes about six months. Patients are able to return to an active lifestyle, except for high impact activities, such as running and jumping.
Benefits – Most patients experience dramatic improvement and relief from pain within weeks of surgery.
Who is a candidate? – Total knee replacement can be a good option for people with painful knee deformities, severe degenerative changes, or advanced or end-stage arthritis.
Risks – The risk of complications is rare in total knee replacement surgeries, occurring in less than 2 percent of patients. Your surgeon may prescribe blood thinners to prevent blood clots after surgery. Some patients notice some loss of motion, stiffness or pain. For a very small percentage of patients, the joint may fail. Studies have shown this is more common in obese patients.
Durability – Doctors have been performing total knee replacements since the early 1970s, and it is one of the most successful surgeries for knee arthritis. New data suggest that contemporary knee replacements may last more than 30 years. Approximately 85 percent of knee replacements done 20 years ago are still functioning well.
Patient Services
MyChart
MyChart is a secure online tool that provides personalized health information from the privacy of your home at any time, day or night. Learn more or login now.
Virtual Second Opinion
If you cannot travel to Cleveland Clinic, help is available. You can connect with Cleveland Clinic specialists from any location in the world via a phone, tablet, or computer, eliminating the burden of travel time and other obstacles. If you’re facing a significant medical condition or treatment such as surgery, this program provides virtual access to a Cleveland Clinic physician who will review the diagnosis and treatment plan. Following a comprehensive evaluation of medical records and labs, you’ll receive an educational second opinion from an expert in their medical condition covering diagnosis, treatment options or alternatives as well as recommendations regarding future therapeutic considerations. You’ll also have the unique opportunity to speak with the physician expert directly to address questions or concerns.
Virtual Visits with Orthopaedics
New patients with common knee injuries or knee pain.
Established patients scheduling follow-up care appointments such as:
- Post-Surgical & wound check visits
- Fracture care follow-up
- Injection follow-up
- Musculoskeletal injury follow-up
- Per-operative teaching prior to surgery
Ask your physician if a virtual visit follow-up appointment is right for your follow-up care.
What is the cost of an orthopaedic virtual visit?
- New patients: $75
- Follow-up visits: $49
- Post-surgical visits: $0*
- Fracture care visits: $0*
- *Within 90 days of incident.
If you would like to use Express Care Online for your next visit, please call your provider’s office. If you are eligible, our team will schedule your virtual visit and provide details on the cost of your appointment and setup instructions.
Appointments

To make an appointment with a knee specialist, call:
- Cleveland Appointments: 216.444.2606
- Akron Appointments: 330.344.2663
- Canton Appointments: 330.489.1362
- Dover Appointments: 330.343.3335
Why Choose Us?
Choosing Your Care
Approximately 1 in 4 people visit a doctor or a hospital because of knee pain each year. Fortunately, there are many ways to successfully treat knee pain and get back to an active lifestyle.
The physicians and surgeons at Cleveland Clinic’s Orthopaedic & Rheumatologic Institute are recognized as among the best in the world for knee assessment and repair. We use a multidisciplinary team approach, with all of the experts you need under one roof, including orthopaedic physicians and surgeons, rheumatologists and physical therapists.
With a broad range of treatment options, state-of-the-art diagnostics and decades of experience, we can evaluate the cause of your knee pain and determine the treatment that is best for you. We also offer convenience, with same-day access and multiple locations throughout Northeast Ohio.
Knee pain can affect every step you take. From playing sports to climbing steps, knee pain is difficult to ignore. Many home remedies can help, but if you have chronic pain or symptoms such as swollen or red joints, it’s time to see a doctor.