A colposcopy is a procedure to check your cervix, the wall of your vagina and your vulva for signs of cancerous or pre-cancerous tissue. If you’ve had an abnormal Pap test or a positive HPV test, your provider may recommend colposcopy to get closer to a diagnosis.
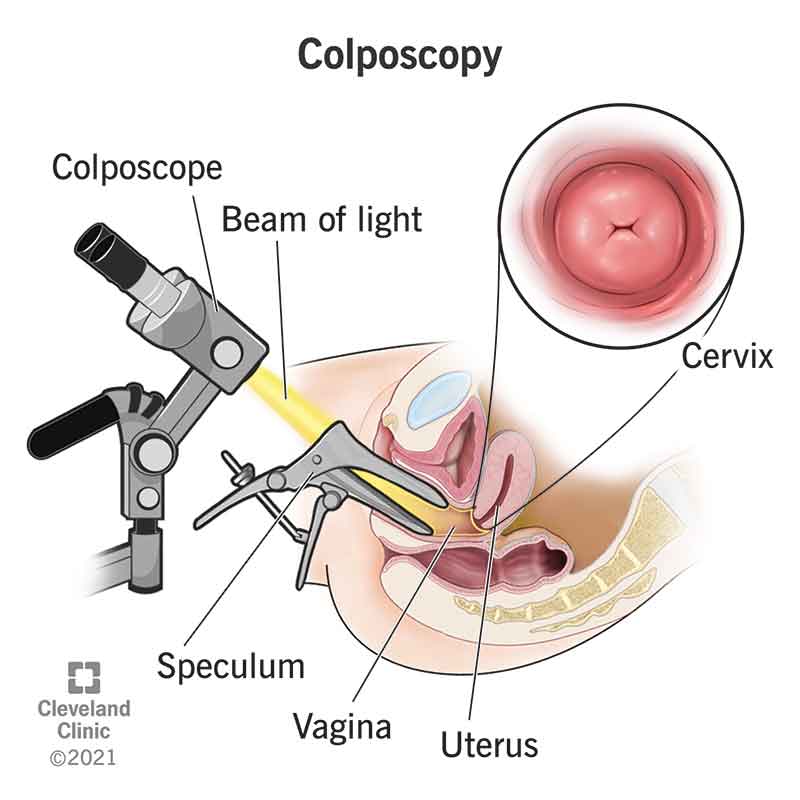
Colposcopy is a diagnostic procedure that allows your provider to check your cervix (lower part of your uterus) and the wall of your vagina for abnormal tissue. During the procedure, a special lighted microscope called a colposcope magnifies the tissue that lines your cervix and vagina. If your provider sees any abnormalities, they can take tissue samples (biopsies) that can be tested in a lab for cancerous or precancerous cells.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Colposcopies primarily check for cancer cells or cells that could become cancer if not treated (also called cervical dysplasia). Your provider will look for these cells in your cervix, vagina and external genitals (vulva). Colposcopies can also test for genital warts and noncancerous growths called polyps.
Sometimes, your provider might recommend a colposcopy to evaluate other symptoms like abnormal vaginal bleeding or vulvar itching.
People designated female at birth (DFAB), including cisgender women, transgender men and nonbinary people with vaginas, may need colposcopy to investigate test results that may indicate abnormalities. Your provider may recommend a colposcopy if you:
You shouldn’t worry. The chances are good that you don’t have cancer. And if you do have precancerous cells, they’re not likely to become cancerous while you’re waiting for your appointment. A colposcopy can allow your provider to identify and treat precancer cells early so that you don’t have to worry over a cancer diagnosis.
Your primary care provider or gynecologist can perform a colposcopy. Sometimes, trained specialists called colposcopists perform the procedure. Research suggests that having an experienced medical specialist perform the procedure increases the likelihood that precancerous cells will be caught early.
Colposcopy isn’t surgery, but biopsies are considered minor surgical procedures. Biopsies sometimes happen as part of colposcopy. If your provider finds any abnormalities during your colposcopy, they can remove a sample of the suspicious tissue. It’s a painless procedure that takes less than 30 minutes and doesn’t require a hospital stay.
Colposcopy can take place in a medical office or clinic. The procedure usually lasts from 10 to 20 minutes. You should be able to go home the same day of your procedure.
A colposcopy is usually no more uncomfortable than having a Pap test. You won’t need any anesthesia or pain medicine. Here’s what to expect:
If your colposcopy shows one or more areas of abnormal tissue, your provider can do a biopsy to remove the tissue for testing.
Unlike a Pap test, where tissue from your entire cervix gets scraped, colposcopy allows your provider to take tissue samples by scraping cells from select areas. Small pieces of tissue will be removed and sent to a laboratory to see if cancer or precancer cells are present. You may feel mild pressure or a pinch when your provider removes the abnormal tissue.
A colposcopy is relatively painless. You may feel slight pressure when the speculum enters your vagina. You may feel a slight burning or stinging when the solution comes into contact with your cervix. If you need a biopsy, you may feel a sharp pinch or a sensation like a period cramp when the tissue sample is excised. Taking over-the-counter pain relievers before the exam can help with the pain.
You should be able to resume normal activities immediately following your appointment. If you didn’t have a biopsy, you might notice some spotting for the next two days.
If you had a biopsy, you might experience:
You can use pads to manage any vaginal discharge or bleeding. In the meantime, avoid inserting anything into your vaginal. Allow your cervix time to heal by avoiding penetrative sex, tampons or douching. Ask your provider about how long you should avoid these activities to ensure adequate recovery time.
The results of your colposcopy and biopsy will determine if you need any treatment. About 40% of people receive results that report no sign of abnormal cells. About 60% need treatment of some kind to address an abnormality. Examples of abnormalities include masses on the cervix, vagina or vulva.
Suppose the colposcopy biopsy results reveal early cases of abnormality, like mild cervical dysplasia. In that case, your provider will ask you to repeat the Pap test periodically. Mild dysplasia may go away on its own (tissue returns to normal without treatment). Treatments for more advanced precancer cells include:
In more serious cases, you may need surgery to remove your entire uterus. Ask your provider about any follow-up testing that is needed after surgery.
Biopsy results usually arrive within two to 10 days. Ask your provider about when you should expect results and how key findings will be communicated with you.
Colposcopy is a relatively safe procedure with few side effects. But you should call your provider if you notice any of the following symptoms:
A note from Cleveland Clinic
Learning that you’ll need follow-up testing because you’ve had abnormal test results is scary. Colposcopy is a simple, relatively painless procedure that can give you peace of mind from worry. Colposcopy can help your healthcare provider identify any cancer or precancerous cells early so that you get the treatment you need. Cervical cancer that’s diagnosed and treated early can be cured. Coloscopy can rule out cancer, too. Discuss your concerns about cancer risk and potential outcomes with your provider as you prepare for the day of your exam.
Last reviewed by a Cleveland Clinic medical professional on 05/19/2022.
Learn more about our editorial process.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy