Trigeminal neuralgia is a chronic condition that can cause sudden, intense painful episodes, typically on one particular side of your face, that can disrupt daily activities. Surgical procedures usually only suppress symptoms for a set amount of time, but other forms of medication can help relieve these short, sporadic, very painful episodes.
Trigeminal neuralgia, also referred to as tic douloureaux, is a condition defined by intense facial pain that can disrupt your normal, everyday activities. Activities as simple as chewing, talking, smiling, brushing your teeth or shaving can trigger brief bouts of intense pain. Though these painful episodes are short-lived, the pain can return sporadically (on and off). Or you might also experience constant pain that isn’t as severe.
Typically, trigeminal neuralgia is unilateral (meaning it only affects one side of your face). If it’s bilateral, both sides will be affected, though not at the same time. Bilateral trigeminal neuralgia is also very rare. Interestingly, the right side of the face is usually more affected by this condition than the left.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
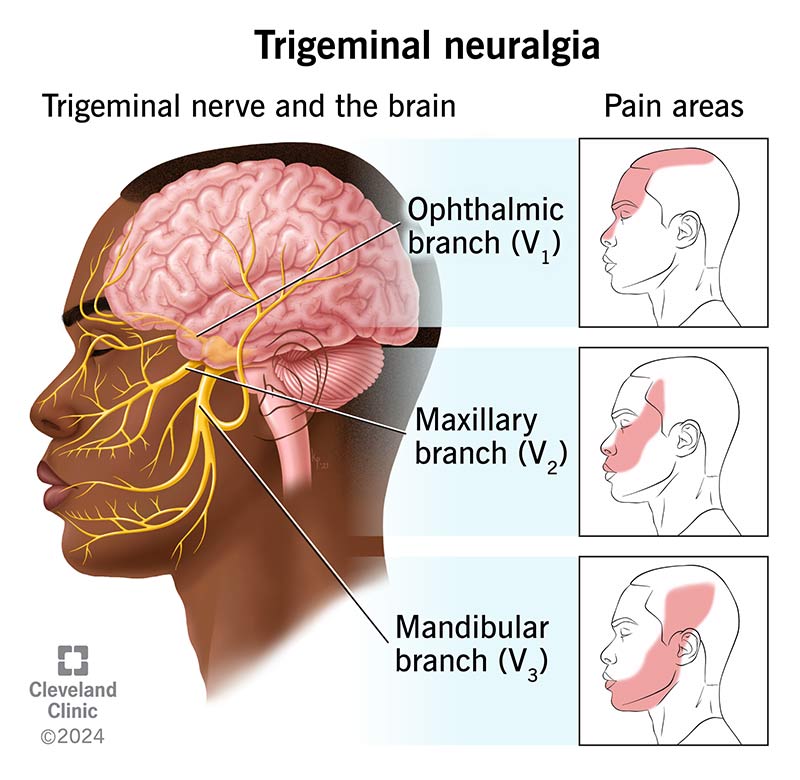
The trigeminal nerve is one of 12 pairs of nerves attached to your brain. It’s responsible for transmitting touch and pain sensations from your face and head to the brain. There are three branches in the trigeminal nerve, all of which are responsible for transmitting nerve impulses to different parts of your face:
There are two main forms of trigeminal neuralgia:
About 150,000 people each year are diagnosed with trigeminal neuralgia. That’s roughly 4.3 new cases per 100,000 people. Trigeminal neuralgia affects people over the age of 50 significantly more than it does people under the age of 40, where it’s considered rare. This condition also affects women more than men and is considered a rare disorder.
About 1 to 2% of people with multiple sclerosis (MS) also have trigeminal neuralgia. MS and trigeminal neuralgia both slowly break down the body’s main protective layer around the nerve (the myelin sheath), which is why there’s a slight overlap. MS patients can also develop trigeminal neuralgia after their MS diagnosis. Similarly, any 40-and-under trigeminal neuralgia patients are considered candidates to develop MS. So, if you fall in this age range, you should consider getting tested for MS.
There are several conditions that may cause trigeminal neuralgia, but it’s typically caused by a blood vessel exerting pressure on the nerve near your brain stem. MS causes the deterioration of the nerve coating called the myelin sheath, so people with MS may also develop TN.
This condition can also be caused by a tumor or lesion that compresses your nerves, though this isn’t nearly as common. If you damage your trigeminal nerve through oral or sinus surgery, a stroke or from facial trauma, you may feel facial nerve pain that’s similar to the symptoms of trigeminal neuralgia.
Some cases of trigeminal neuralgia are idiopathic — meaning no specific cause is identified.
Certain symptoms are contained to the cheek and jaw area, including:
Other symptoms include:
It’s mostly simple activities that require you to move or touch your face that can trigger painful episodes, including:
Your doctor will ask you about your symptoms and medical history, while also performing a physical exam of your head and neck area, including your ears, mouth, teeth and temporomandibular joint (TMJ). They will likely make their diagnosis based on a few different factors:
The doctor may also conduct a neurological exam, which will likely consist of examining how the nerves in your brain and your motor system function, along with assessing your reflexes and pain tolerance.
There are a lot of conditions and disorders where facial pain is the main symptom, so it’s important to rule out these various, other conditions to determine your diagnosis. Conditions that can mimic trigeminal neuralgia include cluster headaches or migraines, post-herpetic neuralgia (pain following an outbreak of shingles) and TMJ disorder. It’s also important to rule out sinusitis and ear infections.
Your doctor may use a magnetic resonance imaging (MRI) scan to rule out brain tumors, MS and other potential causes. The scan can show whether there’s a blood vessel pressing on the nerve that is causing pain.
Unfortunately, trigeminal neuralgia isn’t preventable. But you can prevent painful episodes by avoiding certain activities that cause severe, intense pain. There’s also nothing to suggest that trigeminal neuralgia is brought on by stress.
Trigeminal neuralgia symptoms can be treated with a combination of medications, surgery and complementary therapies.
If you don’t respond to any of these medications or believe your condition is worsening over time, you could be a candidate for surgery. You have several different surgical options. Your doctor will likely recommend one for you based on the severity of your pain, your preference, your physical health, previous surgeries and the surgery’s relative risks and benefits. Additionally, it’s more difficult to perform surgery on those suffering from Type 2 trigeminal neuralgia.
Percutaneous (through the skin) surgical techniques include:
Microvascular decompression is a more invasive surgical procedure. It’s typically the most successful of all these procedures, as it can provide pain relief for up to 10 years (over 70% of patients have seen some sort of relief of their symptoms). The goal of this procedure is to provide a longer-term solution, where the trigeminal nerve can recover and return to a more normal, pain-free state. However, it's invasive because the surgeon must create an opening behind the ear, thus exposing the trigeminal nerve root. This opening reveals the blood vessel that may be compressing the nerve; once your surgeon identifies the specific blood vessel, they place a cushion between the nerve and the blood vessel. Younger patients who are otherwise in good health are suitable candidates for this procedure.
If a surgeon attempts to perform microvascular decompression but doesn’t find a blood vessel actively pressing against the nerve, they may perform a neurectomy. This is a procedure in which the surgeon cuts either part of the nerve near the brain stem or some of the nerve’s branches in the face. A neurectomy can have lasting side effects, including numbness in the areas where the surgeon cut part of the nerve and impaired hearing. Nerves in the face, however, can grow back over time, meaning the pain will return in that specific area as well.
Stereotactic radiosurgery uses Gamma Knife, CyberKnife or LINAC surgery to deliver a highly concentrated amount of radiation on the trigeminal nerve root, where it meets the brain stem. After this procedure, a lesion will form on the nerve that will disrupt its ability to transmit pain signals to the brain, though you may increasingly feel numbness in your face as a result. It can be a few weeks before you begin to see the effects of this procedure. Stereotactic radiosurgery generally eliminates symptoms for about three years.
There are other approaches you can use with drug therapy, including:
Additional therapies that may be helpful include:
It certainly can. At first, the pain may be limited to the jaw area, which leads some with this disorder to think that it’s just a routine dental problem. But over time, the condition can get worse and worse, to the point that the pain-free moments between episodes become shorter and shorter, sometimes until they’re nonexistent. Additionally, the intensity of your pain may increase, making normal activities a burden and forcing you to eliminate simple, everyday tasks from your routine, for fear of an attack. Pain management can also be less effective over time.
A note from Cleveland Clinic
Trigeminal neuralgia isn’t life-threatening but it can be life-altering. You may become afraid of performing certain normal activities, as they can bring on short, intense painful episodes. But, thankfully, there are different surgical procedures and treatment options that can help you live a normal, relatively pain-free life — even if this is a condition that will likely be present, in some way, for your entire life.
You can learn more by taking Cleveland Clinic's Trigeminal Neuralgia Online Risk Assessment.
Last reviewed by a Cleveland Clinic medical professional on 10/25/2021.
Learn more about our editorial process.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy