Two Hearts, One ‘Amazing’ Surgeon
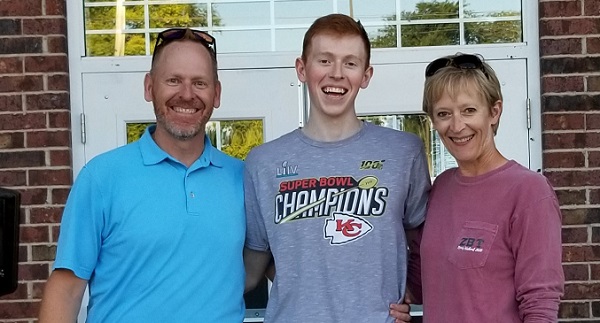
Kathy Chelton and her 19-year-old son, Carter, have a bond that goes beyond family ties: In the past three years, they’ve both had open heart surgery.
Kathy’s came first, nearly four decades after learning she had a heart murmur. Her parents and other close family members also had heart issues.
She lived with the condition until 2017, when it began interfering with daily living. “I was definitely feeling super tired,” Kathy says. “I was only 51, and we’re pretty active. I didn’t want to have to take naps all the time.”
Her cardiologist in Kansas City, Missouri, near where the Cheltons live, gave two recommendations on where to have her mitral valve repaired: one was a local hospital; the other was Cleveland Clinic.
The latter surprised Kathy. “At the time, I’d never heard of it,” she says. “So my husband, Scott, and I, who are both data people, researched Cleveland Clinic. The mortality rates are so low. Why would we not go to the place that does this surgery the most and with the highest rate of success?”
She enjoys describing the confused reaction of other Missourians she knew. “They would look at me rather puzzled. Why are you going to Cleveland? “Because they’re the best,” she’d answer, “and they do this all the time.”
A. Marc Gillinov, MD, Chair of the Department of Thoracic and Cardiovascular Surgery in the Sydell and Arnold Miller Family Heart, Vascular & Thoracic Institute, performed Kathy’s surgery, repairing both her mitral and tricuspid valves. Dr. Gillinov holds the Judith Dion Pyle Chair in Heart Valve Research.
He and the cardiologists at Cleveland Clinic “are all just amazing,” Kathy says. Her husband agrees. “Every heart surgery patient gets the best of care, no matter who you are or where you come from,” Scott says.
So when Carter, then 18, also had to have his mitral valve repaired, the Cheltons immediately knew where to turn.
Connection and gratitude
Carter was a sixth-grader in 2013 when his pediatrician detected a heart murmur. “From that point on, he had follow-up echocardiograms every two years,” Kathy says. “Why his condition progressed so much more rapidly than mine, we will never know, I suppose.” The Cheltons also have a 23-year-old son, Cole, who has not been diagnosed with a heart condition.
By the fall of 2019, Carter had started his freshman year at the University of Kansas and would come back home to Missouri for cardiology appointments. The following January, his cardiologist expressed concern that Carter’s left ventricle was enlarged and suggested he might need surgery. That’s when Kathy had Carter’s records sent to Cleveland Clinic.
From then on, everything happened quickly, she says. Cleveland Clinic worked around Carter’s college schedule and booked his evaluation for the first Monday of spring break. The appointment confirmed the need for surgery.
“All the coronavirus stuff was going on and, of course, we were worried about him,” Kathy says. “But Dr. Gillinov was very reassuring, promising that Carter would be fine and that he would treat him like he would treat his own child.”
Dr. Gillinov performed the operation in June. “What stands out is that the surgeons at the Clinic are so experienced, and so knowledgeable in what they do, that they are literally able to make decisions during surgery as to what is best for the patient,” Kathy says. “Dr. Gillinov told me that he probably spent more time watching Carter ’s echo during his surgery to decide whether or not his tricuspid valve needed repair, which it didn ’t, and then he repaired some chordae, which wasn ’t discussed in his pre-surgery consultation. That is what a high-volume center can offer.”
Carter and his mom not only had the same surgeon, they shared a nurse practitioner, Julia Ehlers, with whom Kathy had made a strong connection during her 2017 hospitalization. “Even though Cleveland Clinic is such a huge place, I feel like it’s a small circle,” Kathy says. “We feel so at home there.”
As a grateful patient, she and her husband have given annually to the heart center and recently made a five-year pledge designated toward Dr. Gillinov’s research fund. They also are planning to make Cleveland Clinic a part of their estate plan.
As for Carter, he decided after his surgery to change his major from aeronautical engineering to pre-med, with the intention of becoming a heart surgeon.
If her surgery had come earlier in her life, she might have done the same, Kathy says. “The two of us have a unique bond. We’ve both been through something. It’s not an inside joke, but we have our little club.”
How You Can Help
Your gift to Cleveland Clinic furthers research that impacts the lives of patients and their families around the world. Give today and support the heart care program ranked No. 1 in the nation for 26 consecutive years by U.S. News & World Report.
Developing the ‘No. 1 Research Center in Florida’
The uncertainty surrounding COVID-19 has highlighted the importance of translational and clinical research and the critical role philanthropy plays in developing vaccines and treatments for the disease caused by SARS-CoV-2, as well as for other infectious threats.
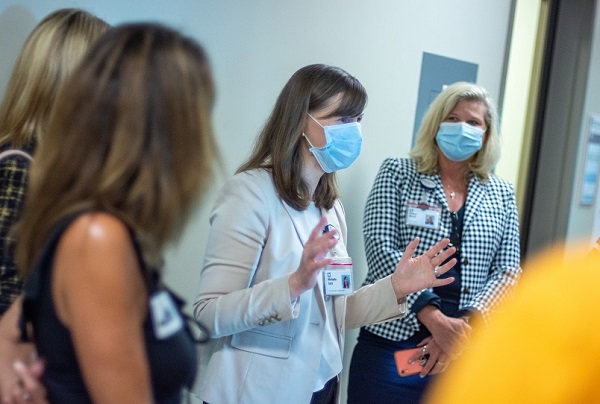
“Donations are vital to the development of the Florida Research and Innovation Center, which we expect will become the number one research center in Florida and ultimately revolutionize therapies for a range of diseases,” says Michaela Gack, PhD, Scientific Director for the Center.
The Center collaborates with the Lerner Research Institute, located on Cleveland Clinic ’s main campus in Ohio, tapping into resources at both facilities to create new treatments for patients around the globe.
“Our focus is on diseases that are of global relevance, and also diseases that primarily affect the Florida region, such as mosquito-transmitted viruses,” Dr. Gack says.
Previously a Professor in the Department of Microbiology at the University of Chicago and Chair of its Committee on Microbiology, Dr. Gack joined Cleveland Clinic Florida in July 2020.
The renowned virologist has an extensive background in molecular virology and infectious disease. Her research focuses on studying the immune response to viruses, an essential step in developing safe and effective antivirals and vaccines. She also has done extensive research on immune evasion mechanisms of dengue, influenza and Zika viruses.
Endowed Chair Propels Research Discoveries
Endowed research positions are enduring gifts to the institution. Each position is permanently paid for with annual revenue generated from an interest-bearing fund in which the principal remains intact. Named chairs are long-standing tributes to the establishers and serve as ways to focus on issues of personal interest and spur advances in those areas.
In July 2020, Dr. Gack was appointed as the inaugural holder of the Arthur and Marylin Levitt Endowed Chair for the Florida Research and Innovation Center.
“The extremely generous funds that established the Arthur and Marylin Levitt Endowed Chair will have a major impact on the Center’s research on a variety of significant viral pathogens, with the ultimate goal of defining novel molecular targets, either in the virus or the human immune system,” Dr. Gack says. “It will facilitate the development of new antiviral therapies, diagnostics, and preventative measures for viral infectious diseases.”
Promising New Research
Since its official opening in July 2020, the Florida Research and Innovation Center has been researching ways to develop new therapies for infectious diseases, cancer, and chronic inflammatory or autoimmune diseases.
- Diseases caused by coronaviruses: Using critical knowledge to identify cellular and viral factors vital for SARS-CoV-2 pathogenesis is leading researchers to understand the mechanism by which coronaviruses cause disease in humans, and to develop novel therapeutic interventions and vaccine strategies against these viruses.
- ‘Ready-to-use’ antiviral treatments: Currently, the main strategy for developing antivirals relies on targeting one virus post-emergence. Projects in the lab are focusing on identifying molecular targets to block multiple viruses, rather than just one. This preemptive approach aims to enhance preparedness in the face of the next viral pandemic by laying the groundwork for developing “ready-to-use” broad-spectrum antiviral therapies.
- Mosquito and tick-borne viral diseases: Emerging viruses, such as mosquito and tick-borne viruses, can quickly cause catastrophic disease outbreaks due to novel changes in the genetics of the virus or introduction to naïve populations. The Center is working to investigate inhibitors targeting the viral life cycle, and to identify novel and conserved characteristics of these viruses that can be clinically targeted to diminish human disease burden.
- Chronic inflammation and autoimmune disorders: Ranging from microbial infections to chronic inflammatory and autoimmune diseases, researchers apply leading-edge technologies to gain a greater understanding of the roles of inflammation-inducing molecules and sensor proteins in disease onset and progression and of the fundamental immunologic principles of these diseases that may aid in developing effective immune-based therapies.
- Virus-induced cancers: An often underestimated yet highly significant contributor to the global cancer burden is virus infection. By improving our understanding of how these viruses infect human cells and induce cancer at the molecular level, the Center is working on identifying novel targets that can be used in the development of effective antiviral and anti-cancer therapeutics.
How You Can Help
Your gift — of any size — is vital to the medical research taking place at the Florida Research and Innovation Center. Donate today to help us continue high-priority research and provide the best care for patients.
Finding a Better Way to Diagnose MS

As many as 1 in every 1,000 people in the U.S. have multiple sclerosis.
Despite extensive research conducted on MS over the past 50 years, we still do not know the cause of this inflammatory disorder of the central nervous system.
But experts agree: There is a need for improved methods for diagnosing MS. Although MRI is a longstanding tool for detecting MS lesions, inaccuracies in diagnosis do happen.
In fact, as many as 1 in 5 people diagnosed with MS is later found not to have the disease.
Now, the National Institutes of Health has awarded $7.2 million to a Cleveland Clinic-led research team to improve the accuracy of MS diagnosis.
The grant will support a multi-center study to evaluate whether a new biomarker (known as the central vein sign, or CVS) can be a reliable diagnostic marker for MS.
“We aim to show that the CVS is a simple and reliable diagnostic biomarker that can be immediately translated into clinical care,” says Daniel Ontaneda, MD, PhD, the study’s co-principal investigator. “These initial exploratory analyses will be important to how readily positive findings about the utility of CVS criteria can impact clinical practice.”
When it comes to diagnosing a patient with MS, timeliness of diagnosis is key. Delays in the diagnosis of relapsing-remitting MS are common and can carry severe and lifelong consequences.
“The ultimate goal is to have the CVS incorporated into the MS diagnostic criteria,” says Dr. Ontaneda.
How You Can Help
Philanthropy is vital to researchers because it helps further investigations that lead to federal funding. Please make a gift today.
WATCH Dr. Ontaneda describe the research in this news clip from NeurologyLive.
Health Education Campus Shines Bright During Debate
On Tuesday, Sept. 29, the Health Education Campus of Case Western Reserve University and Cleveland Clinic took to the national spotlight.
The centerpiece of the facility – the 477,000-square-foot Sheila and Eric Samson Pavilion – served as center stage for the first of four 2020 general election debates.
Watch a time-lapse video of the building’s transformation here.
Millions who tuned in saw both the Health Education Campus and the city of Cleveland on display as a destination for higher learning and exceptional medical care.
“The symbolic nature of holding the first presidential debate of 2020 on the campus is remarkable,” says Tom Mihaljevic, MD, Cleveland Clinic CEO and President. “Debates are vital to a functioning democracy. Serving as host is both a tremendous honor and an opportunity. We are in an unprecedented time in American history and healthcare is at the center of public discourse; the pace of scientific discovery is on everyone’s mind.”
The Health Education Campus, which opened in 2019, is located on Cleveland Clinic’s main campus and was established through a joint partnership between Case Western Reserve University and Cleveland Clinic that began in 2013.
Funded primarily through philanthropic gifts and designed by London architects Foster + Partners, the 11-acre campus was envisioned as a way to encourage interaction among future healthcare professionals in and out of the classroom. Students at the Health Education Campus learn the fundamentals of team-based care while also practicing skills together in simulated settings and actual clinical sites.
“The campus serves a noble purpose of educating future caregivers to fulfill our mission and advance scientific discovery,” says Dr. Mihaljevic. “To have the presidential candidates discuss important issues in our innovative learning space represents a tremendous opportunity for both institutions — and our entire Northeast Ohio region.”
The event was sponsored and produced by theCommission on Presidential Debates, a nonprofit, nonpartisan organization that has sponsored all general election presidential and vice presidential debates since 1988.
Going forward, Cleveland Clinic will continue to serve as Health Security Advisor to the Commission on Presidential Debates, which also will stage presidential debates in Miami and Nashville as well as the vice presidential debate in Salt Lake City.
Promising Alzheimer’s Research Awarded NIH Grant

The National Institute on Aging (NIA), part of the National Institutes of Health, has awarded Dianne Perez, PhD, a five-year, $2 million grant to continue her work to develop a novel treatment for Alzheimer’s disease.
Dr. Perez, a staff member in the Department of Cardiovascular & Metabolic Sciences, has spent the last 30 years researching and developing a compound for cardiac ischemia that, in the last few years especially, has also shown great promise in improving cognition, learning and memory.
Despite having spent the majority of her career studying vascular diseases, she knew she could not overlook the cognitive benefits of the compound, which the team has come to informally call “compound 3.” The Alzheimer’s Drug Discovery Foundation (ADDF) and the Harrington Discovery Institute at University Hospitals together awarded Dr. Perez the ADDF-Harrington Scholar Award, which enabled her and her team to start testing compound 3 in preclinical models of Alzheimer’s disease.
The results of their investigations have been promising, Dr. Perez says, but this next phase of study, made possible by the support from NIA, will allow the team to further refine compound 3 and perform more dose and efficacy testing.
“We want to enhance some of compound 3’s chemical properties to increase its brain penetrance—or how much of the drug is able to effectively cross the blood-brain barrier,” she explains. “We also want to test the drug’s effectiveness, including at difference doses, in a more diverse model of Alzheimer’s disease.”
The pathology of Alzheimer’s disease is notoriously heterogeneous; it is one of the leading reasons an effective treatment has remained elusive. To date, Dr. Perez’s preclinical studies have made use of amyloid-based models. While plaques of beta-amyloid proteins are a hallmark feature of Alzheimer’s brains, there are other important brain changes seen in patients that should be reflected in preclinical models. Dr. Perez says that using different disease models will help broaden how their findings can be interpreted.
Compound 3: The Basics and the Benefits
Dr. Perez’s original research focused on understanding the structure and function of a class of molecules called G-protein coupled receptors—specifically a type called α1-adrenergic receptors, which bind to the neurotransmitter norepinephrine and the neurohormone epinephrine. Epinephrine causes blood vessels to narrow, which increases blood pressure and adapts the heart to withstand damage, making it a viable treatment strategy for ischemia (where reduced blood flow causes a shortage of oxygen to the heart). For this reason, she set out to develop a drug that could imitate and amplify norepinephrine/epinephrine-receptor binding (these types of drugs are called agonists).
There are several subtypes of α1-adrenergic receptors. Dr. Perez discovered that overexpressing α1A receptors had profound cardio- and neuroprotective effects. Preclinical models with increased receptors of this type had reduced risk of ischemia and cancer, lived 10-15% longer and showed signs of improved cognition. They exhibited enhanced learning and memory, as well as increased neurogenesis and synaptic plasticity (formation of new neurons and connections between neurons).
“This is where we saw a real potential for an α1A agonist as a potential Alzheimer’s treatment,” Dr. Perez says. “But the problem was that α1A agonists have been shown to have harmful effects on blood pressure. If we were going to pursue this as a therapeutic approach for Alzheimer’s disease, we knew we needed to find a way to maintain the cognitive benefits without inadvertently raising blood pressure.”
The solution, Dr. Perez found, was to design compound 3 to be an agonist-like compound. Compound 3 still binds norepinephrine and epinephrine to α1-adrenergic receptors, but at a different site than normal.
So far, Dr. Perez has seen positive results from this chemical sleight of hand. Although compound 3 has taken on new life—pivoting from being used to potentially treat cardiac ischemia to now Alzheimer’s disease—Dr. Perez credits this success to the decades she has spent studying α1-adrenergic receptors and her background in chemistry. She received her PhD in chemistry from the California Institute of Technology.
In her most recent preclinical study, which was supported by the BrightFocus Foundation and the ADDF-Harrington Scholar Award, Dr. Perez and her team found that compound 3 significantly increased long term potentiation—an indicator of how strong the brain’s neuronal synapses in memory formation are—and cognitive behavior in models of Alzheimer’s disease without blood pressure changes.
Looking Forward
“This phase of drug development can be difficult and expensive, and projects with early momentum often stall without external support,” says Dr. Perez, “so we are very excited to continue our work with this support from NIA. There are millions of Americans living with Alzheimer’s and we want to help bring them and their families an effective treatment. More research will be necessary, but we are eager at this phase to optimize compound 3 to the best of our ability.”
Future studies to refine compound 3’s properties will be done in collaboration with Shaun Stauffer, PhD, who directs Cleveland Clinic’s Center for Therapeutics Discovery and whose expertise in medicinal chemistry will help with drug optimization.
How You Can Help
Philanthropy helps fund new ideas and exploratory research that helps scientists at Cleveland Clinic gain federal funding to further promising investigations. Please make a gift today.
Register Today for Virtual Medical Innovation Summit

For the first time in its history, Cleveland Clinic’s Medical Innovation Summit will be held virtually on Tuesday, Oct. 6, and complimentary registration will allow participants from around the globe to join the annual event.
The Medical Innovation Summit is where influential investors, entrepreneurs, clinicians and industry professionals collaborate dynamically to drive healthcare change according to its most pressing priorities, including the growing need to make healthcare practice more efficient, transparent, value-based and connected. Today’s world needs fast, innovative solutions to help battle rising drug prices, keep healthcare data safe and combat the COVID-19 pandemic.
The summit will cap off with the reveal of the annual Top 10 Medical Innovations list. A team of leading physicians and researchers will announce the up-and-coming technologies expected to have the greatest impact on healthcare in the coming year.
Now in its 18th year, the Medical Innovation Summit is organized by Cleveland Clinic Innovations, the development and commercialization arm of Cleveland Clinic.
“Innovation is a core value at Cleveland Clinic that has transformed how we deliver care and inspired the Medical Innovation Summit,” said Will Morris, MD, Executive Medical Director of Cleveland Clinic Innovations. “The summit brings together leaders from a variety of industries to share their expertise and best ideas to promote the evolution of healthcare.”
Highlights of the agenda include a panel of top hospital CEOs addressing the importance of provider collaboration during the COVID-19 pandemic. The panel includes Tom Mihaljevic, MD, CEO and President of Cleveland Clinic; Gianrico Farrugia, MD, President and CEO of Mayo Clinic; and Anne Klibanski, MD, President and CEO of Mass General Brigham.
Registration for the summit is now open. Visit the Medical Innovation Summit website to register and learn more.

