Head & Neck Institute Outcomes
Voice Center
Evaluation of Breathing Pattern Disorder in Athletes With Exercise-Induced Laryngeal Obstruction
Shortness of breath/dyspnea is a key symptom in patients with exercise-induced laryngeal obstruction (EILO), also known as vocal cord dysfunction or paradoxical vocal fold motion. EILO is often misdiagnosed as asthma, and asthma treatments are ineffective in improving symptoms that negatively impact the patient’s quality of life. A common comorbidity of asthma is a condition called dysfunctional breathing or breathing pattern disorder (BPD). This is an abnormal biomechanical pattern of respiration caused by functional or structural factors. A key symptom of BPD is shortness of breath on exertion. The presence of dysfunctional breathing is reported to be as high as 29% in individuals with asthma. However, the presence of BPD in athletes with EILO is unknown. Moreover, the current clinical tools for evaluation of dysfunctional breathing pattern such as the Brompton Breathing Pattern Assessment Tool, the Manual Assessment of Respiratory Motion, or the Hi-Lo assessment are limiting in the athlete population, since they only evaluate patients in low ventilatory output tasks of rest breathing.
To determine the prevalence of BPD in athletes, a total of 77 athletes referred to Cleveland Clinic for suspected EILO and 58 athletes without any respiratory difficulty were evaluated. Patients completed the Dyspnea Index, underwent a laryngeal videoendoscopic provocation test, and performed high ventilatory output tasks of heavy breathing.
A novel rating instrument, the Milstein-Breathing Pattern Assessment Index( M-BPAI) was developed specifically to investigate BPD in this patient population. It incorporates several patterns of respiration that are unique to this assessment and are not included in any other BPD instrument. It comprises 6 items on a predefined scale: (1) relative distribution of breathing motion (chest expansion), (2) anterior abdominal displacement, (3) recruitment of accessory muscles of the shoulders, (4) recruitment of the accessory muscles of the neck, (5) backward tilt of the head, and (6) presence of audible stridor. This rating instrument is easy to administer and can be readily used in a rapid manner in any clinical setting.
Results showed that 78% of EILO patients had evidence of BPD, confirming that it is highly prevalent in this population. The overall M-BPAI score was significantly larger in the patient group compared with the control group. The patient group also had significantly higher values of subscale items of shoulder displacement, head tilt, strap muscle contraction, and audible inhalation compared with the control group.
The M-BPAI rating instrument has the potential to be a valuable diagnostic marker for identifying BPD in patients with exercise induced shortness of breath. Results can also help direct the respiratory retraining therapeutic intervention for symptom control.
Overall M-BPAI Score in Athletes Without any Breathing Difficulties (Control Group) and in Athletes Referred With Exercise-Induced Laryngeal Obstruction (Patient Group)
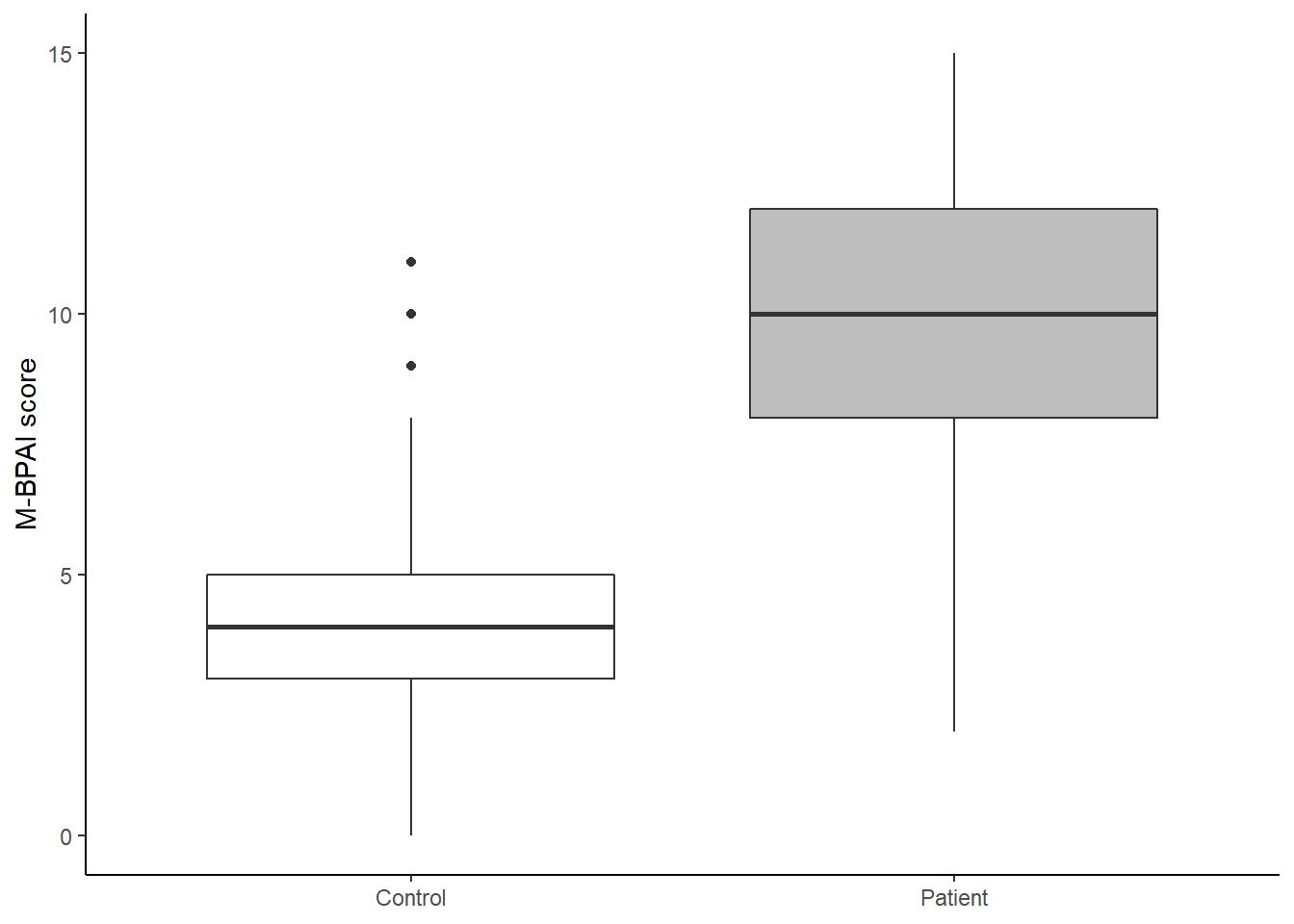
M-BPAI = Milstein-Breathing Pattern Assessment Index
