What is a Stroke?
Each year, nearly 800,000 Americans have a new or recurrent stroke, which is the nation’s fourth leading cause of death and a leading cause of serious long-term disability, according to the American Heart Association and American Stroke Association.
A stroke, or “brain attack,” occurs when the blood supply is cut off from part of the brain. When this happens, the blood-deprived brain loses its supply of oxygen and nutrients. When the brain is deprived of blood for even a few minutes, it begins to die.
There are two types of stroke — ischemic and hemorrhagic.
In ischemic strokes, brain arteries become blocked and prevent blood from nourishing the brain. In hemorrhagic strokes, brain arteries rupture from damage caused by high blood pressure and other risk factors or an aneurysm (an abnormal out-pouching of a blood vessel). This causes blood to flood the brain, creating pressure that leads to brain-cell death.
Strokes do occur in young patients, and pediatric stroke requires highly specialized care. We maintain a dedicated pediatric stroke program for the evaluation and management of childhood stroke from birth to age 18. We are also part of the International Pediatric Stroke Study group, actively participating in pediatric stroke clinical trials and data collection. Our pediatric neurology team works closely with pediatricians and pediatric specialists at Cleveland Clinic Children’s, offering advanced medical care and rehabilitation services.
Remember that for every minute brain cells are deprived of oxygen during a stroke, brain damage increases. The chances for survival and recovery improve when treatment begins within the first few hours of stroke warning signs.
Immediate treatment of a stroke may limit or prevent brain damage. A thrombolytic agent or “clot buster” medication may be given within the first three hours of the onset of stroke symptoms. Hence, it is critical to get to the hospital quickly if you experience stroke symptoms. The fastest way is to call 9-1-1.
Risk Factors
What are the Risk Factors for a Stroke?
If your primary care physician has diagnosed you as being at risk for a stroke, a Cleveland Clinic stroke neurologist can help determine your best course of treatment.
Many factors increase the risk for stroke. Some factors can be controlled; others cannot.
- Family history: Those who have a family history of strokes or a prior stroke are at higher risk for having a stroke.
- High blood pressure: Strokes are four to six times more likely to occur in people with high blood pressure.
- High cholesterol: People with high cholesterol are at double the risk of having a stroke.
- Heart disease: Strokes are six times more likely to occur in people with heart disease.
- Excess weight: Being overweight can lead to heart disease and high cholesterol, which, in turn, increase chances of having a stroke.
- Alcohol use: Heavy drinking increases the risk for stroke.
- Tobacco use: Smokers have double the risk for stroke as nonsmokers.
- Gender: Approximately 55,000 more women than men have a stroke each year.
- Race: African-Americans have a higher rate of stroke than other races.
- Age: After age 65, there is an increased likelihood of stroke.
- Chronic disease: Diabetics are at higher risk for stroke.
How can I reduce my risk?
- Control your blood pressure.
- Find out if you have heart disease, especially an irregular heartbeat known as atrial fibrillation (AF).
- Don’t smoke.
- Find out if you have a diseased carotid artery (arteries that provide blood flow to the head).
- Lower your cholesterol.
- Limit your alcohol intake.
- Control your weight.
- If you have diabetes, manage the disease.
Warning Signs
Many warning signs indicate you may be suffering a stroke. Depending on the function of the part of the brain affected, the person suffering the stroke suddenly may become paralyzed, blind or unable to speak.
It is crucial to get to a hospital immediately. If you experience any of these major stroke warning signs, call 9-1-1:
- Sudden loss of speech
- Slurred speech
- Sudden loss of vision
- Blurry or double vision
- Sudden paralysis
- Sudden weakness
- Sudden dizziness
- Sudden, severe headache, often accompanied by neck stiffness and vomiting
For patients with risk factors, medications for blood pressure, diabetes and high cholesterol are important preventive measures. Smoking must stop. A person who has had transient ischemic attacks (also known as TIAs or ministrokes) or a stroke may be treated with aspirin or other antiplatelet or anticoagulant medications to reduce the risk of another attack. A type of surgery called carotid endarterectomy is sometimes recommended to reduce the risk of a major stroke. In this procedure, the fatty deposits in the carotid artery that block blood flow to the brain are removed. Nonsurgical options for opening blocked carotid arteries include angioplasty and stenting.
Treatments

Our highly trained, diverse team of board-certified specialists and sub-specialists collaborates to provide comprehensive care for stroke patients. That team includes:
- Vascular Neurologists
- Cerebrovascular and endovascular neurosurgeons
- Interventional neuroradiologists with training in neurosurgery,
- Radiology and neurology
- Neurointensivists (physicians specially trained in neurocritical care)
- Pediatric stroke neurologists
- Neuroanesthesiologists
- Stroke rehabilitation specialists
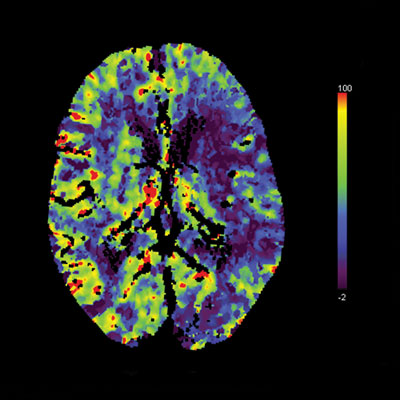
As indicated by our national awards and certifications, Cleveland Clinic’s Cerebrovascular Center has a rigorous stroke care protocol that meets or exceeds national standards and guidelines that improve outcomes. Diagnostic tools such as brain image scans help guide treatment, and neurologists conduct fast but thorough patient evaluations. Further, Cleveland Clinic has been recognized for its fast “door-to-needle” time – the time from arrival at the hospital to administration of intravenous therapies. This timing is recognized as crucial in stroke treatment. Cleveland Clinic’s Neurological Intensive Care Unit (ICU) is staffed 24/7 by a team of critical care neurologists.
For pediatric stroke patients, we offer a dedicated pediatric ICU staffed full time by experienced pediatric intensivists and pediatric neurologists. At our Neurovascular Ultrasound Laboratory, we perform advanced diagnostic examinations to detect abnormalities in the circulation of blood through the brain. This aids in assessing why a patient has suffered a stroke or transient ischemic attack (TIA) and helps determine the best therapies.
Rehabilitation

Rehabilitation for Adults
In collaboration with the Neurological Institute’s Department of Physical Medicine and Rehabilitation, we offer a full spectrum of rehabilitation services designed to return stroke patients to the best possible quality of life.
Our continuum of care spans all phases of the rehabilitative process, from hospital to home. Our multidisciplinary team of rehabilitation specialists includes physiatrists, neurologists, rehabilitation nurses, physical and occupational therapists, speech and language pathologists, psychologists, social workers, recreational therapists and case managers.
These professionals help patients with cognition, mobility, communication, self-care and more. Rehabilitation begins at the inpatient stage and continues on an outpatient basis, including support from Cleveland Clinic Home Care Services, if needed.
Rehabilitation for Children and Teens
After a stroke, pediatric patients are offered comprehensive rehabilitation services at Cleveland Clinic Children’s Hospital for Rehabilitation. Our family-centered pediatric rehabilitation program is accredited by the Commission on Accreditation for Rehabilitation Facilities (CARF), demonstrating our commitment to providing the highest quality services.
Our inpatient rehabilitation program tailors treatment to meet the physical and psychological needs of each child, while preparing the parents to successfully manage their child at home. Our team of rehabilitation medicine specialists, physical therapists, speech therapists, occupational therapists, psychologists, social workers and school reentry specialists work together toward a goal of transitioning the child home and back into school and normal activities. A hospital-based school program ensures the child does not fall behind on schoolwork while hospitalized.
Families are considered an important part of the care team and are involved in every aspect of rehabilitation. Parents participate in daily evaluations and meet with the care team weekly. Parents may stay at the hospital with their child, if they choose: Virtual education sessions and virtual visits are offered for parents who cannot.
Research & Clinical Trials
Lerner Research Institute, the basic science research arm of Cleveland Clinic, houses 36 scientists working on neurologically based research projects. Ongoing cerebrovascular research includes several stroke-related studies such as:
- Subcortical stimulation for rehabilitation of motor deficits following stroke
- Delivery of antioxidant enzymes in cerebral stroke
- Cognitive training that may enhance motor function in stroke patients
- Functional and anatomical adaptations of the brain after stroke and as a result of medical rehabilitation
The Cerebrovascular Center has led several major international trials of stroke medications, including the first-ever trial of intra-arterial thrombolysis in acute stroke. Our patients have the opportunity to participate in other leading-edge clinical research trials, such as:
- An investigation of insulin resistance intervention after stroke
- A study of stenting and aggressive medical management for preventing recurrent stroke
- An evaluation of mechanical retrieval and recanalization of stroke clots using a surgical technique called embolectomy
- A trial of stenting devices for symptomatic ischemic stroke
Patients also may qualify to participate in studies investigating possible genetic links to the development of brain aneurysms.
To learn more about our clinical trials, call Amy Richmond at 216.444.9524.
FAQ's
Q: Is the neurologist/neurosurgeon
fellowship trained?
A. Our stroke neurologists and cerebrovascular and
endovascular neurosurgeons are fellowship trained.
Their areas of expertise combine research, education
and clinical practice to provide innovative and
scientifically based treatments for cerebrovascular
disease with the highest quality patient care.
Q: Do you work within a multidisciplinary team?
A. The Cerebrovascular Center at Cleveland Clinic
understands the importance of tailoring therapy for each
patient. By bringing together physicians from different
training backgrounds and experiences, we offer a
collaborative, multidisciplinary environment to meet the
needs of patients suffering from cerebrovascular disorders.
This unique disease-centered approach allows us to
approach each patient with a consensus plan, benefiting
from a variety of expert perspectives including:
- Board-certified vascular neurologists
- Board-certified cerebrovascular and endovascular neurosurgeons
- Interventional neuroradiologists with training in neurosurgery, radiology and neurology
- Neurointensivists
- Neuro-anesthesiologists
- Stroke prevention and rehabilitation specialists
Q: How many cerebrovascular cases does the
surgeon treat each year?
A. Our Cerebrovascular Center team completed more
than 1,000 surgical/interventional procedures last year
with 1,499 admissions and 4,219 outpatient visits.
Q: Will I be cared for in a dedicated NICU
(Neurological Intensive Care Unit) with
neurointensivists present in the unit 24/7?
A. Within our 22-bed, state-of-the-art dedicated
Neurointensive Care Unit (NICU), we treat more than
1,300 patients per year, with 24/7 coverage. This full
service NICU is equipped to treat any patient with
neurological injury, regardless of the severity. The NICU
also is equipped to handle any heart, lung and gastrointestinal
problems that may arise in neurological
patients. In addition, we have specialized equipment
specifically for the treatment of patients with neurological
illnesses, including inside-the-brain oxygen sensors
and blood flow monitors, and portable head Computed
Tomography (CT) scanning.
Q: What is the average length of stay?
A. The length of your stay in the hospital is one indication
of how good the entire care team, from physicians to
nurses and others, are in expediting your recovery and
return to home. At the Cleveland Clinic Cerebrovascular
Center, we have achieved and maintained average
lengths of stay for our patients consistently below
national benchmarks for four years in a row. The
expected length of stay in the hospital will vary based
on your particular condition and treatment, but at the
Cerebrovascular Center many treatments can now be
done without a single night spent in the hospital.
Q: What are your mortality rates?
A. Cleveland Clinic Cerebrovascular Center mortality
rates have remained well below the national averages
for several years. This results from our patients having
access to the highest levels of specialty care and the
resources available to respond to patient needs 24
hours per day. Make sure the physician you select has
extensive experience treating your condition and has a
multidisciplinary team. Experience counts and good
outcomes similar to the Cerebrovascular Center depend
on a team approach.
Patient Services
Critical Care Transport
If you or someone in your family is having a stroke, expedited transport is crucial. Cleveland Clinic’s critical care transport team is available 24 hours a day to transport patients to our facility from anywhere in the world. Our fleet consists of mobile ICU vehicles, helicopters and fixed-wing aircraft.
Specialty care teams of physicians, nurse practitioners, critical care nurses, paramedics and allied health professionals provide customized care, including pediatric care for infants, children, teens and young adults. In transit, these teams can communicate with your primary care physician or any doctor who has been treating you.
Appointments & Locations
Make an Appointment
To schedule an appointment with a stroke specialist in:
- Akron, Ohio - call 330.344.8523.
- Cleveland, Ohio - call 216.636.5860.
Virtual Visits
Whether you're a new or existing patient, you can get an initial evaluation or follow-up care from a stroke specialist using your phone, tablet or computer. This means there's no travel or parking, less waiting and significant time savings. Call 216.636.5860 to schedule a virtual visit for you or a loved one and get details on cost and set-up instructions.
Cleveland Clinic Stroke Centers
At Cleveland Clinic, our Joint Commission Certified Comprehensive Stroke Center at our main campus serves as the hub in an integrated stroke care network. Cleveland Clinic's health system boasts an additional three Thrombectomy-Capable Stroke Centers, seven Primary Stroke Centers and one regional hospital (Lutheran Hospital) capable of initiating acute stroke treatment. Joint Commission designated hospitals include:
Thrombectomy-Capable Stroke Centers - Ohio
Thrombectomy-Capable Stroke Centers - Florida
Primary Stroke Centers - Ohio
- Ashtabula County Medical Center
- Avon Hospital
- Euclid Hospital
- Marymount Hospital
- Medina Hospital
- Mercy Hospital
- South Pointe Hospital
- Union Hospital
Primary Stroke Centers - Florida
Virtual Second Opinion
If you cannot travel to Cleveland Clinic, help is available. You can connect with Cleveland Clinic specialists from any location in the world via a phone, tablet, or computer, eliminating the burden of travel time and other obstacles. If you’re facing a significant medical condition or treatment such as surgery, this program provides virtual access to a Cleveland Clinic physician who will review the diagnosis and treatment plan. Following a comprehensive evaluation of medical records and labs, you’ll receive an educational second opinion from an expert in their medical condition covering diagnosis, treatment options or alternatives as well as recommendations regarding future therapeutic considerations. You’ll also have the unique opportunity to speak with the physician expert directly to address questions or concerns.
Why Choose Us?
Cleveland Clinic is a nonprofit multispecialty academic medical center. Founded in 1921, it is dedicated to providing quality specialized care and includes an outpatient clinic, a hospital with more than 1,300 staffed beds, an education institute and a research institute.
One of 26 institutes at Cleveland Clinic, the multidisciplinary Neurological Institute is committed to improving outcomes while treating patients with compassion and respect. By bringing together physicians from different training backgrounds and experiences, the Institute’s Cerebrovascular Center offers a collaborative, multidisciplinary environment to meet the needs of patients suffering from cerebrovascular disorders. This unique disease-centered approach allows individualized care for each patient, bringing together a variety of expert perspectives, including:
- Board-certified vascular and interventional neurologists
- Board-certified cerebrovascular and endovascular neurosurgeons
- Board-certified interventional neuroradiologists
- Board-certified neurointensivists
- Stroke prevention and rehabilitation specialists
- Pediatric stroke neurologists
Cerebrovascular Center patients are seen at our main campus in Cleveland and at locations throughout Northeast Ohio and at our Cleveland Clinic Florida locations.
In addition to strokes, the Cerebrovascular Center provides treatment for brain aneurysms, brain and spinal vascular malformations, carotid stenosis, intracranial atherosclerosis and other cerebrovascular conditions. If you or someone you know has a cerebrovascular disorder, please do not hesitate to contact us.