Cleveland Clinic’s one of few nationwide

By Apostolos Kontzias, MD
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 19-year-old patient presented at Cleveland Clinic’s Clinic for Adult Autoinflammatory Diseases with a number of ongoing symptoms. At age three, she began experiencing almost daily fevers of about 104 degrees for about a week that were accompanied by sharp abdominal pain and lymphadenopathy. She would refuse to eat during the episodes and consequently missed many developmental milestones. Her pediatrician, whom she saw frequently, ascribed her fevers to recurrent infection. Her febrile episodes decreased starting at age 10 but she continued to miss many school days and was a sickly child. At about age 14 she began having increasing joint pain and a limp, and was unable to keep up with her peers.
We saw her during a flare at the age of 17, and tested her IgD levels, which were high. We referred her to genetic counseling and she tested positive for a mevalonate kinase (MVK) gene mutation, known to cause hyperimmunoglobulin D syndrome. In fact, her symptoms were classic for the disorder as they were triggered by viral infections and certain vaccines.
After an initial course of injectable anakinra that produced undesirable side effects, we transitioned her to canakinumab. Three months later, she continues to do very well, her symptoms have resolved, she has no abdominal pain, no signs of arthritis and is active again.
Since autoinflammatory disorders were first described nearly 20 years ago, the causes of these confounding syndromes have remained a mystery. Autoinflammatory syndromes remain rare, but they can be debilitating. The potential for serious sequelae, particularly amyloidosis, makes early diagnosis crucial. At the same time, intermittent and confounding symptoms make this a difficult goal to achieve. Nimble scheduling that permits seeing a patient in the midst of a flare-up is often difficult. As a result, patients typically experience a delay in diagnosis that averages seven to 10 years, as depicted in this case study. Also, while genetic variants are clearly involved in the development of these syndromes, environmental factors ranging from menstruation to infection can trigger flares. All of these factors contribute to the diagnostic conundrum autoinflammatory disease poses.
As advances in genomic medicine improve the diagnosis of autoinflammatory disease and help us recognize new disorders in this class, the need for coordinated care intensifies.
Patients clearly benefit from a multidisciplinary, specialized approach that helps solve diagnostic puzzles and addresses the wide-ranging and often debilitating symptoms that accompany these syndromes. An experienced care team includes rheumatologists, pediatric rheumatologists, geneticists and genetic counselors, dermatologists, gastroenterologists, immunodeficiency experts, ophthalmologists, otolaryngologists, and psychologists.
Easy access to the team is vitally important at the outset with scheduling that can accommodate same-day or near same-day appointments. Later, it is important to offer convenient, coordinated appointments that allow patients and family members to see a number of specialists on the same day.
Very few dedicated autoinflammatory clinics exist across the country, including our Clinic for Adult Autoinflammatory Diseases. We work closely with our Genomic Institute to offer genetic counseling for patients and families, as well as referral to other specialists and subspecialists.
We have created an autoinflammatory disease registry to record results and data, including genetic testing, and answers from patient questionnaires concerning family history and symptom triggers.
The database is helping us study these diseases in a systematic way. We hope this will lead to fruitful collaboration with other institutions to advance science and improve clinical care.
The diagnosis of autoinflammatory conditions, a group of ever-expanding disorders, requires a high level of suspicion. If a patient presents with symptoms that fail to fit known conditions, clinicians should consider an autoinflammatory syndrome and a referral to a clinic with experience and expertise in this area.

Consider secondary syphilis in the differential of annular lesions

Persistent rectal pain leads to diffuse pustules

Techniques are borrowed from rhinoplasty, malar augmentation and others

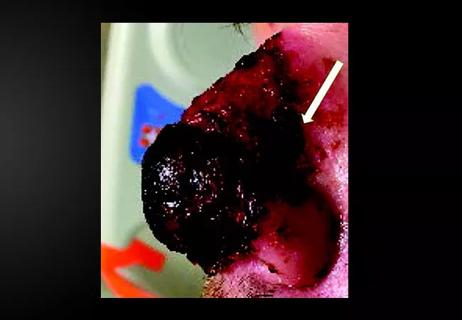
Two cases — both tremendously different in their level of complexity — illustrate the core principles of nasal reconstruction
Stress and immunosuppression can trigger reactivation of latent virus

Low-dose, monitored prescription therapy demonstrates success

Antioxidants, barrier-enhancing agents can improve thinning hair